Abstract
Introduction and hypothesis
Management of a recurrent urogenital fistula is very challenging and requires experienced surgeons. The aim of this study was to describe the characteristics, success rates, and associated factors related to surgical repairs of patients with recurrent urogenital fistulas by an experienced team at a fistula centre in Nigeria.
Methods
This was a retrospective cohort study of 154 patients that had repeat urogenital fistula repairs at the National Obstetric Fistula Centre, Abakaliki, Nigeria, between January 2014 and December 2016. Information was retrieved from their hospital records. Successful repair was defined by continent status at 3 months after repair. Data were analyzed with SPSS version 20 by IBM Inc., and p < 0.05 was taken as statistically significant. Chi-square test was used to determine the association between the factors and successful repair.
Results
The mean age was 36.27 ± 12.96 years. Obstetric fistula occurred in 92.2% of the patients. The success rates for the first, second, third, and fourth repeat repairs were 68.8%. 56.2%, 50%, and 0% respectively. Significant factors were the number of previous attempts at repair (χ2 = 20.44, p = 0.002), age group (χ2 = 16.95, p = 0.03), Waaldijk’s classification (χ2 = 13.31, p = 0.04), duration of fistula (χ2 = 19.6, p = 0.03), surgeons’ experience (χ2 = 7.11, p = 0.04), and place of previous attempt at repair (χ2 = 6.35, p = 0.02). There were no complications in 86.4%.
Conclusions
The success rate was good. Patients who had previous failed repairs at the fistula centre had better outcomes after the repeat surgeries. Centralizing fistula care will enhance optimal outcomes. It may also boost training and research in this specialty.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
An urogenital fistula is an abnormal opening between the genital and urinary systems [1]. Vesicovaginal fistula (VVF) is the most common urogenital fistula, and it is seen in the developing world largely because of obstructed labour unlike the scenario in developed countries in which it usually follows surgical procedures, gynaecological cancers, and irradiation [1, 2]. The mainstay of management of genitourinary fistula is surgical repair [3]. The first successful repairs were documented by James Marion Sims in 1852, and there have been improvements in fistula repair since then, especially from the mid-twentieth century [2, 4]. VVF repair however remains technically challenging despite these advances [2]. At times, when the fistula is closed, up to one-third of women continue to experience incontinence due to weakened or damaged pelvic floor musculature [5, 6].
Success of repair depends on adherence to basic principles, including pre-operative evaluation, good visualization, good dissection, good haemostasis, resection of devascularized tissue, excision of surrounding fibrous tissue and removal of a foreign body, tension-free approximation of fistula edges, water tight closure, and adequate post-operative urinary drainage [2, 7,8,9].
It is well documented that the success rate is higher at the first attempt than repeat procedures [10,11,12]. In Cameroon, success rates of 72.5%, 69.2, and 41.1% at the first, second, and third attempts respectively were documented [13]. Failures were significantly associated with complete or partial urethral destruction, fibrosis of the fistula edges, severe vaginal scarring, small bladders, size and circumferential involvement [13, 14]. The main complications of fistula repair are recurrent fistula formation, ureteric injury or obstruction and vaginal stenosis. Recurrent fistulas are initially managed conservatively with bladder catheterization and observation. A further repair may be undertaken after resolution of the inflammatory response to the initial procedure [2]. Furthermore, it has also been documented that optimum results are more likely if repair is carried out by surgeons well versed in available techniques because an association between workload and outcome has been established [10, 15]. The aim of this study was to describe the characteristics, success rates, and associated factors of repeat surgical repairs of genitourinary fistulae by an experienced team at a fistula centre in Nigeria.
Methodology
This was a retrospective cohort study involving recurrent urogenital fistula patients that had repeat surgical repair at the National Obstetric Fistula Centre (NOFIC), Abakaliki, Nigeria, between January 2014 and December 2016. NOFIC Abakaliki is one of the specialized fistula centres in Nigeria; it repairs over 500 fistulas per year. The hospital is also involved in prevention of fistulas and rehabilitation of the women following successful fistula closure. The inclusion criterion was previous failed urogenital fistula repair, while the exclusion criterion was incomplete medical records. A Foley urethral catheter was left to drain for 14 days, and the patient was examined with a dye test before discharge from the hospital. A dye test was done by backfilling the bladder using a Foley urethral catheter with fluid dyed with methylene blue. Prophylactic antibiotics were given for 7 days. Patients are usually discharged after the repeat dye test and given a 3-month appointment for follow-up. Successful repair was defined by continent status at 3 months after repair. Ethical clearance was obtained from the Ethics and Research Committee of NOFIC, Abakaliki. Of the 167 patients that had repeat urogenital fistula repairs, 154 (92.2%) records were available for review. The study proforma was filled out using the patients’ hospital records. The proforma included the biodata, history of index delivery, fistula, previous treatment, index surgical repair, and outcome. The fistulas were classified according to Waaldijk’s classification [16].
Data were analyzed with SPSS version 20 by IBM Inc., and p < 0.05 was taken as statistically significant. Means and standard deviations were used to summarize continuous variables while frequency and percentages were used for discrete variables. Chi-square test was used to determine the association between the factors and successful repair.
Results
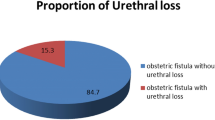
A total of 154 patients were reviewed during the study period. The age of the patients ranged from 8 to 70 years. The mean age was 36.27 ± 12.96 years and the mean parity was 2.45 ± 1.99. The baseline characteristics of the patients are shown in Table 1. The majority of patients had only one previous attempt at repair while only one had four previous attempts at repair (Table 1). Obstetric fistula was the most common aetiology (92.2%) while congenital malformation, hysterectomy, and insertion of caustic substances accounted for the remaining 7.8% (Table 1). According to Waaldijk’s classification, half of the patients were type I while type IIa in which the closing mechanism is affected accounted for the minority.
Of the 154 patients reviewed, 99 (64.3%) achieved continence, 20 (13%) were incontinent despite closed fistula, and the fistulas were not closed in the remaining 35 (22.7%) patients. The success rates for the first, second, third, and fourth repeat repairs were 68.8%. 56.2%, 50, and 0% respectively. The patient with four previous failed repairs subsequently had urinary diversion because she was incontinent despite the fistula being closed (Table 2). Continence was also achieved in 67.5%. 60.7%, 55, and 88.9% of patients with type I, type IIa, type IIb, and type III fistula respectively (Table 2).
Associations between some factors and outcome of the repairs were statistically significant (Table 2). Number of previous attempts at repair (χ2 = 20.44, p = 0.002), age group (χ2 = 16.95, p = 0.03), classification (χ2 = 13.31, p = 0.04), duration of fistula (χ2 = 19.6, p = 0.03), surgeons’ experience (χ2 = 7.11, p = 0.04), and place of previous attempt at repair (χ2 = 6.35, p = 0.02) were significantly associated with success. On the other hand, presence of fibrosis around the fistula was not significant (χ2 = 4.65, p = 0.79).
The majority of patients had no complications (Table 3). The complication rate was 13.6% and it included ureteric ligation (1.3%), haemorrhage that warranted blood transfusion (2.6%), sepsis (2.6%), cervical stenosis (2.6%), gynaetresia (2.6%), urinary tract infection (1.3%), and anaesthetic complication (0.6%). There was no mortality.
Discussion
This review involved a wide range of patients from young girls with congenital fistulas to elderly women who had been living with fistulas for more than 30 years. This implies that urogenital fistula is a condition that afflicts women from the cradle to the grave. The highest frequency age group was 21–30 years, comparable to studies from Port Harcourt, Nigeria [17, 18], and Sagamu, Nigeria [19]. The highest frequency parity was also primiparity as documented in previous Nigerian studies [17, 19]. Obstetric fistula was the most common in this study in keeping with findings from low-resourced settings [5, 17]. This tragedy usually occurs during the first parous experience in these women as a consequence of obstructed labour.
The success rate of repeat fistula repairs in this fistula centre was comparable to documented success rates in other hospitals [13]. The success rates deteriorated significantly with increasing numbers of previous attempts at repair. Tebeu et al. documented success rates of 69.2 and 49.1% with second and third attempts at repair in Cameroon [13]. The best attempt to repair urogenital fistula is the first attempt as demonstrated by previous studies [20]. The lowest success rate was found in type IIb of Waaldjk’s classification. This group was made up of those that required urethral reconstruction with the repair. This could be attributed to the fact that some of these surgeries were staged repairs in which the surgical repairs were carried out in two or more stages before achieving continence.
The continence rates reduced with increasing age in this review [21, 22]. Age-related differences in wound healing have been clearly documented in the literature. Although this significant difference in the success rates could not be unrelated to pre-existing medical conditions in the elderly, many of the processes involved in wound healing are delayed in the elderly [22]. Age is also a predisposing factor to urinary incontinence, which may be due to loss of an intrinsic continence mechanism independent of repair [23]. Patient age and duration between the onset of fistula and repair were however not significantly related to outcome of repair in a review by Jeremy et al. [24]. This difference could be attributed to the smaller sample size compared with the index review. The significant association between the duration of onset of fistula and repair and outcome could be related to the number of previous repairs because fistulas with longer duration were more likely to have had previous attempt(s) at repair.
Waaldijk’s classification essentially classified fistulas according to complexity and involvement of continence mechanisms, both of which have been regarded as prognostic factors for the outcome of fistula repair. It is therefore not surprising that Waaldijk’s classification was significantly related to the success rates in this review [25]. Patients that had previous failed repair at this fistula centre were significantly more likely to achieve continence after a repeat repair at this centre. This finding may be because some of these repairs were staged procedures. Also, subsequent repairs could be made by the same surgeon or a more experienced surgeon. This study also showed better outcomes among surgeons with more experience. These observations support the proposal that fistulas should be managed at specialized centres for better outcomes [15, 26]. It has also been observed that a volume-outcome relationship may exist in fistula repair like in other specialties [15]. Centralizing the care of fistula patients will provide them with high-quality care by experienced surgeons, multidisciplinary care, and optimal outcomes. It may also boost training and research in this field.
The documented complications were similar in type and incidence to those in previously reported studies [17, 24]. The complication rate was comparable to 11.8% reported by Gupta et al. for repeat vesicovaginal fistula repairs in India [27].
We have described the patients’ characteristics and outcomes of repeat surgical repairs of urogenital fistulas in Abakaliki, Nigeria. Most reviews were usually on all surgical repairs of all fistulas but this study described patients with previous failed repairs, which are usually difficult to treat. The weakness of this study was the small sample size and inability to retrieve information for all the patients because it was a retrospective study.
The continence rate in this review was good but there could be improvements. Patients who had previous failed repairs at the fistula centre had better outcomes after the repeat surgeries because subsequent repairs were planned with the benefits of hindsight. Centralization of fistula care to ensure multidisciplinary care and optimal outcomes may be the way forward in fistula care of complex cases.
References
Frajzyngier V, Li G, Larson E, Ruminjo J, Barone MA. Development and comparison of prognostic scoring systems for surgical closure of genitourinary fistula. Am J Obstet Gynecol. 2013;208(2):112.
Williams S. Vesicovaginal fistula. BJUI. 1999;83(5):564–70.
Lee AL, Symmonds RE, Williams TJ. Current status of genitourinary fistula. Obstet Gynecol. 1988;72:313–9.
Sims JM. On the treatment of vesicovaginal fistula. Am J Med Sci. 1852;23:59–82.
Wilson SM, Sikkema KJ, Watt MH, Masenga GG, Mosha MV. Psychological symptoms and social functioning following repair of obstetric fistula in a low-income setting. Matern Child Health J. 2016;20(5):941–5.
Browning A, Menber B. Women with obstetric fistula in Ethiopia: a 6-month follow up after surgical treatment. BJOG Int J Obstet Gynaecol. 2008;115:1564–9.
Kapoor R, Ansari MS, Singh P, Gupta P, Khurana N, Mandhani A, et al. Management of vesicovaginal fistula: an experience of 52 cases with a rationalised algorithm for choosing the transvaginal or transabdominal approach. Indian J Urol. 2007;23(4):372–6.
Qadir T, Ghaffar N, Baloch SN, Muneer A. Clinical pattern and outcome of vesicovaginal fistula. JRMC. 2014;18(2):270–3.
Couvelaire R. Reflections on a personal statistics of 136 vesicovaginal fistulas. J Urol Medicale Chir. 1953;59:150–60.
Hillary CJ, Osman NI, Hilton P, Chapple CR. The aetiology, treatment, and outcome of urogenital fistulae managed in well- and low-resourced countries: a systematic review. Eur J Urol. 2016;70:478–92.
Elkins TE. Surgery for the obstetric vesicovaginal fistula: a review of 100 operations in 82 patients. Am J Obstet Gynecol. 1994;170(4):1108–18.
Hussain A, Johnson K, Glowacki CA, Osias J, Wheeless CR Jr, Asrat K, et al. Surgical management of complex obstetric fistula in Eritrea. J Women’s Health. 2005;14(9):839–44.
Tebeu PM. Fosso GK, Vadandi V, Dobit JS, Fomulu JN, Rochat CH (2013) Prognostic value of repeated surgery on obstetric Vesicovaginal fistula outcome: a Cameroonian experience. Asian Pacific J Reprod 330–332.
United Nations Population Fund (UNFPA). Obstetric fistula: a tragic failure to deliver maternal care. New York: United Nations Population Fund; 2008. Available at: http://www.unfpa.org/mothers/fistula.htm
Cromwell D, Hilton P. Retrospective cohort study on patterns of care and outcomes of surgical treatment for lower urinary-genital tract fistula among English National Health Service hospitals between 2000 and 2009. BJU Int. 2013;111:257–62.
Waaldijk K. Surgical classification of obstetric fistulas. Int J Gynaecol Obstet. 1995;49:161–3.
Ijaiya M, Rahman GA, Aboyeji AP, Olatinwo WO, Esuga SA, Ogah K, et al. Vesicovaginal fistula: a review of Nigerian experience. West Afr J Med. 2010;29(5):293–8.
Inimgba NM, Okpani AOU, John CT. Vesico-vaginal fistulae in Port Harcourt, Nigeria. Trop J Obstet Gynaecol. 1999;16:49–51.
Odusoga OL, Oloyede OAO, Fakoya TA, Sule-Odu AO. Obstetric vesico-vaginal fistula in Sagamu. Nig Med Pract. 2001;39:73–5.
Hilton P. Urogenital fistula in the UK: a personal case series managed over 25 years. BJU Int. 2012;110:102–10.
Gerstein AD, Phillips TJ, Rogers GS, Gilchrest BA. Wound healing and aging. Dermatol Clin. 1993;11(4):749–57.
Van de Kerkhof PC, Van Bergen B, Spruijt K, Kuiper JP. Age-related changes in wound healing. Clin Exp Dermatol. 1994;19(5):369–74.
Ockrim JL, Greenwell TJ, Foley CL, Wood DN, Shah PJR. A tertiary experience of vesico-vaginal and urethro-vaginal fistula repair: factors predicting success. BJU Int. 2009;103:1122–6.
Seshan V, Alkhaswneh E, Hashmi IH. Risk factors of urinary incontinence in women: a literature review. Int J Urol Nurs. 2016;10(3):118–26.
Arrowsmith SD, Barone MA, Ruminjo J. Outcomes of obstetric fistula care: a literature review. Curr Opin Obstet Gynecol. 2013;25(5):399–403.
Hilton P. Debate: post-operative urinary fistulae should be managed by gynaecologists in specialist centres. BJU Int. 1997;80(1):35–42.
Gupta NP, Mishra S, Mishra A, Seth A, Anand A. Outcome of repeat supratrigonal obstetric vesicovaginal fistula repair after previous failed repair. Urol Int. 2012;88(2):259–62.
Acknowledgements
The authors appreciate Mrs. Marcelina who helped to retrieve the patients’ records.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Rights and permissions
About this article
Cite this article
Okunola, T.O., Yakubu, E., Daniyan, B. et al. Profile and outcome of patients with recurrent urogenital fistula in a fistula centre in Nigeria. Int Urogynecol J 30, 197–201 (2019). https://doi.org/10.1007/s00192-018-3738-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-018-3738-8