Abstract
Introduction and hypothesis
The aetiology of the overactive bladder (OAB) symptom complex is still poorly understood. In order to obtain further insight, the prevalence and predictors of the symptoms included in OAB, that is urgency, urgency incontinence (UUI), frequency and nocturia, were investigated in a sample of nonpregnant nulliparous women.
Methods
A national, postal and web-based survey of OAB symptoms was conducted in women aged 25–64 years (n = 9,197). Crude prevalence and prevalence adjusted according to body mass index (BMI) were calculated from a logistic regression model to evaluate the prevalence of OAB.
Results
The response rate was 52%. The prevalence of urgency, bothersome urgency, UUI, and nocturia, but not daytime frequency, increased consistently with advancing age and increasing BMI. Urgency was associated with BMI, age ≥45 years, nocturia, and daytime frequency of eight or more micturitions. Daytime urinary micturition frequency was not affected by age either in women with OAB or in women without OAB. Bothersome OAB affected almost half of the woman in the oldest age group and was strongly associated with nocturia of two or more micturitions and OAB with UUI.
Conclusions
There were contrasting changes in the prevalence of the different symptoms included in OAB. With increasing age and BMI, the prevalence of nocturia, urgency and UUI increased, while daytime frequency remained stable. These findings are of importance as the primary endpoint for the evaluation of drug therapies for OAB has often been daytime urinary frequency.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Overactive bladder (OAB) is defined as a symptom complex comprising urinary urgency, usually accompanied by frequency and nocturia, with or without urgency urinary incontinence (UUI), in the absence of urinary tract infection or any other obvious pathology [1]. OAB is a distressing symptom syndrome with a significant negative effect on quality of life [2,3,4]. OAB is common and epidemiological studies in Europe and North America [5,6,7,8,9] have shown an overall prevalence ranging between 12% and 20%, and in all of these studies its prevalence increased with age. Contemporary evidence suggests that the lower urinary tract symptoms in OAB are common, and among these urinary urgency is generally considered to be the cardinal symptom in patients with OAB [10]. Urgency is directly associated with the development of frequency, reduced intervoid interval and nocturia and UUI.
Because the prevalence of OAB increases with age, it could be considered that the prevalence of the individual symptoms of the OAB would also increase, but this association has not always been found in previous studies [5, 7, 8, 11]. This discrepancy may be due to specific characteristics in the populations studied. Whilst all large epidemiological studies have shown similar prevalence data, they also included women of different parities, making it difficult to control for the consequences of pregnancy and childbirth, which may have led to a confounding effect. The aim of this study was to investigate both the prevalence of OAB and the effect of ageing on urinary symptoms in a cohort of nulliparous women to exclude the possible confounding influences of pregnancy and childbirth.
Materials and methods
Ethical approval for the study was obtained from the Regional Ethical Review Board (reference no. 776-13, 18 November 2013). All women received written information and gave written consent before participation in the study.
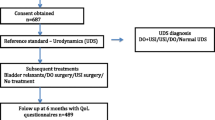
This national, postal and web-based questionnaire survey was conducted in 2014. The potential study population was identified by the Survey Division of the Central Bureau of Statistics (CBS) from the Total Population Register and comprised women registered in Sweden who had not given birth and were 25–64 years of age. A total of 625,810 nulliparous women were eligible for sampling and 20,000 were randomly selected from four independent random samples stratified by decades of age (25–34 to 55–64 years). A letter with information about the study, which included login credentials to a web-based form was sent to all the women. This introductory letter was followed by postal questionnaire. The questionnaire (web and postal versions) was returned by 10,187 women (52%) after three mailing cycles during a 4-month period. Of these women, 264 declined participation or returned a nonevaluable questionnaire. Based on the answers in the questionnaire, 194 women who were pregnant at the time and 525 parous women were excluded. Misdiagnosis of parity was predominantly related to immigration (337/525). Another 7 were excluded due to missing information about parity, leaving a total study population of 9,197.
The 40-item questionnaire included questions about current height and weight, urinary or anal incontinence, genital prolapse, childhood nocturnal enuresis, menstrual status, hysterectomy, and the menopause. The questionnaire used in this study was divided into three different sections: a symptom inventory for urinary incontinence (UI) and other lower urinary symptoms, and sections relating to faecal incontinence and genital prolapse. We also included a measure of degree of bother and distress caused by UI and other lower urinary tract symptoms, faecal incontinence and symptoms of genital prolapse. We used three separate validated questionnaires; Sandvik’s, Tegerstedt’s, and Wexner’s [12,13,14,15].
OAB was defined according to the International Continence Society (ICS)/International Urogynecological Association (IUGA) definition as urgency with or without UUI, usually accompanied by frequency and nocturia [1]. Nocturia, UI and UUI were also defined according to ICS/IUGA definitions [1]. Urgency was present in women responding in the affirmative to at least one of the following questions: “Do you have urinary urgency with a sudden and strong urge to void which is hard to postpone?”, or “Do you have involuntary loss of urine in connection with a sudden and strong urge to void?” (= UUI). In this study UUI was also termed ‘OAB wet’ and OAB without UUI was termed ‘OAB dry’. The women were requested to report the number of daytime micturitions. For the purposes of the statistical analysis, daytime micturition frequency was also dichotomized into less than eight and eight or more. The impact of urgency on daily life as perceived by the woman was dichotomized into ‘not bothersome’ (no problem/a small nuisance) or ‘bothersome‘ (some bother/much bother/a major problem). Body mass index (BMI) was calculated from weight and height reported in the questionnaire and was categorized as normal (<25 kg/m2), overweight (25.0–29.9 kg/m2), moderately obese (30.0–34.9 kg/m2), and severely and very severely obese (≥35 kg/m2). Women were also asked if they were on medication for urgency or had previously had surgery or medication for UI. The proportions of missing data in the responses to the questionnaire was low and varied between 0.3% for taking medication for UI (lowest) and 1.9% for sought consultation for UI (highest).
Characteristics of responders and nonresponders
Responders and nonresponders were compared using information from the Total Population Register, available for 99.9% of the total sample. Nonresponders were younger (56.7% of the age group 25–29 years compared with 37.3% of the age group 60–64 years), and were more likely to be immigrants (63.7%), to be non-Swedish citizens (67.8%), to be unmarried (51.2%), to live in suburban or commuting municipalities (53.7%), and to have a lower income and lower level of education (59.1% of those with ≤3 years of secondary education compared with 40.9% of those with >3 years secondary education and higher).
Statistical analysis
Statistical analyses were performed using IBM SPSS Statistics 22 software. The chi-squared and Student’s t test were used to compare characteristics of women with and without urgency. Crude and adjusted prevalences and their 95% confidence intervals (CI) were calculated for each 10-year category and calculated from the logistic regression model taking the variables age and BMI into account. Logistic regression analysis was used to identify independent predictors of having bothersome urgency. The following predictors and confounders were used: age, BMI, eight or more daytime micturitions, nocturia and OAB wet versus OAB dry. The level of statistical significance was set at p < 0.05.
Results
The overall response rate for the total cohort was 52.2%; data from 9,197 women were available for analysis. The response rate varied between 43.3% in the youngest age group (25–29 years) and increased incrementally and consistently to 62.7% in the oldest group (60–64 years). Of the respondents, 52% completed the questionnaire in web form and 48% completed the postal questionnaire. Of the respondents, 1,576 were postmenopausal, 358 had undergone a hysterectomy and 175 were taking oestrogens. Medication or treatment for urgency or UI was being taken by only a small proportion of the women (Table 1).
The symptom of urgency was reported by 1,884 of the 9,197 nulliparous women (20.5%) but was absent in 7,264 women (missing n = 49). Childhood nocturnal enuresis, hysterectomy, and surgery and medication for UI were highly over-represented among women with urgency (Table 1). Women with urgency were also older and heavier than those without (Table 1). The prevalence of urgency and urgency-related symptoms (UUI, nocturia and bothersome urgency) consistently increased across all age groups, whereas the number of daytime micturitions and prevalence of eight or more daytime micturitions were similar in the different age groups. The greatest relative increase was seen for nocturia of two or more micturitions (fourfold increase), OAB wet (threefold increase), bothersome urgency (twofold increase) and the symptom of urgency (twofold increase; Table 2).
The number of daytime micturitions and the proportion of women with eight or more daytime micturitions were also similar across all age groups in these nulliparous women with urgency. The proportion of women with ‘OAB dry’ consistently decreased, whereas the proportion of women with ‘OAB wet’ correspondingly and incrementally increased across all age groups (1.5 times). The proportion of women with nocturia of two or more micturitions increased with age more than three times from 8.5% in the youngest age group (25–34 years) to 27.2% in the oldest age group (55–64 years; Table 3).
Comparing women with urgency and those without, both groups showed increases in nocturia with age (Table 4) but the two groups showed no difference in daytime frequency (Table 4). In the logistic regression analysis, urgency showed significant associations with BMI, age ≥45 years, nocturia, daytime frequency of eight or more micturitions, and childhood enuresis (Table 5). In the logistic regression analysis, bothersome urgency showed the strongest associations with nocturia of two or more micturitions (OR 2.80, 95% CI 2.15–3.67), ‘OAB wet’ (OR 2.39, 95% CI 1.95–2.94), and eight or more daytime micturitions (OR 1.30, 95% CI 1.05–1.59; Table 6). Age and BMI were not significant predictors. Women with urgency were twice as likely to have eight or more daytime micturitions and nocturia of one or more micturitions than women without urgency, and three times as likely to have nocturia of two or more micturitions (Table 4).
Discussion
The main findings of this study were that the prevalence of OAB/urgency, bothersome urgency, UUI, and nocturia increased with increasing age. Across all ages, nocturia of two or more micturitions was consistently about three times more prevalent in women with OAB than in those without. In contrast, in both women with and women without OAB, daytime frequency was not associated with age. The presence of urgency was associated with increasing BMI and age, nocturia, and a daytime frequency of eight or more micturitions. Bothersome OAB affected almost half the woman in the oldest age group and was strongly associated with nocturia of two or more micturitions and OAB wet.
OAB is common in women of childbearing age [5,6,7,8,9, 11]. Since most previous cross-sectional studies have included women of different parities, the effects of pregnancy and childbirth may have influenced the reported prevalence. The present study addressed this problem by studying nonpregnant, nulliparous women of different ages. To our knowledge the only study that has previously evaluated the prevalence of urgency in nulliparous women of different ages (2,251 of 18,992 women) is the national cross-sectional survey of Chinese women by Zhang et al. [11]. They showed that urgency (according to the ICS/IUGA definition) increased linearly from 11.8% in women aged 20–29 years to 32.3% in women aged 60–69 years, which is consistent with our results. In the same study daytime frequency (defined as eight or more micturitions per day) increased from 13.0% to 22.4% in the same age groups, which is in contrast to our findings.
The current definition of OAB is urgency with or without UUI usually with frequency and nocturia [1]. This study demonstrated that age and BMI influence the symptoms of OAB differently. The aetiology of OAB is still unknown, but it is likely to be multifactorial. Our results suggest a time-dependent change in prevalence contrasting daytime frequency, and nocturia and urgency. These data are consistent with the hypothesis that urgency is the driving symptom for daytime frequency, nocturia and UUI, although daytime frequency is unlikely to be influenced by urgency alone.
The pattern of changes in the prevalence of daytime frequency found in this study and in a previous study of predominantly parous women [5] is of importance, as daytime frequency has been both a trial entry criterion and a primary endpoint in studies evaluating OAB drug therapy. It is apparent from this cohort of nulliparous women, that daytime frequency does not follow the same pattern of change as seen for urgency and nocturia. The prevalence of urgency increases with age, although data on frequency are not consistent [5,6,7,8,9, 11]. In more elderly women, frequency may be affected by behavioural changes, such as reduced fluid intake in older individuals, redistribution of body water, a reduction in nocturnal renal concentrating ability or central redistribution of peripherally pooled interstitial fluid when supine, resulting in an increased incidence of nocturia. In the absence of other factors such as urgency, one could hypothesize that life-time 24-h voiding frequency remains the same although the ratio between daytime and night time voiding changes with ageing resulting in a reduction in daytime frequency and an increase in nocturia.
This study supports previous epidemiological work demonstrating an increase in nocturia with increasing age [16, 17]. This is likely to result from an increase in urgency with age as well as other age-related changes such as nocturnal polyuria relating to diabetes mellitus, cardiac disease, sleep apnoea and sleep disturbance, an increase in BMI and potentially other factors such as an increase in bladder overactivity. Nocturia of two or more micturitions has been shown to be bothersome in terms of both effect on quality of life [16] and increased morbidity and mortality. The prevalence of nocturia in women aged 55–64 years with urgency was 73–74% compared to 50% in women without urgency, an increase of 24% in those with OAB. A similar pattern was seen for nocturia of two or more micturitions.
The main strengths of this study were the large, randomly selected, national cohort of nonpregnant, nulliparous women covering an age span of 40 years. The women included were aged 25–64 years and older women were deliberately excluded in order to restrict the confounding effects of multiple illnesses. We also wanted to include a larger number of fertile women for the planned prospective longitudinal follow-up of these nulliparous women. Subjects were identified and recruited from the Total Population Register. All births are continuously recorded, and the register is updated every 6 weeks. A control question regarding ongoing pregnancy and previous births was also included in the questionnaire. A cohort restricted to nulliparous women is optimal for studying the natural history of pelvic floor dysfunction, without the interference of pregnancy and birth-related confounding factors. OAB symptoms (micturition frequency, urgency, nocturia and UUI) were self-reported using validated questions and reported according to current ICS/IUGA definitions [1]. The data presented were based on a subjective evaluation by the women themselves and were not confirmed objectively. However, the use of a questionnaire is considered to be the most feasible tool for gathering information about these sensitive issues [18].
Some limitations of this study need to be considered. First, the response rate increased consistently with age from 43% among the youngest to 63% in the oldest age group. A possible explanation for this difference in response rates is that older women are more compliant with questionnaires and are also more motivated to respond. Symptoms are more commonly encountered in older women and they may have more time to do so. This may have tended to overestimate overall prevalence figures. Second, the validity of the self-reported information depends on the participants’ willingness and ability to perceive, evaluate and report correctly. Third, data about nonresponders suggest a selection bias. Nonresponders were younger, more often immigrants or non-Swedish citizens, less often married and living in suburbs or commuting municipalities, had a lower income and a lower level of education compared with responders. A lower socioeconomic status (SES) among nonresponders is known to be associated with many other predictors of UI whereas higher SES has been consistently linked to increased help-seeking behaviour [19]. In addition, the women in this study were predominantly Caucasian, and the results should be interpreted with caution in relation to diverse ethnic groups.
Conclusions
This study demonstrated an increase in the prevalence of urgency and hence OAB as well as nocturia with increasing age in nulliparous women between the ages of 25 and 64 years. However, there was no corresponding age-related effect on daytime frequency. This is surprising since women with OAB have a higher prevalence of daytime frequency (eight or more micturitions per day) across ages than women without urgency.
References
Haylen BT, de Ridder D, Freeman RM, Swift SE, Berghmans B, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Int Urogynecol J. 2010;21:5–26. doi:10.1007/s00192-009-0976-9.
Kelleher CJ, Cardozo LD, Khullar V, Salvatore S. A new questionnaire to assess the quality of life of urinary incontinent women. Br J Obstet Gynaecol. 1997;104:1374–9.
Coyne KS, Sexton CC, Irwin DE, Kopp ZS, Kelleher CJ, Milsom I. The impact of overactive bladder, incontinence and other lower urinary tract symptoms on quality of life, work productivity, sexuality and emotional wellbeing in men and women: results from the EPIC study. BJU Int. 2008;101:1388–95.
Vaughan CP, Johnson TM 2nd, Ala-Lipasti MA, et al. The prevalence of clinically meaningful overactive bladder: bother and quality of life results from the population-based FINNO study. Eur Urol. 2011;59:629–36.
Milsom I, Abrams P, Cardozo L, Roberts RG, Thüroff J, Wein AJ. How widespread are the symptoms of an overactive bladder and how are they managed? A population-based prevalence study. BJU Int. 2001;87:760–6.
Stewart WF, Van Rooyen JB, Cundiff GW, et al. Prevalence and burden of overactive bladder in the United States. World J Urol. 2003;20:327–36.
Irwin DE, Milsom I, Hunskaar S, et al. Population-based survey of urinary incontinence, overactive bladder, and other lower urinary tract symptoms in five countries: results of the EPIC study. Eur Urol. 2006;50:1306–14.
Coyne KS, Sexton CC, Thompson CL, et al. The prevalence of lower urinary tract symptoms (LUTS) in the USA, the UK and Sweden: results from the epidemiology of LUTS (EpiLUTS) study. BJU Int. 2009;104:352–60.
Milsom I, Coyne KS, Nicholson S, Kvasz M, Chen CI, Wein AJ. Global prevalence and economic burden of urgency urinary incontinence: a systematic review. Eur Urol. 2014;65:79–95.
Abrams P. Urgency: the key to defining overactive bladder. BJU Int. 2005;96(Suppl 1):1–3.
Zhang L, Zhu L, Xu T, et al. A population-based survey of the prevalence, potential risk factors, and symptom-specific bother of lower urinary tract symptoms in adult Chinese women. Eur Urol. 2015;68:97–112.
Sandvik H, Hunskaar S, Seim A, Hermstad R, Vanvik A, Bratt H. Validation of a severity index in female urinary incontinence and its implementation in an epidemiological survey. J Epidemiol Community Health. 1993;47:497–9.
Hannestad YS, Rortveit G, Sandvik H, Hunskaar S. A community-based epidemiological survey of female urinary incontinence: the Norwegian EPINCONT study. Epidemiology of Incontinence in the County of Nord-Trondelag. J Clin Epidemiol. 2000;53:1150–7.
Tegerstedt G, Miedel A, Maehle-Schmidt M, Nyren O, Hammarstrom M. A short-form questionnaire identified genital organ prolapse. J Clin Epidemiol. 2005;58:41–6.
Jorge JM, Wexner SD. Etiology and management of fecal incontinence. Dis Colon Rectum. 1993;36:77–97.
Tikkinen KA, Johnson TM 2nd, Tammela TL, et al. Nocturia frequency, bother, and quality of life: how often is too often? A population-based study in Finland. Eur Urol. 2010;57:488–96.
Madhu C, Coyne K, Hashim H, Chapple C, Milsom I, Kopp Z. Nocturia: risk factors and associated comorbidities; findings from the EpiLUTS study. Int J Clin Pract. 2015;69:1508–16.
Rothman KJ, Greenland S, Lash TL. Design strategies to improve study accuracy, restriction. In: Modern epidemiology. 3rd ed. Philadelphia: Lippincott Williams & Wilkins; 2008. p. 168–82.
Milsom I, Altman D, Cartwright R, et al (2013) Epidemiology of urinary incontinence (UI) and other lower urinary tract symptoms (LUTS), pelvic organ prolapse (POP) and anal (AI) incontinence. In: Abrams P, Cardozo L, Khoury H, Wein A, editors. Incontinence. Health Publications Ltd, Paris.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
D.R. has received honoraria from Astellas, Allergan, Ixaltis, Ferring and Pfizer for consultancy, speaker and/or trial participation. S.Å. has no competing interests. A.W. has received honoraria from Astellas Pharma, Pfizer Corp and SCA. C.C. has received honoraria from Allergan, Astellas, Medtronic, Ono and Recordati for consultancy, speaker and/or trial participation. I.M. has received honoraria from Allergan, Astellas, Pfizer and SCA for consultancy, speaker and trial participation. M.G. has received honoraria from Astellas for speaker participation.
Funding
The study was supported by a National LUA/ALF grant no. 11,315, grants from The Göteborg Medical Society and Hjalmar Svenssons Fund, Alice Swenzons Fund and The Healthcare Committee, Region Västra Götaland. The funding sources had no role in study design, data analysis, data interpretation, or writing of the report.
Rights and permissions
About this article
Cite this article
Robinson, D., Åkervall, S., Wagg, A. et al. Prevalence and predictors of overactive bladder in nonpregnant nulliparous women below 65 years of age. Int Urogynecol J 29, 531–537 (2018). https://doi.org/10.1007/s00192-017-3435-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-017-3435-z