Abstract
Low calcaneal ultrasound measurement (quantitative ultrasound, QUS) has been shown to predict fractures in elderly women. However, only a few studies have examined its ability to predict perimenopausal and early postmenopausal fractures. We conducted a prospective population-based cohort study to assess the capability of QUS as compared to axial BMD measurement to predict early postmenopausal fractures at that age. Four hundred and twenty-two women (mean age 59.6, range 53.7–65.3) from the Kuopio Osteoporosis Risk Factor and Prevention Study (OSTPRE) were randomly chosen to undergo a calcaneal ultrasound measurement. In all, 9.4% of these women were premenopausal at the time of measurement. Thirty-two follow-up fractures were reported during the mean follow-up of 2.6 years (SD 0.7). These were validated with patient record perusal. Broadband ultrasound attenuation (BUA), speed of sound (SOS) and stiffness index (SI) were significantly lower among women with than without fracture (P-values 0.028, 0.001 and 0.001, respectively). Mean T-score adapted from SI was −1.5 (95% CI −1.7 to −1.2) for fracture group and −1.0 (95% CI −1.1 to −0.9) for the non-fracture group. All QUS measurements predicted fractures even after adjusting for age, weight, height, previous fracture history, femoral neck BMD and use of hormone replacement therapy according to Cox regression. The adjusted hazard ratios (HR, 95% confidence interval) of a follow-up fracture for a 1 SD decrease were 1.80 (1.27–2.56), 1.72 (1.21–2.45) and 1.43 (1.01–2.03) for SOS, SI and BUA, respectively. Similarly, the adjusted HR for a 1 SD decrease of spinal BMD was 1.27 (0.85–1.94) and for that of femoral neck BMD 1.14 (0.78–1.70). In receiver operator analyses, the area under the curve (AUC) was greatest for QUS measurements: SOS (AUC=0.68), stiffness (AUC=0.67), BUA (AUC=0.62) and least for lumbar BMD (AUC=0.56), while and femoral neck BMD (AUC=0.59). The difference between AUCs was statistically significant between SI and lumbar BMD (P=0.02, Duncan’s P=0.07). We conclude that low calcaneal QUS predicts early postmenopausal fractures as well as or even better than axial BMD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis is a systemic skeletal disease characterized by low bone mass and microarchitectural deterioration of bone tissue, thus increasing the risk of fractures [1]. The diagnosis of osteoporosis is commonly based on measurements with dual energy X-ray absorptiometry (DXA), which has been considered as a gold standard [2]. Quantitative ultrasound measurement (QUS) is widely used as a non-ionizing and a low-cost method aimed to diagnose osteoporosis [3]. However, the information value of a single ultrasound measurement for a patient is still controversial and interpretation is more complicated than with central DXA [4]. Prospective studies have shown that low QUS predicts hip fracture and is associated with low bone mineral density (BMD) of the hip as measured by DXA [5, 6, 7]. Moreover, a few prospective studies have studied the ability of calcaneal broadband ultrasound attenuation (BUA) to detect fractures also in perimenopausal women [8, 9, 10]. Stewart et al. found significant association in terms of Odd’s ratios between BUA and fracture risk [8], and Thompson et al. showed that QUS can predict fractures among women over 55 years of age [9]. Gnudi et al. found that patellar ultrasound is a significant predictor of osteoporotic fractures in early postmenopausal women [10]. However, information on the ability of QUS to detect future fractures as compared to BMD during early postmenopausal years is scarce. Our aim was to evaluate how well a single baseline QUS measurement can predict future fractures in early postmenopausal women as compared to femoral or lumbar BMD measurement.
Materials and methods
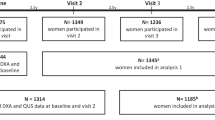
The initial study population consisted of 506 women, a random subsample of 2025 randomly chosen women who participated in the Kuopio Osteoporosis Risk Factor and Prevention Study (OSTPRE) in Kuopio, Eastern Finland. These 506 women were invited to undergo calcaneal ultrasound measurement (Lunar Achilles, Lunar Corporation, Madison, Wisc., USA) at the time of DXA densitometry (Lunar DPX) of the proximal femur and lumbar spine (L2–L4) during 1994–1995. In all, 84 women were excluded from the analyses: 46 did not turn up, seven had died and two had moved from the area; four women could not be measured due to swollen feet and in 24 cases the ultrasound instrument did not work properly. The reasons for these technical hazards in ultrasound measurement could not be fully elucidated. Lunar Achilles was one of the first generation equipments in ultrasound densitometry, and therefore it might have some inherent problems which seem to have been overcome in later generation machines, e.g. in Achilles+. In some patients the machine was unable to get a proper signal, perhaps due to some micro-dust from socks dissolving in water from the skin surface, even although the foot was properly washed before immersion. Thus, 422 women formed the final study cohort. Body weight and height were measured during the bone measurement visit and a questionnaire was used to collect data about previous fractures, use of hormone replacement therapy (HRT), alcohol consumption, smoking and use of dietary calcium. At the end of May 1999, a follow-up questionnaire was sent to the entire cohort in order to acquire data of fractures during the follow-up. Crosschecking radiological reports from medical records was used to validate self-reported fractures. Rib fractures were accepted without radiological evidence based on clinical diagnosis alone. The local ethics committee approved the study design.
Statistical analysis
The first fracture during the follow-up period was the end point event for statistical analyses which were performed using SPSS for Windows software, version 7.5 (Statistical Package for Social Sciences; SPSS Inc.). In univariate analyses, the two-tailed, unpaired Student’s t-test or analysis of variance were used for continuous variables and chi-square statistics for categorical variables. Relative risks were estimated as proportional hazards (HR) with 95% confidence intervals (CI) using the Cox proportional hazards model. The following baseline variables were used as covariates in the Cox model: age, weight, height, femoral neck BMD, previous fracture history and use of HRT. Furthermore, receiver operator characteristic (ROC) analysis was used to identify which measurement of QUS and BMD has the best predictive ability for follow-up fractures. Statistical testing for ROC curves was performed using Roccomp software (Stata/SE 8.0, Stata Base Reference Manual, Volume 3, Stata Corp. College Station, Tex., USA) [11].
Results
During the mean follow-up time of 2.6 years (SD±0.7, range 0.3–4.0 years), 32 women experienced 33 fractures. Nine of these were wrist and nine were ankle fractures (Table 1). In addition, nine fractures were assumed to be high energy fractures and 24 low energy fractures, according to the mechanism of fracture. Characteristics of the study group are presented in Table 2. The only statistically significant differences between the fracture and the non-fracture groups were found in QUS parameters, while differences in the axial bone density were not statistically significant between groups. Mean Z-scores in fracture and non-fracture groups were, respectively, for BUA −0.37, 0.03, for SOS −0.58, 0.05, for SI −0.55, 0.04, for spinal BMD −0.21, 0.02 and for femoral neck BMD −0.27, 0.02. Furthermore, QUS measurement expressed in terms of mean T-score in the fracture group was −1.5 (95% CI −1.7 to −1.2) and in the non-fracture group −1.0 (95% CI −1.1 to −0.9).
When the study subjects were categorized into tertiles according to QUS and BMD values, the distribution of follow-up fractures was different for each parameter (Fig. 1). Most fractures were cumulated in the lowest tertile of SOS and stiffness, while in the highest tertile of BUA the number of fractures was the least. In order to find clinically relevant threshold values to judge how well an individual measurement separates fractured women from non-fractured ones, we chose cut-off values at −1 SD below the group mean (Z-score −1.0) and at the group mean (Z-score 0.0) (Table 3). Using −1 SD as a cut-off value, only a minority (15.6–40.6%) of fractured women belonged in the group below −1 SD. However, women below the group mean experienced the most fractures (50.0–71.9%) during follow-up. In ROC analyses, the largest area under the curve was shown by SOS (AUC=0.68) and the least area by lumbar BMD (AUC=0.56) (Fig. 2). Nevertheless, statistically significant differences were found only between areas of SOS and spinal BMD (P=0.03, Duncan’s P=0.13) and between SI and spinal BMD (P=0.02, Duncan’s P=0.07).
The number of ankle fractures was highest in the lowest SOS and stiffness tertiles, which in all cases seemed to be more sensitive in discriminating ankle fractures as compared to BUA and axial BMD. On the contrary, wrist fractures were equally distributed in BUA, SOS, stiffness and lumbar BMD tertiles. However, the number of wrist fractures was highest in the lowest tertile of femoral neck BMD, although the difference between tertiles was non-significant. Previous fracture was not an independent predictor of fracture; six women (18.8%) in the fracture group and 86 women (22.1%) in the non-fracture group had experienced at least one fracture before baseline measurements.
A backward stepwise Cox regression analysis was performed to evaluate the relative risk of fracture per 1 SD change in QUS and BMD measurements (Table 4). After adjusting for confounding variables, the hazard ratio (HR, 95% confidence interval) of a follow-up fracture for a 1 SD decrease was 1.80 (1.27–2.56), 1.72 (1.21–2.45) and 1.43 (1.01–2.03) for SOS, stiffness and BUA, respectively. Similarly, HR for a 1 SD decrease in spinal BMD was 1.27 (0.85–1.94) and for femoral neck BMD 1.14 (0.78–1.70). All QUS parameters predicted fracture independently of BMD. In the main analyses, traumatic fractures were not excluded to elucidate the value of a single measurement in predicting a future fracture per se. However, when Cox’s analyses were performed taking only low-energy fracture as an end-point variable, the results remained unchanged for QUS and BMD measurements (Table 5).
In power analyses, we used unadjusted hazard ratios for QUS and BMD measurements to find out whether our sample size was large enough to detect the associations. For given hazard ratios, a sufficient number to detect associations for BUA was 740, for SOS 274, for stiffness 303, for femoral neck BMD 1543 and for spinal BMD 699 (Hintze 2001; NCSS and PASS. Number Cruncher Statistical Systems. Kaysville, Utah, USA, www.ncss.com).
Discussion
The present study verified that calcaneal QUS is able to predict early postmenopausal fractures as well as or even better than axial BMD. A 1 SD decrease in BUA values increased the risk of future fracture by 43%, which equaled the risk of 1 SD decrease in spinal BMD. Furthermore, only QUS measurements were found to predict fractures after adjusting for confounding factors. Our results are comparable with the prospective study by Thompson et al. [9], in which a 1 SD decrease in BUA resulted in 40% increase in fracture risk in 3150 women aged 45–75 years. Similarly, Stewart et al. showed that 1 SD reduction in BUA in 1000 perimenopausal women aged 45–49 years predicted a follow-up fracture by an odds ratio of 1.4 (95% CI 1.2–2.4), although there were no statistically significant differences in the mean BUA values between the fracture and the non-fracture groups [8]. In a more recent study by Gnudi et al., a low patellar ultrasound measurement increased the risk of fracture by an RR of 2.89 (95% CI 1.12–7.42) for a 1 SD decrease [10]. In the elderly, low ultrasound measurement has also been shown to be associated with elevated hip fracture risk [6, 7, 12] and with other non-spinal fracture risk [12].
In the present study, adjusting for BMD did not change the ability of QUS measurement in prediction of fracture. This is in agreement with the assumption that ultrasound measurement also reflects other components of bone strength than BMD [13]. Interestingly, adjusting BMD for QUS parameters seemed to dilute the effect of BMD in fracture prediction. Possibly the inability of BMD to predict a fracture in the present study was due to the small sample size, as shown in the power analyses. Evidence from previous studies has shown that low BMD is a prominent and independent predictor of perimenopausal fractures [14, 15, 16, 17, 18]. However, according to our results, one could also speculate that peripheral QUS might discriminate peripheral fractures more accurately than axial BMD measurements. This could be explained by site specificity, i.e. calcaneal QUS is more sensitive for changes in bone quality or composition close to the measurement site than axial BMD. The majority of the follow-up fractures in this study were wrist or ankle fractures (56%) and there were only three vertebral and three pelvic fractures. As a consequence, peripheral measurements could be preferable in detecting (peripheral) fractures during the early postmenopausal period. Moreover, similar risk ratios for fractures as reached from calcaneal QUS could be expected from calcaneal BMD measurement [6]. Whether the decision to start treatment for osteoporosis could be based solely on peripheral ultrasonographic measurement is, however, unclear and needs further studies.
The follow-up fractures that were included in each QUS and BMD tertiles were partially different, highlighting the fact that different patients were identified according to the technique. This poses a question on how to interpret QUS results in the light of axial BMD, which is considered the gold standard in osteoporosis diagnosis and treatment. In a study by Blake and Fogelman, differences in axial and peripheral densitometry were evaluated, and indicated that different techniques identify different patients and there is no absolute method of identifying all fracture patients [19]. Therefore, it may be unwise to calibrate peripheral QUS to fit in the results of axial BMD.
Notwithstanding the results, the overall performance of axial and peripheral measurements to find fracture cases seems to be far from perfect. There are still a great number of fracture cases who do not have either low QUS or low BMD values. In the ROC analyses, areas under curves are fairly modest, indicating the inaccuracy of these methods. In other words, women with low QUS or BMD (i.e. value below −1 SD of the group mean) experienced only a minority of fractures. However, if the group mean was used as a threshold, women who belonged to the lower part sustained the majority of fractures. Thus, choosing a cut-off value close to the mean would lead to a more complete detection of fracture candidates. This finding is in agreement with our earlier study, in which we found a threshold point of 0.64 SD below the mean in the axial BMD to offer the best cut-off point to discriminate between the fracture and non-fracture patients [16]. Even so, moving the cut-off point closer to the mean increases the number of false positives. In terms of T-score adapted from stiffness values, the mean T-score was −1.5 for the fracture group and −1.1 for the non-fracture group in our present study. Thus, a cut-off point of T-score −1.2 might provide a useful threshold in clinical practice to discriminate between increased and normal fracture risk.
The strengths of this study include the prospective population-based design and a well-defined cohort of early postmenopausal women, which is a clinically interesting group. However, the main limitations of our study are the low number of fractures as well as the relatively small sample size and short follow-up time resulting in diminished study power. According to power calculations, however, the sample size seemed to be large enough to explain the statistically significant results of stiffness and SOS measurements. On the other hand, for our BMD and BUA results, study power may not be sufficient. This also explains why a historical fracture which has previously been shown to strongly predict future fractures [16, 17, 20] had no effect on follow-up fractures in this study. Moreover, the study subjects consisted only of Caucasian women; the interpretation should not be applied to men, to other races or to women in other age groups. We used a water-coupled device (Lunar Achilles), but according to the study of Njeh et al. [21], our results could be applied with caution to other water-coupled and also gel-coupled devices.
In conclusion, low calcaneal QUS is an independent predictor of fracture in perimenopausal and early postmenopausal women. Our results suggest that the predictive ability of calcaneal QUS is similar or even better than that of axial BMD. The risk of fracture increases after QUS cut-off value T-score −1.2 (adapted from stiffness). It seems that early postmenopausal women might benefit more from peripheral than axial measurements when searching for potential fracture candidates in the short term. Thus, calcaneal QUS can be recommended as a method to assess fracture risk in early postmenopausal women.
References
Consensus development conference (1993) Diagnosis, prophylaxis, and treatment of osteoporosis. Am J Med 94:646–650
Kanis JA, Delmas P, Burckhardt P, Cooper C, Torgerson D (1997) Guidelines for diagnosis and management of osteoporosis: the European Foundation for Osteoporosis and Bone Disease. Osteoporos Int 7:390–406
Njeh CF, Boivin CM, Langton CM (1997) The role of ultrasound in the assessment of osteoporosis: a review. Osteoporos Int 7:7–22
Miller PD, Njeh CF, Jankowski LG, Lenchik L (2002) International Society for Clinical Densitometry Position Development Panel and Scientific Advisory Committee. What are the standards by which bone mass measurement at peripheral skeletal sites should be used in the diagnosis of osteoporosis? J Clin Densitom 5:S39–45
Porter RW, Miller CG, Grainger D, Palmer SB (1990) Prediction of hip fracture in elderly women: a prospective study. BMJ 29:638–641
Bauer DC, Gluer CC, Cauley JA, Vogt TM, Ensrud KE, Genant HK et al. (1997) Broadband ultrasound attenuation predicts fractures strongly and independently of densitometry in older women. A prospective study. Study of Osteoporotic Fractures Research Group. Arch Int Med 157:629–634
Hans D, Dargent-Molina P, Schott AM, Sebert JL, Cormier C, Kotzki PO et al. (1996) Ultrasonographic heel measurements to predict hip fracture in elderly women: the EPIDOS prospective study. Lancet 348:511–514
Stewart A, Torgerson DJ, Reid DM (1996) Prediction of fractures in perimenopausal women: a comparison of dual energy X-ray absorptiometry and broadband ultrasound attenuation. Ann Rheum Dis 55:140–142
Thompson PW, Taylor J, Oliver R, Fisher A (1998) Quantitative ultrasound (QUS) of the heel predicts wrist and osteoporosis-related fractures in women age 45–75 years. J Clin Densitom 1:219–225
Gnudi S, Ripamonti C, Malavolta N (2000) Quantitative ultrasound and bone densitometry to evaluate the risk of nonspine fractures: a prospective study. Osteoporos Int 11:518–523
Hanley JA, McNeil BJ (1983) A method of comparing the areas under receiver operating characteristic curves derived from the same cases. Radiology 1148:839–843
Pluijm SM, Graafmans WC, Bouter LM, Lips P (1999) Ultrasound measurements for the prediction of osteoporotic fractures in elderly people. Osteoporos Int 9:550–556
Bouxsein ML, Radloff SE (1997) Quantitative ultrasound of the calcaneus reflects the mechanical properties of calcaneal trabecular bone. J Bone Miner Res 12:839–846
Honkanen R, Kroger H, Tuppurainen M, Alhava E, Saarikoski S (1995) Fractures and low axial bone density in perimenopausal women. J Clin Epidemiol 48:881–888
Kroger H, Huopio J, Honkanen R, Tuppurainen M, Puntila E, Alhava A, Saarikoski S (1995) Prediction of fracture risk using axial bone mineral density in a perimenopausal population: a prospective study. J Bone Miner Res 10:302–306
Huopio J, Kroger H, Honkanen R, Saarikoski S, Alhava E (2000) Risk factors for perimenopausal fractures. A prospective study. Osteoporos Int 11:219–227
Torgerson DJ, Campbell MK, Thomas RE, Reid DM (1996) Prediction of perimenopausal fractures by bone mineral density and other risk factors. J Bone Miner Res 11:293–297
Tuppurainen M, Kroger H, Honkanen R, Puntila E, Huopio J, Saarikoski S et al. (1995) Risks of perimenopausal fractures—a prospective population-based study. Acta Obstet Gynecol Scand 74:624–628
Blake GM, Fogelman I (2001) Peripheral or central densitometry: does it matter which technique we use? J Clin Densitom 4:83–96
Cauley JA, Thompson DE, Ensrud KC, Scott JC, Black D (2000) Risk of mortality following clinical fractures. Osteoporos Int 11:556–561
Njeh CF, Hans D, Li J, Fan B, Fuerst T, He YQ, Tsuda-Futami E, Lu Y, Wu CY, Genant HK (2000) Comparison of six calcaneal quantitative ultrasound devices: precision and hip fracture discrimination. Osteoporos Int 11:1051–1062
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Huopio, J., Kröger, H., Honkanen, R. et al. Calcaneal ultrasound predicts early postmenopausal fractures as well as axial BMD. A prospective study of 422 women. Osteoporos Int 15, 190–195 (2004). https://doi.org/10.1007/s00198-003-1534-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-003-1534-9