Abstract
The ability of regional data from whole body scans to provide an accurate assessment of site-specific BMD, osteoporosis prevalence and fracture risk has not been fully explored. To address these issues, we measured total body (TBBD) and site-specific BMD in an age-stratified population sample of 351 women (21–93 years) and 348 men (22–90 years). We found an excellent correlation between AP lumbar spine and total body lumbar spine subregion BMD (r 2=0.92), but weaker ones for total hip compared to pelvis region (r 2=0.72) or between total wrist and left arm subregion from the whole body scan (r 2=0.83). The error in estimating site-specific BMD from total body regions ranged from 4.3% (lumbar spine) to 11.2% (femoral neck) in women and from 4.9 to 11.1%, respectively, in men. Site-specific versus regional measurements at the lumbar spine and total hip/pelvis provided comparable overall estimates of osteoporosis prevalence, but disagreed on the status of individuals; measurements at whole body regions underestimated osteoporosis as assessed at the femoral neck or total wrist. All measurements were associated with a history of various fractures [age adjusted odds ratios (OR), 1.3 to 2.1 in women and 1.2 to 1.5 in men] and were generally interchangeable, but femoral neck BMD provided the best estimate of osteoporotic fracture risk in women (OR, 2.9; 95% CI, 1.7–5.0). Although there are strong correlations between BMD from dedicated scans of the hip, spine and distal forearm and corresponding regions on the whole body scan, the measurements provide somewhat different estimates of osteoporosis prevalence and fracture risk.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
After making bone mineral density (BMD) measurements by dedicated dual-energy X-ray absorptiometry (DXA) scans at the proximal femur in its third cycle, the National Health and Nutrition Examination Survey (NHANES) switched to total body bone density (TBBD) measurements beginning in 1999. Whole body scans will provide important new data on body composition in the United States, and they also offer the possibility of assessing the prevalence of osteoporosis at other skeletal sites (e.g., the spine), but the implications of changing from dedicated site-specific scans to dependence upon TBBD have not been fully explored. For example, it has been shown that bone density values from particular regions of the DXA whole body scan correlate fairly well with those from corresponding site-specific scans [1, 2, 3, 4, 5, 6, 7], but the established international reference standard for hip densitometry is now based on proximal femur BMD data from NHANES III [8]. Moreover, hip BMD data from NHANES III have been used to judge the frequency of osteoporosis in the United States [9], and the influence of changing methodology on overall estimates of osteoporosis prevalence is unclear. Finally, in contrast to the extensive evaluation of dedicated DXA scans [10], the ability of TBBD measurements to predict fracture risk [11] or response to treatment has hardly been studied. To address these issues, we evaluated TBBD, along with site-specific measurements from dedicated scans at the hip, spine and distal forearm, in women and men recruited from an age-stratified random sample of Rochester, Minn., residents [12]. The purpose of this report is to compare these results with respect to BMD values, estimated osteoporosis prevalence and fracture risk assessment.
Subjects and methods
Study subjects
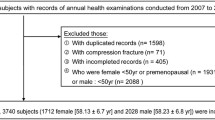
Following approval by the Mayo Clinic’s Institutional Review Board, subjects were recruited from an age-stratified random sample of Rochester residents that was selected using the medical records linkage system of the Rochester Epidemiology Project [13]. The majority of the local populace is attended at the Mayo Clinic in any 3-year period, so the enumerated population (Rochester women seen in 1990±1 year and men seen in 1991±1 year) approximates the underlying population of the community. Of 899 eligible men, 348 (39%) participated and provided full study data [12]. There were approximately 50 men per decade of age from 20–29 years to 80 years and over (mean age ± SD, 55.4±19.6 years; range, 22 to 90 years). Of 812 eligible women aged 20 years and over, 351 (43%) participated. There were approximately 50 women per decade of age, and the subjects included 138 premenopausal (35.0±8.6 years; range, 21 to 54 years) and 213 postmenopausal (67.8±13.2 years; range, 34 to 93 years) women.
Bone densitometry
Areal BMD (g/cm2) was determined for the total body (and subregions), lumbar spine [L2-L4 in anteroposterior projection (AP)], proximal femur (total and subregions) and forearm (total and subregions) by DXA using the QDR 2000 instrument (Hologic, Waltham, Mass.), with coefficients of variation of 0.8, 0.6, 1.8 and 0.8%, respectively, for total body, AP spine, total hip and total forearm BMD measurements by fan beam. Bone density at each site was categorized as osteoporotic or not according to World Health Organization (WHO) criteria [14]. Young normal means and SDs, including those for TBBD, were derived from the 50 Rochester women and 48 Rochester men who were 20–29 years of age at baseline, and all analyses were based on these sex-specific reference values.
Fracture ascertainment
Subjects were interviewed with a standard protocol to collect clinical data, including a history of fractures that was verified by review of each subject’s complete (inpatient and outpatient) medical records in the community [13]. The interview and record reviews were completed independently of any knowledge of each subject’s BMD values. There is generally good agreement between interview and medical record data [15], but, where disagreements occurred, priority was given to documented medical history. The duration of contemporary documentation in hand averaged 30.8 years (range 1 to 81 years), and ascertainment of clinically evident fractures is believed to be complete. The diagnosis of vertebral fracture was accepted on the basis of a radiologist’s report of wedging, compression or collapse of one or more thoracic or lumbar vertebrae, and no morphometric assessment was made. “Osteoporotic” fractures were defined as clinically recognized fractures of the hip, spine or distal forearm that resulted from moderate trauma (e.g., a fall from standing height or less) among persons 35 years of age or older.
Statistical analysis
Pearson correlation coefficients were used to evaluate univariate relationships between the various bone density measurements. Correlations were compared between genders and age groups using a Fisher’s Z transformation [16]. Assuming a linear correlation, we calculated the standard error of the estimate (SEE) to assess the percentage error involved in predicting site-specific BMD values from the corresponding regional TBBD results. To standardize results, the SEE was expressed as a percentage relative to the mean of the dependent variable.
The prevalence of osteoporosis was estimated by age group and gender and summarized by direct age adjustment to the structure of the white population of the United States in 2000. Ninety-five percent confidence intervals (95% CI) were calculated assuming a Poisson distribution of the osteoporosis cases [17].
The relative risk of an osteoporotic fracture was estimated by odds ratios (OR) per change in one sex-specific SD that were obtained from bivariate logistic regression models, where a history of various fractures was the endpoint, while age and a BMD value were the predictors. To compare logistic models when substituting different BMD variables one for another, we used the c-index [18], a rank correlation that compares the predicted probabilities from a model to the observed responses (whether or not fracture was detected). This is a useful statistic for comparing models—the higher the c, the better the model does at predicting the event.
Results
The overall correlation of standard AP lumbar spine BMD with the spine region from the whole body scan was good (r 2=0.82), as delineated in Table 1 for women and men, separately. However, the correlation was even better with the lumbar spine subregion from the whole body scan (r 2=0.92). These data are illustrated in Fig. 1 for women and men of different ages. Generally, the correlation with lumbar spine subregion BMD was slightly better (P =0.044) in women (r 2=0.93) than men (r 2=0.91) and was relatively constant across life. Lumbar spine subregion data predicted standard AP spine BMD with an error (SEE) of 4.3% in women and 4.9% in men (Table 1). Despite the good correlations, there was some disagreement with respect to the presence of osteoporosis at the spine according to these two measurements as shown in Table 2.
The overall correlation of BMD at the total hip site with the pelvis region from the whole body scan was weaker (r 2=0.72). As shown in Table 1, correlations were better (P =0.039) in women (r 2=0.74) than men (r 2=0.66) and improved somewhat with age in both sexes (Fig. 2). Pelvis region BMD predicted total hip BMD with an error of 9.4% in women and 9.2% in men. Correlations between the pelvis region and BMD assessed at the femoral neck were less good, and the prediction error was also greater at 11.2% in women and 11.1% in men. Again, there was quite a bit of misclassification with respect to osteoporosis at the hip (Table 2). Sixty-eight subjects were classified as osteoporotic on the basis of total hip DXA compared to only 57 by pelvis region BMD. However, 118 of these subjects were considered osteoporotic by femoral neck BMD.
Overall correlation of the left arm subregion from the whole body scan with DXA scans of the nondominant forearm at the total wrist site was better (r 2=0.83), and arm subregion BMD predicted total wrist BMD with an error of 7.5% in women and 6.7% in men (Table 1). However, agreement on the classification of osteoporosis at the wrist was not good since the whole body arm scan was much less sensitive (Table 2). One might have expected a closer correlation with the midradius site on the forearm scan, which represents predominantly cortical bone, but overall results were similar (r 2=0.74) when left arm subregion BMD was compared with midradius BMD (Table 1), and there was an equivalent degree of misclassification for osteoporosis prevalence (data not shown).
The influence of these various measures on the estimated prevalence of osteoporosis among Rochester women and men age 50 years and over is summarized in Table 3. Compared to estimates based on AP spine BMD, prevalence was lower using data from the total body spine region, but was similar when based on the lumbar spine subregion. At the hip and wrist, prevalence estimates by regional TBBD were generally lower than those for the corresponding dedicated site-specific measurements. An exception was among postmenopausal women, where osteoporosis prevalence as assessed at the total hip was similar to that for the pelvis region. However, both the total hip and pelvis measurements in women gave a lower estimate of osteoporosis prevalence (13.4 and 14.3%, respectively) than that obtained from a more focused assessment of the femoral neck (27.4%). Similar results were seen in men where the prevalence was much greater when based on femoral neck BMD (21.9%) than when assessed at either the total hip or the pelvis region from the whole body scan (15.2 and 8.2%, respectively).
Altogether, 50% of the 200 men and 55% of the 195 women age 50 years and over had experienced one or more fractures after age 35 years. In women, more of these fractures were due to moderate trauma (123) than severe trauma (66), but the reverse was true in men (85 versus 115). Forty-six women (24%) and 33 men (16%) had one or more moderate trauma fractures that met our definition of an “osteoporotic” fracture. Prediction of a fracture history by the various BMD measurements in this cross-sectional analysis is shown in Table 4. Generally, BMD was more closely associated with fractures in women than men and with moderate trauma and osteoporotic fractures than with fractures in general. There was no clear trend with respect to fracture assessment by site-specific BMD compared to regional TBBD. In fact, the different measures could mostly be substituted one for another (Table 5). If, for example, pelvis region BMD were substituted for total hip BMD in the model predicting a history of osteoporotic fractures in women, the model c-index declined only from 0.768 to 0.724; in men, the models were comparable (0.722 and 0.723).
Discussion
In this age-stratified sample of community women and men, there was good correlation between regional BMD values measured on a whole body DXA scan and those from dedicated DXA scans at more or less comparable sites. These results are consistent with previous reports from diverse study populations [1, 2, 3, 4, 5, 6, 7]. For example, Hangartner and colleagues found a good correlation (r 2=0.88) between BMD of the spine region on the whole body scan and AP spine BMD in women and reported a prediction error (6.7%) almost identical to that observed here [6].
However, we found potential misclassification of specific study subjects with respect to the presence or absence of osteoporosis by the different techniques. Among postmenopausal women, for example, only 14% would have been classified as osteoporotic on the basis of pelvic region BMD from the whole body scan compared to 27% by measurement of femoral neck BMD. The latter figure is greater than the reported prevalence of femoral neck osteoporosis in white women from NHANES III [19], 20% when comparably adjusted to the 2000 white population ≥50 years of age, because our young normal mean (0.903 g/cm2) was higher than the comparable NHANES referent value (0.895 g/cm2, also used in Hologic devices) so that more women fell below the −2.5 SD cut-off level [12]. By contrast, the apparent prevalence of spine osteoporosis would be little changed by a switch from standard AP lumbar spine measurements to measurements of BMD from the lumbar spine subregion of the whole body scan (6.9 versus 7.4%), although there again would be misclassification of individual patients and both measures greatly underestimate spinal osteoporosis as judged from lateral DXA scans [20]. If TBBD per se were used, the overall prevalence of osteoporosis would be only 13 and 10%, respectively, in white women and men aged 50 years and over [20].
Such discrepancies are a well-known problem even with standard DXA measurements of the hip, spine and wrist [21]. Indeed, we have shown previously that the estimated prevalence of osteoporosis by WHO criteria ranges from 2 to 45% among postmenopausal women, and from 0 to 36% among men 50 years of age and older, depending upon the skeletal parameter assessed [20]. For example, more rapid bone loss at the femoral neck compared to the total hip site (−0.31%/year versus −0.15%/year) helps explain the greater prevalence of osteoporosis at the femoral neck seen here, while greater bone loss from the total wrist in women compared to men (−0.71%/year versus −0.13%/year) accounts for the sex-specific discrepancy observed at that site [22].
This raises the issue of which measurement is most “correct.” In clinical practice, the gold standard is fracture risk prediction by DXA [23, 24]. Any given level of absolute BMD predicts fractures similarly in men and women, although the relative risk per SD change may be less in men when sex-specific SDs are used in the analysis as SDs are often smaller in men than women [25]. Moreover, DXA measurements at a variety of skeletal sites are comparable when predicting fractures generally, with a relative risk per SD change of about 1.5 [10]. Similar results were seen here with regional or subregional TBBD measurements or, indeed, with TBBD per se (age-adjusted OR, 1.2; 95% CI, 1.1–1.3). However, hip fracture prediction has been considered most important, and proximal femur BMD is better at predicting hip fractures than other DXA measurements [26]. Thus, the relative risk of hip fracture per SD change in TBBD was only 1.6 [11] compared to 2.6 per SD change in femoral neck BMD [10]. As a consequence, proximal femur DXA has become the standard assessment tool for osteoporosis diagnosis and prognosis [27].
From a public policy point of view, switching from proximal femur BMD on the dedicated hip scan to pelvis region BMD on the whole body scan will likely affect the apparent prevalence of osteoporosis in the population. The magnitude of this effect varies depending on the femur subregion considered. In the present sample of postmenopausal women, the estimated prevalence of osteoporosis based on the pelvis region from the whole body scan was similar to that based on total hip BMD, but only half as high as that using femoral neck BMD from a dedicated scan. For men, estimates based on the total body pelvis region were considerably lower than either femur subregion from the dedicated scan. The exact reduction in the apparent prevalence of osteoporosis in the general population is uncertain at present because NHANES is now using a different densitometer (Hologic QDR 4500), and normative data for the United States population have not yet been released. More importantly, perhaps, different individuals are classified as osteoporotic by pelvis region BMD compared to total hip BMD, and it is not clear which measurement is better since the ability of regional data from the whole body scan to predict fracture risk has not been evaluated in detail.
It would be difficult to substitute TBBD measurements for dedicated hip and spine scans for other reasons as well. Thus, most clinical practice guidelines are designed around dedicated DXA scans, e.g., [28], and responses in site-specific BMD have been employed as an endpoint in most randomized controlled clinical trials of currently approved osteoporosis therapies. In addition, most of our knowledge about the epidemiology and pathophysiology of osteoporosis derives from hip and spine BMD, not TBBD. In particular, TBBD disproportionately assesses cortical bone compared to the specific metaphyseal scanning sites that contain more cancellous bone. Moreover, the pelvis and arm regions do not correspond anatomically to actual osteoporotic fracture sites as well as the femoral neck and ultradistal radius subregions on site-specific scans. Finally, WHO criteria for the diagnosis of osteoporosis are based on proximal femur BMD [14], and hip BMD data from NHANES III are now used as standard normal values in most densitometers [8].
The question arises whether the whole body scan could be reconfigured in some way to provide data for the ‘traditional’ scan regions, e.g., femoral neck BMD. Some DXA devices do allow special regions of interest (ROI) to be defined so that a total hip ROI similar to the dedicated total hip region of interest could be drawn on the whole body scan. The problem with this approach is that the whole body scan mode is optimized for total body measures: Because such a large bone mass and area is being measured, whole body modes typically employ lower radiation doses and larger pixel sizes, so measures of small ROIs are not as precise nor accurate as those from dedicated modes. Some densitometers also allow a predefined scan sequence for AP spine, femur and total body, but the patient is still scanned multiple times and only time is saved. Another approach would be to slow down the whole body scan to capture higher resolution AP spine and femur data, but positioning for the hip and spine scans differs [29]. For example, most DXA scanners recommend lifting the legs onto a positioning cushion to reduce lordosis for spine scans, and hip scans usually employ a leg rotation positioner. Both the spine positioning cushion and the hip positioner would interfere with whole body exams.
In conclusion, the lumbar spine subregion from the whole body scan is about as good as the site-specific AP lumbar spine scan, which is also the conclusion reached in other studies [1, 2, 3, 4, 5, 6, 7]. However, the accuracy of both approaches is challenged by artifacts in AP measurements, e.g., aortic calcification and osteophytes [20], which are quite common among older adults. The pelvis region from the whole body scan is not a very good surrogate for the proximal femur, as one might have guessed. Somewhat unexpectedly, the total body arm region does not correlate well even with the midradius site on the forearm scan. These data are limited by the relatively small number of subjects and the cross-sectional nature of the fracture risk analysis. Nonetheless, in the absence of prospective data on fracture risk prediction and assessment of osteoporosis treatment responses using regional data from whole body scans, it seems clear that it would be premature to substitute TBBD for site-specific BMD in health policy considerations or patient management decisions. Fortunately, it is now planned to again include dedicated hip scans in the NHANES protocol in 2005.
References
Lloyd T, Eggli DF (1992) Measurement of bone mineral content and bone density in healthy 12-year-old white females. J Nucl Med 33:1143–1145
Feyerabend AJ, Lear JL (1993) Regional variations in bone mineral density as assessed with dual-energy photon absorptiometry and dual X-ray absorptiometry. Radiology 186:467–469
Lu PW, Briody JN, Ogle GD, Morley K, Humphries IRJ, Allen J, Howman-Giles R, Sillence D, Cowell CT (1994) Bone mineral density of total body, spine, and femoral neck in children and young adults: a cross-sectional and longitudinal study. J Bone Miner Res 9:1451–1458
Nysom K, Mølgaard C, Michaelsen KF (1998) Bone mineral density in the lumbar spine as determined by dual-energy X-ray absorptiometry: comparison of whole body scans and dedicated regional scans. Acta Radiol 39:632–636
Franck H, Munz M (2000) Total body and regional bone mineral densitometry (BMD) and soft tissue measurements: correlations of BMD parameter to lumbar spine and hip. Calcif Tissue Int 67:111–115
Hangartner TN, Skugor M, Landoll JD, Matkovic V (2000) Comparison of absorptiometric evaluations from total-body and local-region skeletal scans. J Clin Densitometry 3:215–225
Hammami M, Koo MW, Koo WW, Thomas RT, Rakhman D (2001) Regional bone mass measurement from whole-body dual energy X-ray absorptiometry scan. J Clin Densitom 4:131–136
Hanson J (1997) Standardization of femur BMD. J Bone Miner Res 12:1316–1317
National Osteoporosis Foundation (2002) America’s bone health: the state of osteoporosis and low bone mass in our nation. National Osteoporosis Foundation, Washington, DC, pp 1–55
Marshall D, Johnell O, Wedel H (1996) Meta-analysis of how well measures of bone mineral density predict occurrence of osteoporotic fractures. BMJ 312:1254–1259
Schott AM, Cormier C, Hans D, Favier F, Hausherr E, Dargent-Molina P, Delmas PD, Ribot C, Sebert JL, Breart G, Meunier PJ for the EPIDOS Group (1998) How hip and whole-body bone mineral density predict hip fracture in elderly women: the EPIDOS Prospective Study. Osteoporos Int 8:247–254
Melton LJ III, Atkinson EJ, O’Connor MK, O’Fallon WM, Riggs BL (1998) Bone density and fracture risk in men. J Bone Miner Res 13:1915–1923
Melton LJ III (1996) History of the Rochester Epidemiology Project. Mayo Clin Proc 71:266–274
Kanis JA, Melton LJ III, Christiansen C, Johnston CC, Khaltaev N (1994) The diagnosis of osteoporosis. J Bone Miner Res 9:1137–1141
Beard CM, Melton LJ III, Cedel SL, Richelson LS, Riggs BL (1990) Ascertainment of risk factors for osteoporosis: comparison of interview data with medical record review. J Bone Miner Res 5:691–699
Snedecor GW, Cochran WG (1980) Statistical methods. Iowa State University Press, Ames, IA, pp 185–188
Bergstralh EJ, Offord KP, Chu CP, Beard CM, O’Fallon WM, Melton LJ III (1992) Calculating incidence, prevalence and mortality rates for Olmsted County, Minnesota: an update. Technical report series no. 49, section of biostatistics. Mayo Clinic, Rochester, MN
Harrell FE Jr, Lee KL, Mark DB (1996) Multivariable prognostic models: issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Stat Med 15:361–387
Looker AC, Orwoll ES, Johnston CC Jr, Lindsay RL, Wahner HW, Dunn WL, Calvo MS, Harris TB, Heyse SP (1997) Prevalence of low femoral bone density in older US adults from NHANES III. J Bone Miner Res 12:1761–1768
Melton LJ III, Khosla S, Achenbach SJ, O’Connor MK, O’Fallon WM, Riggs BL (2000) Effects of body size and skeletal site on the estimated prevalence of osteoporosis in women and men. Osteoporos Int 11:977–983
Faulkner KG, von Stetten E, Miller P (1999) Discordance in patient classification using T-scores. J Clin Densitometry 2:343–350
Melton LJ III, Khosla S, Atkinson EJ, O’Connor MK, O’Fallon WM, Riggs BL (2000) Cross-sectional versus longitudinal evaluation of bone loss in men and women. Osteoporos Int 11:592–599
U.S. Preventive Services Task Force (2002) Screening for osteoporosis in postmenopausal women: recommendations and rationale. Ann Intern Med 137:526–528
Cummings SR, Bates D, Black DM (2002) Clinical use of bone densitometry. JAMA 288:1889–1897
Melton LJ III, Orwoll ES, Wasnich RD (2001) Does bone density predict fractures comparably in men and women? Osteoporos Int 12:707–709
Nelson HD, Helfand M, Woolf SH, Allan JD (2002) Screening for postmenopausal osteoporosis: a review of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med 137:529–541
Kanis JA, Glüer C-C for the Committee of Scientific Advisors, International Osteoporosis Foundation (2000) An update on the diagnosis and assessment of osteoporosis with densitometry. Osteoporos Int 11:192–202
National Osteoporosis Foundation (2003) Physician’s guide to prevention and treatment of osteoporosis. National Osteoporosis Foundation, Washington, DC, pp 1–37
Watts NB (2004) Fundamentals and pitfalls of bone densitometry using dual-energy X-ray absorptiometry (DXA). Osteoporos Int 15:847–854
Acknowledgements
We would like to thank Vicki Gathje and Margaret Holets for data collection, Elizabeth Atkinson for assistance with data analysis and Mary Roberts for help in preparing the manuscript. This work was supported by research grant AR27065 from the National Institute of Arthritis, Musculoskeletal and Skin Diseases, U.S. Public Health Service.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Melton, L.J., Looker, A.C., Shepherd, J.A. et al. Osteoporosis assessment by whole body region vs. site-specific DXA. Osteoporos Int 16, 1558–1564 (2005). https://doi.org/10.1007/s00198-005-1871-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-005-1871-y