Abstract
This study assessed the proportion of patients treated with anti-osteoporotic drugs during the 1-year period after hospitalization for a fracture, and the influence of a guideline in the period 1998–2000 on the likelihood of receiving treatment for osteoporosis after a fracture. Patients were assessed retrospectively for anti-osteoporotic drug use during a 1-year period following hospitalization for non-traumatic fracture. The PHARMO system, a population-based database (n=865,000) containing drug and hospitalization data of community-dwelling inhabitants of defined areas in the Netherlands, was used. The study population comprised 1654 patients age 50 years and over who were admitted to hospital for a fracture resulting from a fall during the period 1998–2000. The treatment rate of newly treated patients and the change in treatment rate throughout the period 1998–2000 were the outcome measures. The majority of these patients were women (73%), and had femur fractures (51%). In total, 247 out of 1654 patients (15%) were prescribed anti-osteoporotic drugs within 1 year after discharge from the hospital. Of these 247 patients, 86 were newly treated, mainly with bisphosphonates in the year after discharge following the fracture, yielding a new treatment rate of 5%. The likelihood of receiving treatment for osteoporosis following fracture did not change with the calendar year of fracture (OR 0.95; 95% CI: 0.68–1.30). The result of this study shows that despite the introduction of an osteoporosis treatment guideline in 1999 recommending treatment for fracture patients, most of the time, fracture patients are not being treated for osteoporosis. Thus, to a large extent, osteoporosis remains under-treated.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis is a silent disease that often remains asymptomatic and undetected until fracture occurs. The prevalence of osteoporosis among patients of 50 years and older varies from 10 to 20%, depending on race and assessment methods [1, 2, 3]. In a recent population survey in Belgium, a demographic population comparable to the Netherlands, the prevalence of osteoporosis was estimated at 15% among 2649 postmenopausal women aged 45–91 years [1]. Fractures of the wrist, hip and vertebrae are well-recognized consequences of bone fragility, which occurs as bone mass decreases, i.e. the disease of osteoporosis [4]. However, although patients fulfill the diagnostic criteria of osteoporosis, not all patients will suffer from the clinical consequences. On the other hand, patients who have already had a fracture have an increased risk of subsequent fractures [5, 6, 7, 8]. Therefore, focusing attention on patients with a fracture may be an important step towards a significant reduction in the burden of osteoporosis in society [9].
It is, however, unknown how many patients are treated for secondary prevention of osteoporotic fractures. Some studies in different countries have observed that a significant proportion of patients did not receive any treatment for osteoporosis even after a fracture [10]. However, the majority of these studies have been limited to a small sample of patients or to center-specific populations [11, 12, 13, 14, 15]. In the Netherlands, three guidelines advise on post-fracture diagnostic assessment and treatment of osteoporosis [16, 17, 18]. Although these guidelines differ with respect to the need for screening and the number of risk factors, they all agree that fractures are major targets for case finding. The guideline for general practitioners appears to be the more conservative guideline available in the Netherlands, and was implemented during the study period. According to this guideline, treatment is indicated for patients with an osteoporotic fracture or those using corticosteroids (equivalent to prednisone >7.5 mg/day) [18].
In this study, we assessed the proportion of patients treated with anti-osteoporotic drugs after hospitalization for a fracture of wrist, spine, hip and other bones resulting from accidental falls. Furthermore, it was investigated whether this proportion increased or decreased with years following hospitalization due to fracture. This is particularly relevant because the GP treatment guideline was introduced in 1999.
Materials and methods
Data setting
This study used data from the PHARMO system, a population-based database (n=865,000), in which data concerning drug use and hospitalizations are collated prospectively from all community-dwelling residents of 25 geographic and demographic areas since 1989, scattered throughout the Netherlands. Patients histories include per resident detailed information of all dispensed drugs by date of dispensing, type, prescriber, dose, duration of use and costs as well as information of all discharge diagnoses (ICD-9-CM), surgical procedures and other administrative information. Data from the PHARMO system permit accurate and detailed estimates of drug use characteristics and hospital morbidity in the Netherlands [17].
Selection of patients
All patients, 50 years of age or older and hospitalized for a fracture of the hip, spine, wrist or other fractures (ICD-9-CM codes: 805, 810–813, 820–824) resulting from a fall during the period 1998–2000 were selected from the PHARMO database. We assumed based on clinical observations that most of these fractures had been caused by falls from a standing height or less. Fracture sites like proximal femur, proximal humerus, distal forearm, thoracic and lumbar spine (ICD-9-CM codes: 805.2, 805.4, 812.0, 813.4 and 820) were considered to be osteoporotic with certainty; the ribs, sternum and pelvis were possible osteoporotic fracture sites; the remaining fractures were not considered to be of osteoporotic origin. Patients who died or who were sent to rehabilitation or nursing homes were excluded from this study, as the drug information for these patients was incomplete in the PHARMO system. All patients included in this study had to have a history of registration in the PHARMO area for a 5-year period prior to the index date, a follow-up period of at least 1 year and virtual complete hospital and drug exposure histories. For each patient, the index date was set on the discharge date of the first fracture-related admission in the study period.
Use of anti-osteoporotic drugs
Dispensing of one or several anti-osteoporotic drugs throughout the year was assessed during the year following hospital discharge. Anti-osteoporotic drugs included in this study were sodium fluoride (Procal), vitamin D and calcium formulations labeled for treatment of osteoporosis, bisphosphonates, SERMs and estrogens. Patients who had been dispensed an anti-osteoporotic drugs in the 5-year period prior to the date of fracture hospitalization were classified as previously diagnosed and treated for osteoporosis.
Validation
For all patients for whom GP data were accessible and who were admitted for fractures (approximately 10–15%), the general practitioners’ case records were examined for diagnostic tests (i.e. dual-energy X-ray absorptiometry; DXA), diagnosis of osteoporosis and subsequent treatment before and after index hospitalization due to fracture.
Statistical analyses
The proportion patients treated with anti-osteoporotic drugs was estimated by calculating the percentage of patients who received at least one prescription of any anti-osteoporotic medication during the year following discharge from the hospital. Sub-analyses were performed by excluding patients already treated with anti-osteoporotic drugs prior to admission for the fracture, to estimate the percentage of patients newly treated with anti-osteoporotic drugs. The impact of the introduction of the NHG guidelines [18] (March 1999) on likelihood of receiving anti-osteoporotic drugs was estimated using a logistic regression, with likelihood of receipt of anti-osteoporotic medication as outcome variable and year of admission, age and gender as covariates. Furthermore, we assessed how and how long patients used anti-osteoporotic drugs after hospital discharge. All analyses were performed using SAS version 8.2 (SAS, Cary, N.C., USA).
Results
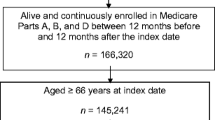
A total of 5323 fracture related hospitalizations were identified from the PHARMO hospital database. After excluding 2490 patients under 50 years of age, follow-up admissions (n=266), 344 hospitalizations due to traffic injuries and 122 hospitalizations due to external force related accidents, 2108 hospitalizations met the inclusion criteria of this study (Table 1). Excluding deceased (n=122) and institutionalized (n=332) patients, 1654 patients were left for analysis (Table 2). Patients were predominantly women (73.1%), and 75 years of age and older (55.9%). Proximal femur fracture (52.7%) was the most frequent reason for hospitalization, while 62.5% of the fractures were considered to be osteoporotic fractures with certainty (Table 1). The median length of stay in the hospital was 14 days.
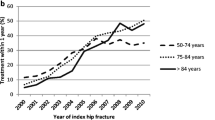
In the 5-year period prior to admission, 291 (17.6%) patients had been dispensed anti-osteoporosis drugs, although only 158 (7.5%) of these patients used any anti-osteoporosis drugs during the 3-month period prior to the admission date, indicating that at least 50% of the patients had discontinued treatment with anti-osteoporosis drugs before hospitalization for the fracture. In total, 247 out of 1654 patients (14.9%) were dispensed anti-osteoporosis drugs within 1 year after discharge from hospital. Patients used several drugs in combination or switched during the year: 113 (6.8%) patients used biphosphonates, 62 (3.7%) patients received estrogens, 96 (5.8%) received calcium and 48 (2.9%) received vitamin D containing preparations. One patient used raloxifene and no patient used sodium fluoride. Of these 247 patients, 163 (66.0%) patients had received anti-osteoporosis prescriptions prior to their index fracture, whereas the remaining 84 patients were new recipients of anti-osteoporosis drugs, yielding a new treatment rate of 84/1654 or 5.1%. A multivariate logistic regression on likelihood of receipt of treatment for osteoporosis revealed that compared to 1998, likelihood of receiving treatment did not change in 1999 [odds ratio (OR): 0.7, 95%CI: 0.5–1.1] or 2000 (OR 0.95; 95% CI: 0.68–1.30).
Women were 3 times more likely to receive treatment with anti-osteoporotic drugs in the year following index fracture as compared to men (OR 3.1; 95% CI: 1.9–5.0), after controlling for other factors (Table 3). Increased treatment rates were also observed for patients 65–84 years of age relative to patients 50–64 years of age and among patients admitted for vertebral fractures as compared to patients admitted for femur fractures (OR 1.9, 95%CI: 1.1–3.4).
No differences in treatment rates were observed with age when the population was restricted to patients never treated with anti-osteoporotic drugs prior to fracture. In this specific group, the treatment rate of vertebral fracture increased to an odds ratio of 3.1 (95% CI: 1.5–6.4) as compared to patients with femur fractures, and 5.4 (95% CI: 2.4–11.9) as compared to patients admitted for fractures considered as unlikely to be osteoporotic. However, less than 50% of these patients used these anti-osteoporosis drugs consistently and consequently in the year of follow-up.
For a sample of 208 out of 1654 cases, GP case records were available. Of these patients, 34 (16.3%) had ever been treated with anti-osteoporotic drugs in the year after discharge from the hospital. Only 11 out of the 208 patients in the GP records had a diagnosis of osteoporosis. Six of them were treated, while five patients remained untreated during the year following discharge. The first entry of all diagnoses was recorded before hospital admission. DXA results were obtained from only two patients.
Discussion
During the period from 1998 to 2000, only 247 out of 1654 patients (14.9%) 50 years and older admitted for treatment of fractures resulting from an accidental fall were prescribed anti-osteoporotic drugs, primarily bisphosphonates. Of these patients, more than 50% discontinued use of anti-osteoporotic drugs before the end of the follow-up year, indicating that compliance was poor. Most of these patients had already been prescribed these drugs in the 5-year period prior to index hospital admission, although more than 50% had stopped anti-osteoporosis drug therapy prior to their fracture. Only 84 patients (5.1%) were treated for the first time with anti-osteoporotic drugs during the year after discharge. The most likely recipients of anti-osteoporotic drugs were women, patients between 65 and 84 years of age and those admitted for a vertebral fracture. Among patients treated with anti-osteoporotic drugs, only about 5% had a formal diagnose of osteoporosis on their medical record.
Several studies reported a prevalence of osteoporosis in the range of 10–20% in the 50 year and older population. Further, considering the increased risk of subsequent fracture for patients with fracture, these patients are an important target for anti-osteoporotic therapy [5, 6, 7, 8]. However, only 13.8% used anti-osteoporosis drugs prior to hospitalization. Although the Dutch GP guidelines suggest that treatment for osteoporosis should be considered for patients suffering an osteoporotic fracture, only 5% of all patients were newly detected and treated with anti-osteoporostic drugs. Also, in the general practitioner case records, evidence of the presence of osteoporosis was rarely recorded. Furthermore, the vertebral fractures in this study all required hospital admission, which underlines the seriousness of these fractures. In prior studies, it has been observed that only about one-third of these vertebral fractures actually come to the clinician’s attention.
These findings suggest that a only a very small proportion of patients with fractures are being treated for osteoporosis, leaving the vast majority of patients after fracture untreated, i.e. at high risk of subsequent fracture. Of those who were treated, at least 50% discontinued treatment, reducing those appropriately treated to less than 7.5%. Further, no evidence was found for improvement in rate of detection or treatment with the introduction of the general practitioner guidelines in 1999. Moreover, and paradoxically, the number of newly treated fracture patients showed a slight decrease over time.
In conclusion, the results of this study suggest that treatment for osteoporosis for post-fracture patients in current practice is still quite appalling. Hospitalization for fractures in current practice is, at least in the period 1998–2000, not considered a major trigger for detection and treatment of osteoporosis.
References
Geusens P, Autier P, Boonen S, Vanhoof J, Declerck K, Raus J (2002) The relationship among history of falls, osteoporosis, and fractures in postmenopausal women. Arch Phys Med Rehabil 83:903–906
Melton LJ 3rd (2001) The prevalence of osteoporosis: gender and racial comparison. Calcif Tissue Int 69:179–181
Tenenhouse A, Joseph L, Kreiger N, Poliquin S, Murray TM, Blondeau L et al. (2000) Estimation of the prevalence of low bone density in Canadian women and men using a population-specific DXA reference standard: the Canadian Multicentre Osteoporosis Study (CaMos). Osteoporos Int 11:897–904
Doube A (1999) Managing osteoporosis in older people with fractures. BMJ 318:477–478
Johnell O, Oden A, Caulin F, Kanis JA (2001) Acute and long-term increase in fracture risk after hospitalisation for vertebral fracture. Osteoporos Int 12:207–214
Klotzbucher C, Ross P, Landman P, Abott TI, Berger M (2000) Patient with prior fractures have an increased risk of future fractures: a summary of literature and statistical synthesis. J Bone Miner Res 15:721–739
Lindsay R, Silverman SL, Cooper C, Hanley DA, Barton I, Broy SB et al. (2001) Risk of new vertabral fracture in the year following a fracture. JAMA 285:320–323
Castel H, Bonneh DY, Sherf M, Liel Y (2001) Awareness of osteoporosis and compliance with management guidelines in patients with newly diagnosed low-impact fractures. Osteoporos Int 12:559–64
McLellan AR (2003) Identification and treatment of osteoporosis in fractures. Curr Rheumatol Rep 5:57–64
Pal B (1999) Questionnaire survey of advice given to patients with fractures. BMJ 318:500–501
al-Allaf AW, Pal B, Reid N (1998) An audit of post fracture rehabilitation with special emphasis on osteoporosis assessment and treatment. Clin Exp Rheumatol 16:451–453
Kamel HK, Hussain MS, Tariq S, Perry HM, Morley JE (2000) Failure to diagnose and treat osteoporosis in elderly patients hospitalized with hip fracture. Am J Med 109:326–328
Torgerson DJ, Dolan P (1998) Prescribing by general practitioners after an osteoporotic fracture. Ann Rheum Dis 57:378–379
Cuddihy MT, Gabriel SE, Crowson CS, Melton LJ 3rd (2002) Osteoporosis intervention following distal forearm fractures. Arch Int Med 162:421–426
Freedman KB, Kaplan FS, Bilker WB, Strom BL, Lowe RA (2000) Treatment of osteoporosis: are physicians missing an opportunity? J Bone Joint Surg [Am] 82-A:1063–1070
Gezondheidsraad: Commissie Osteoporose (1998) Preventie van aan osteoporose gerelateerde fracturen. Gezondheidsraad, Rijswijk
CBO (2002) Osteoporose Tweede Herziene Richtlijn. Kwaliteitsinstituut voor de Gezondheidszorg CBO, Utrecht
Elders PJ, van Keimpema JC, Petri H, Matser A (1999) NHG-standaard Osteoporose. Huisarts Wet 42:115–128
Herings RMC (1993) PHARMO: a record linkage system for postmarketing surveillance of prescription drugs in the Netherlands. Doctorate, Utrecht University
Acknowledgement
This study was supported by Merck & Co. USA.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Panneman, M.J.M., Lips, P., Sen, S.S. et al. Undertreatment with anti-osteoporotic drugs after hospitalization for fracture. Osteoporos Int 15, 120–124 (2004). https://doi.org/10.1007/s00198-003-1544-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-003-1544-7