Abstract
Introduction
Urinary voiding dysfunction is a common postpartum condition. Increased knowledge of risk factors for postpartum urinary retention could improve early identification of women at risk and lead to enhanced postpartum surveillance. We sought to identify intrapartum factors that contribute to postpartum urinary retention.
Methods
This retrospective case-control study compared subjects who developed postpartum urinary retention requiring indwelling catheterization after vaginal delivery to a control group who did not require catheterization. The control group was randomly selected in a 1:4 ratio. Continuous data were analyzed using a two-sample t-test and Mann-Whitney U test. Categorical data were analyzed using Fisher’s exact test and two proportions test. Logistic regression was performed to identify variables independently associated with increased risk for development of postpartum urinary retention.
Results
A total of 5802 women who delivered vaginally met eligibility criteria with 38 women (0.65%) experiencing postpartum urinary retention. Logistic regression revealed that nulliparity, ≥ 2nd-degree obstetrical laceration, and intermittent catheterization during labor were independently associated with increased risk for postpartum urinary retention.
Conclusion
No single factor predicted development of postpartum urinary retention; however, a higher index of suspicion after vaginal delivery is warranted for nulliparous women, ≥ 2nd-degree obstetrical laceration, and if intermittent catheterization during labor was required.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Urinary voiding dysfunction is a common postpartum condition. The reported prevalence range of voiding dysfunction is wide and varies from 0.05% to 45% because of no standardized definitions [1,2,3]. Voiding dysfunction can present as minor incomplete bladder emptying [4] to complete inability to void or urinary retention. In 2016, there were 3,945,875 registered births in the US, and of those 2,760,047 were vaginal deliveries [5]. Supposing the lowest prevalence of urinary voiding dysfunction affects these vaginal deliveries, > 1380 women per year suffer from overt postpartum urinary retention or the inability to void associated with discomfort [1, 6]. Postpartum urinary retention warrants heightened recognition and treatment to avoid bladder overdistension injury.
Normal bladder capacity in women ranges from 400 to 600 ml [7, 8]. Overdistension injury can occur during situations of prolonged bladder filling such as labor, particularly with use of neuraxial anesthesia if monitoring and bladder catheterization are not performed in a timely fashion [9]. Overdistension injuries can lead to bladder denervation, detrusor atony, and future voiding dysfunction [9, 10].
Previous studies have investigated factors that increase the risk of postpartum urinary retention [1, 10,11,12,13,14]. However, few studies have focused on intrapartum factors leading to the development of postpartum urinary retention (10). Increased knowledge of risk factors leading to postpartum urinary retention could improve the early identification of women at risk and lead to enhanced postpartum surveillance. The objective of our study was to identify intrapartum factors that contribute to postpartum urinary retention.
Materials and methods
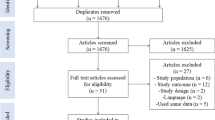
This retrospective case-control study compared women who experienced postpartum urinary retention to controls who delivered at a community-based, academic-affiliated hospital. This study was deemed institutional review board exempt (Atlantic Health System IRBNet ID 1162717-1). Cases of postpartum urinary retention were defined as women who required indwelling catheterization after delivery because of inability to void. Controls were selected from the pool of women who did not require any form of catheterization after delivery and were chosen in a 1:4 case-control ratio. Inclusion criteria consisted of all women who delivered vaginally between July 2015 and June 2017. Women were excluded if they underwent cesarean delivery, had a multiple gestation pregnancy, or had an indwelling catheter placed during their intrapartum or postpartum period for reasons other than urinary retention.
We evaluated intrapartum variables including: prolonged second stage of labor; use of misoprostol or intracervical balloon catheter for cervical ripening; use of oxytocin for labor induction or augmentation; neuraxial analgesia during labor; episiotomy performed; second-degree or greater obstetrical laceration; operative vaginal delivery with forceps or vacuum; use of intermittent catheterization during labor; use of continuous catheterization during labor; maximum intrapartum bladder volume ≥ 600 ml. Prolonged second stage of labor was defined as a duration ≥ 4 h. Maximum bladder volume ≥ 600 ml was chosen as 600 ml is generally considered the upper limit of normal bladder capacity in women.
Data were obtained through electronic health record review and recorded in the REDCap electronic data collection system (Vanderbilt University, Nashville, TN). All eligible cases during the study time frame were included. For every case, four controls were randomly selected from the pool of women who met eligibility criteria. Randomization of controls was completed by an online random number generator (https://www.randomlists.com/random-numbers) after the cases were removed from the pool of eligible participants.
Continuous data were analyzed using two-sample t-test and Mann-Whitney U test. Univariate analysis was performed on intrapartum variables. Logistic regression was performed to identify variables independently associated with increased risk for development of postpartum urinary retention. Missing data points were excluded from analysis. Statistical analysis was performed using Minitab 17 Statistical Software (State College, PA: Minitab, Inc.).
Results
From July 2015 to June 2017, 5802 women delivered vaginally at our institution and met eligibility criteria. Thirty-eight women (0.65%) experienced urinary retention requiring an indwelling catheter after their delivery; 152 women were randomly selected to constitute the control group.
Table 1 includes baseline characteristics. More cases were nulliparous than controls. Maternal age and neonatal birth weight had a statistical difference; however, the difference has no clinical relevance.
Univariate analysis of intrapartum variables showed use of oxytocin for labor induction or augmentation, induction with misoprostol or intracervical foley balloon, epidural use, and second-degree or greater obstetrical laceration were significant (Table 2). Operative vaginal delivery also increased the risk of postpartum urinary retention development; however, when this category was further subdivided, we found that only use of forceps increased the risk for postpartum urinary retention. There was no significant difference in the second stage of labor lasting ≥ 4 h, episiotomy, use of continuous catheterization, or women with a maximum intrapartum bladder volume ≥ 600 ml between cases and controls.
Logistic regression revealed that nulliparity, ≥ 2nd-degree obstetrical laceration, and use of intermittent catheterization in labor were independently associated with increased risk for development of postpartum urinary retention with a correlation coefficient of 0.3.
Discussion
Postpartum urinary retention requiring in-dwelling catherization was uncommon after vaginal delivery in our population, with an overall incidence of 0.65%. We did not find a single intrapartum factor that accurately predicted women who experienced postpartum urinary retention requiring in-dwelling catheterization.
Rather than looking for one marker to predict which women may experience postpartum urinary retention, clinicians should assess a combination of factors to flag patients for close monitoring of postpartum voiding dysfunction. We found nulliparity to be associated with increased risk for postpartum urinary retention. Clearly, nulliparity is not a modifiable risk factor; however, it may be used as a criterion to prompt providers to monitor postpartum urine output in this population to avoid complications related to bladder overdistention. Furthermore, ≥ 2nd-degree laceration was also found to independently increase the risk for postpartum urinary retention. This was common in subjects overall but was found to be more common in cases. Additionally, the use of intermittent catheterization in labor was found to increase the risk of postpartum urinary retention and was noted to be statistically significant; however, this result is difficult to clinically implement as a screening factor since almost half of the control group underwent intermittent catheterization as well. These variables are consistent with findings from other similar studies evaluating risk factors for postpartum urinary retention [10].
Nulliparity, ≥ 2nd-degree perineal laceration, and intermittent catheterization during labor all occurred too often in controls to be used as accurate predictors of those who will develop postpartum urinary retention. The fact that these three variables were not rare in the control group provides a low sensitivity in order to use these variables as strict screening guidelines. Ideally, screening criteria are accurate enough to detect conditions early; however, real-world circumstances are not always idyllic or we may not have enough information to make precise determinations. Regarding postpartum urinary retention, we recommend providers use the aforementioned variables to maintain a higher index of suspicion for patients that may be at higher risk for this disorder, especially for women who have all three risk factors.
The strengths of the study include a robust case control with clear case selection criteria and a 1:4 case-control ratio. Due to our clear definition of urinary retention as an inability to urinate requiring postpartum indwelling catheterization, we were able to focus on a group of women who are at the highest risk of bladder distention injury, which is not the case with many prior studies. Postpartum urinary retention has a low prevalence; therefore, this study provides further insight into predicting which patients may be at risk for developing postpartum urinary retention.
We recognize this study has limitations including bias inherent to the retrospective study design. Furthermore, these risk factors for postpartum urinary retention may differ or affect women to varying degrees in other patient populations.
Postpartum urinary retention requiring in-dwelling catheterization is uncommon and is likely caused by a multitude of factors. Obstetrical providers should have a higher index of suspicion for women who delivered vaginally and are nulliparous, sustained an obstetrical laceration ≥ 2nd degree, and required intermittent catheterization during labor. These three factors can be used as a screening tool but they cannot accurately predict those who will develop postpartum urinary retention. The importance of this study is to increase awareness of postpartum urinary retention and avoid negative long-term effects if left untreated such as bladder overdistension injury. Further prospective studies are warranted to elucidate risk factors and potential interventions for postpartum urinary retention.
References
Teo R, Punter J, Abrams K, Mayne C, Tincello D. Clinically overt postpartum urinary retention after vaginal delivery: a retrospective case-control study. Int Urogynecol J Pelvic Floor Dysfunct. 2007.
Yip SK, Brieger G, Hin LY, Chung T. Urinary retention in the post-partum period. The relationship between obstetric factors and the post-partum post-void residual bladder volume. Acta Obstet Gynecol Scand. 1997.
Mulder FEM, Hakvoort RA, Schoffelmeer MA, Limpens J, Van Der Post JAM, Roovers JPWR. Postpartum urinary retention: a systematic review of adverse effects and management. Int Urogynecol J. 2014.
Mulder FEM, Rengerink KO, van der Post JAM, Hakvoort RA, Roovers JPWR. Delivery-related risk factors for covert postpartum urinary retention after vaginal delivery. Int Urogynecol J. 2016.
Martin JA, Hamilton BE, Osterman MJKS, Driscoll AK, Drake P. Births: final data for 2016 National Vital Statistics Reports. Natl Vital Stat Rep. 2018;67(1):1–55.
Yip SK, Brieger G, Hin LY, Chung T. Urinary retention in the post-partum period. The relationship between obstetric factors and the post-partum post-void residual bladder volume. Acta Obstet Gynecol Scand. 1997;76:667–72.
Lamonerie L, Marret E, Deleuze A, Lembert N, Dupont M, Bonnet F. Prevalence of postoperative bladder distension and urinary retention detected by ultrasound measurement. Br J Anaesth. 2004;92:544–6.
Afraa TA, Al Afraa T, Mahfouz W, et al. Normal lower urinary tract assessment in women: I. Uroflowmetry and post-void residual, pad tests, and bladder diaries. Int Urogynecol J. 2012;23:681–5.
Madersbacher H, Cardozo L, Chapple C et al. What are the causes and consequences of bladder overdistension?: ICI-RS 2011. Neurourol Urodyn. 2012.
Pifarotti P, Gargasole C, Folcini C, et al. Acute post-partum urinary retention: analysis of risk factors, a case-control study. Arch Gynecol Obstet. 2014;289(6):1249–53.
Cavkaytar S, Kokanali MK, Baylas A, Topcu HO, Laleli B, Tasci Y. Postpartum urinary retention after vaginal delivery: Assessment of risk factors in a case-control study. J Turkish Ger Gynecol Assoc. 2014.
Carley ME, Carley JM, Vasdev G et al. Factors that are associated with clinically overt postpartum urinary retention after vaginal delivery. Am J Obstet Gynecol. 2002.
Kekre AN, Vijayanand S, Dasgupta R, Kekre N. Postpartum urinary retention after vaginal delivery. Int J Gynecol Obstet. 2011.
Musselwhite KL, Faris P, Moore K, Berci D, King KM. Use of epidural anesthesia and the risk of acute postpartum urinary retention. Am J Obstet Gynecol. 2007.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Charbel Salamon, MD, is a consultant for Boston Scientific and Intuitive Surgical. Andrea M. Avondstondt, MD, and Ryan Hidalgo, MD, declare that they have no conflicts of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Avondstondt, A.M., Hidalgo, R.J. & Salamon, C.G. Intrapartum risk factors for postpartum urinary retention: a case-control study. Int Urogynecol J 31, 2395–2398 (2020). https://doi.org/10.1007/s00192-020-04378-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-020-04378-2