Abstract
Forty-eight community living women 66–87 years old volunteered to participate in a 12-month prospective, randomized, controlled, trial. The aim was to determine if a combined weight-bearing training program twice a week would be beneficial to bone mineral density and neuromuscular function. The participants were pairwise age-matched and randomly assigned to either an exercise group (n=24) or a control group (n=24). Twenty-one subjects in the intervention group and 19 in the control group completed the study. The exercise program lasted for 50 min and consisted of a combination of strengthening, aerobic, balance and coordination exercises. The mean percentage of scheduled sessions attended for the exercise group was 67%. At the completion of the study, the intervention group showed significant increments in bone mineral density of the Ward’s triangle (8.4%, P<0.01) as well as improvement in maximum walking speed (11.4%, P<0.001) and isometric grip strength (9.9%, P<0.05), as compared to the control group. The conclusion was that a combined weight-bearing training program might reduce fracture risk factors by improving bone density as well as muscle strength and walking ability. This program could be suitable for older community living women in general, and might, therefore, have important implications for fracture prevention.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Most studies on osteoporosis have indicated an increasing incidence in Europe and North America during the past 30–40 years [1, 2]. Also, the age-adjusted incidence has increased [3]. The reasons for this are unknown, but genetic or environmental factors, including the habitual level of physical activity, might contribute to the increasing incidence [4].
The impact of osteoporosis lies in the associated fractures, which cause great suffering and reduced quality of life for the affected individuals [5]. The fractures are also associated with high costs for society [6]. Low bone density is thought to be the single most important risk factor in the development of fragility fractures, but neuromuscular impairment such as reduced muscle strength, impaired gait and balance [7, 8], as well as physical inactivity and a sedentary lifestyle, have been suggested to contribute to the increasing risk [9, 10, 11].
Most previous intervention studies have been performed on premenopausal and younger postmenopausal women and have suggested that exercise or physical activity might increase bone mass [12, 13, 14, 15]. However, there are only a few randomized studies on women with a mean age above 70 years. One study [16] examined the effect of weight-lifting training, and another study [17] investigated the effect of a weight-bearing program, including strengthening, coordination and balance exercises, where, though, the emphasis was on social interaction and enjoyment. Those studies did show significant improvements in muscle strength but not in bone mineral density.
The aim of this study was to investigate whether a combined weight-bearing training program, containing strengthening, aerobic, balance and coordination exercises but no jumping activities, is suitable for older community living women in general and to determine the effects of the program on bone mineral density, muscle strength, gait, and balance.
Materials and methods
Subjects
In order to recruit volunteers for a prospective, randomized controlled trial, an informative lecture was given at the University for the Elderly in Umeå, Sweden. A study invitation was also sent to a group of women who were born in 1920 and who had already participated in a previous study called U-70. A total of 56 community living women 66–87 years old volunteered to take part in the present study. Exclusion criteria were dementia, current smoking, current hormone replacement therapy (HRT), and use of a walking aid. The subjects underwent a medical examination carried out by a physician as well as assessment carried out by a physiotherapist. All individuals who reported cardiovascular disease, or functional disability, of a degree that would contraindicate physical exercise were then excluded. A total of eight volunteers were excluded, due to HRT (n=1), tamoxifen treatment (n=1), heart disease (n= 4), and smoking (n=1), and one person changed her mind and did not want to participate, leaving 48 subjects in the study.
The participants were pairwise age-matched and randomly assigned to either an exercise group (n=24) or a control group (n=24). Twenty-one subjects in the intervention group and 21 in the control group completed the study (baseline characteristics are presented in Table 1). The other participants dropped out, from the intervention group because of dementia (n=1), heart failure (n=1), and unspecified knee pain (n=1), and from the control group because of lack of interest (n=2); one person in the control group died. Two other subjects in the control group started to participate on a regular basis in another aerobics class during the study period and were therefore excluded, leaving 19 subjects in the control group for the statistical analyses. All subjects included in the study were assessed twice, first at baseline prior to the start of the exercise program and then at the follow up visit after completion of the 1-year training program. None of the subjects used any medication known to affect bone metabolism, nor did they have any endocrinological diseases or bone diseases. Informed consent was obtained from all subjects.
The Ethics Committee of the Medical Faculty, Umeå University, approved the study.
Assessments
Bone mineral density measurements
Bone mineral density (BMD; in grams per square centimeter) of the total body, percent fat, fat mass, and lean body mass were measured before and after the intervention. A dual-energy X-ray absorptiometer (DXA), Lunar DPX-L, software version 1.3y (Lunar Co., Wis., USA) was used. The BMD of the head and arms was derived directly from the total body scan, whereas the BMD of the right femoral neck, trochanter major (trochanter), Ward’s triangle (Ward’s), and lumbar spine BMD were derived by means of the femur software and lumbar software, respectively. T-scores, defined as the number of standard deviations from reference means of young adults, were calculated by means of the results of the bone measurements. To minimize inter-observer variation, the same investigator carried out all analyses. In our laboratory the coefficient of variation (CV-value) (standard deviation/mean) for repeated measurements was estimated at 0.7% (total body), 2.2% (head), and 1.0% (arms). CV-values for the femur and spine software were 0.8% (neck), 1.2% (Ward’s), 1.5% (trochanter), and 0.6% (lumbar spine). CV-values for percent body fat, fat mass, and lean body mass were 3.9%, 2.6%, and 0.9%, respectively.
Clinical measurements
Height and weight were measured with standard equipment, with the subjects in stocking feet and underwear. Body mass index (BMI) was calculated as weight (in kilograms)/height (in meters)2.
Dietary intake
Total dietary intake, including total energy (in kilocalories), calcium (in milligrams), vitamin D (in micrograms), and the use of vitamin and mineral supplements were estimated on a complete 3-day dietary record at baseline, and at the follow-up visit. The food composition was calculated with MATS software (MATS program, version 4.0. Västerås, Sweden: Rudans Lättdata 1997).
Assessment of physical activity
The level of physical activity during the summer and winter seasons was estimated separately according to the Frändin–Grimby activity scale [18]. The subjects were also asked to report how many minutes they spent walking briskly every week.
Isometric strength of leg extensors
Isometric muscle strength of the knee extensors was measured (in Newtons) with a tensiometer (Gossen, Sweden, no 12016) with the test person sitting on a table. The equipment was marked in kilograms, with a precision of 0.5 kg, which corresponds to 4.9 N. Hip and knee were kept in 90° flexion, determined by a goniometer. The subjects were instructed to perform three maximal isometric contractions with their right legs, with 30 s of rest between each contraction. The highest value was used for the statistical analyses.
Isometric grip strength
Isometric grip muscle strength was also measured (in Newtons), with the same tensiometer as above, with the subjects sitting with their arms fixed and elbow angles in 90° flexion and semi-pronation throughout the test. Shoulders were in a 0° flexion angle. The subjects were instructed to grip maximally, and three maximal attempts with their dominant arms were recorded, with 30 s rest in between. The highest value was used for further analyses.
Maximum walking speed
The subjects were initially asked to walk 30 m along a walkway at normal speed and then told to walk the same distance as fast as possible without running. A timer was started at commencement and stopped when the trunk of the subject reached the finishing line. Time was registered to one decimal place of a second [19].
Balance
We determined standing balance by timing each participant as she stood on one leg with her eyes open. The subjects were allowed to choose which leg they wanted to use, and the maximum time was set at 120 s. Two attempts were allowed, with 1 min of rest between, and the best time was recorded. The same leg was used at the follow-up test 1 year later. Balance was also assessed with the Berg Balance Scale [20].
Intervention
Exercise program
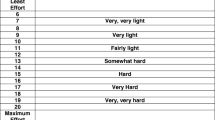
The intervention group participated in a weight-bearing exercise program twice a week for 12 months, with a 5-week break during the summer vacation. The program was accompanied by music, lasted for 50 min and was supervised by a physiotherapist. The exercise program consisted of a combination of strengthening, aerobic, balance and coordination exercises, designed to load bones with intermittent compressive forces, introducing atypical and novel stress on the bone, which is known to improve skeletal integrity [21], and improving neuromuscular function, the lack of which is associated with falls and fractures. The program was preceded by 10 min of warming-up, followed by a mix of aerobic, strengthening, balance and coordination exercises for 27 min. The program then ended with 11 min of cooling down, stretching and relaxation.
During the aerobic exercises the subjects could choose between walking and jogging and, thus, mainly used the large muscle groups in their legs. The aerobic exercises consisted of steps in different combinations and directions, with coordinated arm movements. However, in order to suit all subjects the exercises did not include jumping activities. Aerobic capacity exercises were performed for a total of 10 min divided into three sections during the whole exercise session. During the strengthening section, legs, abdominal, and back muscles were trained by means of body resistance only. Individually assessed dumbells were used during the training of the arms.
The strengthening exercise was performed for 2×8-12 repetitions for each muscle group and lasted for a total of 12 min. Heavier dumbells were used, in a progressive phase during the study time, to increase the intensity as well as change the biomechanics conditions. Dynamic and static balance and coordination were trained throughout the whole program but more intensively for 5 min of the program, with exercises such as one-leg standing and more advanced coordinated steps. Making more complex or faster coordinated movements increased the intensity in the balance and aerobic exercise. The difficulties in the balance exercise could also be increased by decreasing the base of support. In order to suit all participants, the intensity of the program was self-paced and the subjects were allowed to rest if necessary.
If participants missed out on a training session they were advised to perform a home exercise program instead. This program included brisk walking for 30 min, squats with 3×10 repetitions, and training of hand grip with a piece of T-foam for 3×15 repetitions.
Control group
The women in the control group were asked not to increase their normal physical activity during the study period. They were also interviewed after 6 and 12 months so that any changes in their exercise habits could be monitored.
Statistical analysis
All data were analyzed with the SPSS package (SPSS, Chicago, USA) for Macintosh. We used Student’s t-test for independent samples to test for differences between the control group and the exercise group. In order to correct for different baseline values when analyzing the inter-group significance of changes, we also performed analysis of covariance (ANCOVA), by means of baseline values as covariate [22]. Changes from baseline and over the 12-month training period were evaluated with paired t-tests.
Multiple regression models were adapted to analyze the effect of the training activity in the presence of other predictor variables. Possible interaction was examined between training activity, age, weight, BMI, age at menopause, weight loss before the study and baseline values. Bivariate correlations were also measured, in the respective groups, between the changes in outcome variables and different explanatory factors. Pearson’s coefficient of correlation was used for this. Results were considered significant at the level of P<0.05. Power calculations were done for BMD, muscle strength and maximal walking speed. A sample size of 24 in each group, α-level of 0.05 and standard deviation of 10% gave 30% power to detect a 5% difference in change between the two groups, as well as intra-group differences.
Results
Anthropometric data on exercisers and controls are presented in Table 1.There was no significant difference in total BMD between the groups at the beginning of the study, but the BMD in the Ward’s triangle was significantly lower in the exercise group at baseline. The initial degree of physical activity was comparable in the two groups. No significant group differences in age, height, weight, fat mass, lean body mass, BMI or food intake were found at baseline, but it should be noted that the mean age for menopause was significantly higher in the control group.
The training compliance in the intervention group, defined as percent of scheduled sessions attended, was 67% (range 23%–95%). Besides the training program, there were no significant changes in either group in the level of physical activity or other daily habits, nor were there any significant changes in the estimated dietary intake in either of the groups, and there were no injuries during the year of the study.
Outcome data for bone mass and neuromuscular measurements on exercisers and controls are presented in Table 2. At the follow up, we noticed a slight increase (5.3%) in BMD of the Ward’s triangle in the exercise group, whereas a decrease (−3.1%) was observed among the controls. After adjustments for baseline differences in the BMD, weight and age, inter-group percent change scores in BMD of the Ward’s were found to be significant (P<0.05). Inter-group percent change scores in the BMD of arms, lumbar spine, and trochanter were not significant, although there were significant increments in the BMD of the arms (1.5%), lumbar spine (3.1%) and trochanter (6.3%) sites in the exercise group. In the control group, change scores in the BMD of arms, lumbar spine, and trochanter were 1.5%, 1.0%, and 2.9%, respectively. Similar results were found when changes in T-scores of the different sites were analyzed (data not shown).
Furthermore, we observed significant improvement in the subjects’ ability to stand on one leg (75.7%), increased maximum walking speed (15.3%), and improved isometric grip strength (7.4%), in the exercise group, as well as a tendency toward improved ability to stand on one leg (42.7%), a significant increase in maximum walking speed (3.9%), and a tendency toward a decrease in the isometric grip strength in the control group (−2.5%). We also observed a tendency toward an increase in isometric strength of knee extensors (5.6%) in the exercise group and a tendency toward a decrease (−1.2%) in the control group However, the maximum walking speed showed a highly significant inter-group difference (P<0.001). In addition, the isometric grip strength showed a significant inter-group difference (P<0.05). None of the other neuromuscular parameters achieved statistical significant differences.
Bivariate correlations were performed in each group and demonstrated that the number of training sessions attended was not associated with any of the BMD changes but was positively associated with maximum walking speed (Pearson coefficient 0.664, P<0.001). We did not observe any interaction between the significant changes in the BMD and muscle strength, age, BMI, age at menopause, or weight loss before the study. However, we found a significant correlation between weight at baseline and change in the BMD of Ward’s triangle in the control group (Pearson coefficient 0.656, P<0.01). However, no significant correlations were found between weight and changes at other BMD sites. In the exercise group, weight was not associated with any of the BMD changes. In a stepwise regression model, we did not find any of the parameters age, height, age at menopause, weight, BMI, fat mass, lean body mass, one-leg standing, maximum walking speed, grip strength, knee extension strength, or dietary intake to predict changes in the BMD.
Discussion
In the present study, we have shown that a 1-year combined weight-bearing training program was associated with a significant increase in the BMD of the Ward’s triangle, trochanter, lumbar spine, and arms in older women. Surprisingly, we also found significant increases in the BMD of the arms and trochanter region in the non-exercising control group. This was unexpected, since normally in this age group, the BMD decreases [11, 23, 24]. Yet, in our study, a decrease in the BMD was demonstrated only in Ward’s triangle in the control group, whereas we observed a slight increase in the same region in the exercise group. In fact, this was the only site where we found a significant difference between the groups, suggesting that this was a true effect of the training. This is in accordance with an earlier study [25] that showed a tendency toward an increase in BMD of Ward’s triangle after a 12-month strength-training program.
Cancellous bone has a higher bone turnover than cortical bone, which could explain why we found adaptation in Ward’s triangle but not in the femoral neck. Thus, the duration of the intervention period might have been too short to observe a response in the femoral neck area [26, 27]. Another explanation for the lack of improvement in the femoral neck could be that this type of training, without jumping activities, is not creating sufficient strains to evoke an osteogenic response in this area. In premenopausal women earlier studies indicate that high-impact loading is also needed to obtain adaptations in the lumbar spine [14]. However, studies performed on postmenopausal women have, at the best, shown a maintenance effect on BMD with high-impact exercise [27, 28].
The present exercise program included no jumping-activities because the participants were rather old, and jumps would, therefore, be too risky and even difficult for some subjects in this group. Several earlier studies with older postmenopausal women have not shown any effects of jumping exercises on bone mass [27, 29, 30]. Another study found significant effects of jumping activities only in premenopausal women, not in postmenopausal women [31]. One study even indicates that intensive high-impact exercise, such as jumping, may cause reduction in regional bone mass [29]. The type of exercise performed in the present study seems to be sufficient, however, to maintain and even increase bone density at Ward’s triangle. Since this site is highly associated with proneness to both intertrochanteric and cervical hip fractures, even small increments in BMD may lower the risk for hip fractures, especially in individuals with below normal bone mass [32]. However, it should be pointed out that this type of exercise was not associated with any improvement in the femoral neck BMD, which is another strong predictor of the risk for hip fractures.
This combined training program was also associated with significant improvement in the subjects’ ability to stand on one leg, in the exercise group, although there was no significant inter-group difference. There were, however, significant inter-group differences in increased maximum walking speed and improved isometric grip strength, with the higher improvement in the training group. We also observed tendencies toward an increase in isometric muscle strength of the knee extensors in the exercise group and a decrease in the control group. However, our method of measuring the strength of knee extensors may not be the best for the outcome of this type of exercise [33]. It might have been more appropriate and sensitive if we had measured dynamic strength to study the changes in muscle strength. One earlier cross-sectional study indicates that there is a connection between the strength of knee extensors and the BMD of the Ward’s triangle and the lumbar spine in elderly women [34], but we could not verify those findings in our present study.
Neuromuscular impairment such as reduced gait speed is a significant and independent predictor of the risk of hip fracture in elderly, mobile, women [7], and earlier studies suggests that physical activity significantly reduces the risk of falls and fractures by improving muscle strength and balance [17, 35, 36]. Gregg and co-writers [37] demonstrated a significant reduction in the age-adjusted risk of hip fracture among physically active women as compared with inactive women, and recommended low-intensity physical activity for sedentary older women as fracture prevention. It is, therefore, possible that the gains in strength and gait speed of the elderly women in this combined training program might reduce the propensity for falls.
Together with the increments in bone mass seen in the present study, this combined training program may subsequently have a protective effect to reduce the risk of osteoporotic fractures. It is well known that lean body mass normally decreases with age [38]. Yet, even though participants in the exercise group improved their neuromuscular performance, such as isometric grip strength, their ability to stand on one leg, and their maximal walking speed and lean body mass decreased in this group as well as in the control group. This gives further support that this training program enhanced neuromuscular function due to neural adaptation rather than to muscle hypertrophy [39].
One major shortcoming of this study is that the sample is rather small, and the power might not have been sufficient to detect significant differences in the BMD changes between the two groups. Furthermore, we do not know for certain whether the subjects in the exercise group performed the home exercise program or not on those occasions when they did not attend their training group. This could certainly have influenced the results. The attendance, however, was good, implying that this type of training program is suitable for older women.
Another possible explanation for the lack of significant differences between the groups and the increments in the non-exercising control group might be that our subjects were healthy volunteers and that they volunteered because of a genuine interest in physical activity and health projects. Some of the participants became disappointed when they were randomized to the control group. We also know that many of the women were friends, and we therefore believe that some subjects in the control group came to know about the training exercises in that way and were, subsequently, not as sedentary as they would otherwise have been. However, no significant changes in their exercise habits were noticed during the study period. On the other hand, our method for estimating changes in the level of physical activity is not very sensitive. Furthermore, blinding of the research staff was not possible. Therefore, notwithstanding the quantitative test measures, it is possible that some improvements may have resulted from observer bias.
In summary, this study suggests that a combined weight-bearing training program, without jumping activities but including strengthening, aerobic, balance and coordination exercises, might reduce fracture risk factors by improving bone density as well as neuromuscular functions associated with the risk of falls. In this cohort there was no problem for them to participate on a regular basis in a program of this intensity. The program could be suitable for older community living women in general and might, therefore, have important implications for fracture prevention. However, this needs to be further elucidated in future studies.
References
Melton LJ 3rd (1996) Epidemiology of hip fractures: implications of the exponential increase with age. Bone 18 [3 Suppl]:121S–125S
Johnell O, et al (1992) The apparent incidence of hip fracture in Europe: a study of national register sources. MEDOS Study Group. Osteoporos Int 2:298–302
Kannus P, et al (1999) Hip fractures in Finland between 1970 and 1997 and predictions for the future. Lancet 353:802–805
Gullberg B, Johnell O, Kanis JA (1997) World-wide projections for hip fracture. Osteoporos Int 7:407–413
Lips P, et al (1997) Quality of life as outcome in the treatment of osteoporosis: the development of a questionnaire for quality of life by the European Foundation for Osteoporosis. Osteoporos Int 7:36–38
Zethraeus N, Gerdtham UG (1998) Estimating the costs of hip fracture and potential savings. Int J Technol Assess Health Care 14:255–267
Dargent-Molina P, et al (1996) Fall-related factors and risk of hip fracture: the EPIDOS prospective study. Lancet 348:145–149
Tinetti ME, Speechley M, Ginter SF (1988) Risk factors for falls among elderly persons living in the community. N Engl J Med 319:1701–1707
Albrand G, et al (2003) Independent predictors of all osteoporosis-related fractures in healthy postmenopausal women: the OFELY study. Bone 32:78–85
Cummings SR., et al (1995) Risk factors for hip fracture in white women. Study of Osteoporotic Fractures Research Group. N Engl J Med 332:767–773
Nguyen TV, Sambrook PN, Eisman JA (1998) Bone loss, physical activity, and weight change in elderly women: the Dubbo osteoporosis epidemiology study. J Bone Miner Res 13:1458–1467
Bravo G, et al (1996) Impact of a 12-month exercise program on the physical and psychological health of osteopenic women. J Am Geriatr Soc 44:756–762
Berard A, Bravo G, Gauthier P (1997) Meta-analysis of the effectiveness of physical activity for the prevention of bone loss in postmenopausal women. Osteoporos Int 7:331–337
Heinonen A, et al (1996) Randomised controlled trial of effect of high-impact exercise on selected risk factors for osteoporotic fractures. Lancet 348:1343–1347
Kelley GA (1998) Exercise and regional bone mineral density in postmenopausal women: a meta-analytic review of randomized trials. Am J Phys Med Rehabil 77:76–87
McCartney N, et al (1995) Long-term resistance training in the elderly: effects on dynamic strength, exercise capacity, muscle, and bone. J Gerontol A Biol Sci Med Sci 50:B97–104
Lord SR, et al (1996) The effects of a community exercise program on fracture risk factors in older women. Osteoporos Int 6:361–367
Frändin K, Grimby GG (1994) Assessment of physical activity, fitness and performance in 76-year-olds. Scand J Med Sci Sports 4:41–46
Collen FM, Wade DT, Bradshaw CM (1990) Mobility after stroke: reliability of measures of impairment and disability. Int Disabil Stud 12:6–9
Berg K, et al (1989) Measuring balance in the elderly: preliminary development of an instrument. Physiother Can 41:304–311
Lanyon LE (1996) Using functional loading to influence bone mass and architecture: objectives, mechanisms, and relationship with estrogen of the mechanically adaptive process in bone. Bone 18 [1 Suppl]:37S–43S
Vickers AJ, Altman DG (2001) Statistics notes: analysing controlled trials with baseline and follow up measurements. BMJ 323:1123–1124
Dalsky GP, et al (1988) Weight-bearing exercise training and lumbar bone mineral content in postmenopausal women. Ann Intern Med 108:824–848
Ahlborg HG, et al (2003) Bone loss and bone size after menopause. N Engl J Med 349:327–334
Pruitt LA, Taaffe DR, Marcus R (1995) Effects of a one-year high-intensity versus low-intensity resistance training program on bone mineral density in older women. J Bone Miner Res 10:1788–1795
Shaw J, Snow C (1998) Weighted vest exercise improves indices of fall risk in older women. J Gerontol Med Sci 53:M53–58
Snow CM, et al (2000) Long-term exercise using weighted vests prevents hip bone loss in postmenopausal women. J Gerontol A Biol Sci Med Sci 55:M489–491
Bassey EJ, Ramsdale SJ (1995) Weight-bearing exercise and ground reaction forces: a 12-month randomized controlled trial of effects on bone mineral density in healthy postmenopausal women. Bone 16:469–476
Von Heideken Wagert P, et al (2002) Jumping exercises with and without raloxifene treatment in healthy elderly women. J Bone Miner Metab 20:376–382
Uusi-Rasi K, et al (2003) Effect of alendronate and exercise on bone and physical performance of postmenopausal women: a randomized controlled trial. Bone 33:132–143
Bassey EJ, et al (1998) Pre- and postmenopausal women have different bone mineral density responses to the same high-impact exercise. J Bone Miner Res 13:1805–1813
Cummings SR, et al (1993) Bone density at various sites for prediction of hip fractures. The Study of Osteoporotic Fractures Research Group. Lancet 341:72–75
Murphy AJ, Wilson GJ (1996) Poor correlations between isometric tests and dynamic performance: relationship to muscle activation. Eur J Appl Physiol Occup Physiol 73:353–357
Hughes VA, et al (1995) Muscle strength and body composition: associations with bone density in older subjects. Med Sci Sports Exerc 27:967–974
Province MA, et al (1995) The effects of exercise on falls in elderly patients. A preplanned meta-analysis of the FICSIT Trials. Frailty and Injuries: Cooperative Studies of Intervention Techniques. JAMA 273:1341–1347
Carter ND, et al (2002) Community-based exercise program reduces risk factors for falls in 65- to 75-year-old women with osteoporosis: randomized controlled trial. CMAJ 167:997–1004
Gregg EW, et al (1998) Physical activity and osteoporotic fracture risk in older women. Study of Osteoporotic Fractures Research Group. Ann Intern Med 129:81–88
Lindsay R, et al (1992) Bone mass and body composition in normal women. J Bone Miner Res 7:55–63
Sale DG (1988) Neural adaptation to resistance training. Med Sci Sports Exerc 20 [5 Suppl]:S135–145
Acknowledgements
We would like to acknowledge the late Dr Eva Gagerman, who was the main initiating force in this study. Without her the study would not have been accomplished. We would also like to thank Professor Ronny Lorentzon for valuable advice, research assistant Torsten Sandström for skillful bone density measurements, and the dieticians Britt-Marie Nyberg and Maine Carlsson for calculating the dietary intake. Special thanks to the physiotherapists Erik Rosendahl, Åsa Karlsson, Ulrica Radsjö, and Anna Åström for supervising the exercise classes. This study was supported by grants from the Borgerskapet in Umeå Research foundation, Gun and Bertil Stohnes’ foundation and funds of the Faculty of Medicine at Umeå University, Sweden.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Englund, U., Littbrand, H., Sondell, A. et al. A 1-year combined weight-bearing training program is beneficial for bone mineral density and neuromuscular function in older women. Osteoporos Int 16, 1117–1123 (2005). https://doi.org/10.1007/s00198-004-1821-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-004-1821-0