Abstract
Introduction and hypothesis
The aim of this study was to compare robotic or laparoscopic sacrohysteropexy (RLSH) and open sacrohysteropexy (OSH) as a surgical treatment for pelvic organ prolapse (POP).
Methods
Among 111 consecutive patients who had undergone sacrohysteropexy for POP, surgical outcomes and postoperative symptoms were compared between the RLSH (n = 54; robotic 14 cases and laparoscopic 40 cases) and OSH (n = 57). groups The medical records of enrolled patients were reviewed retrospectively.
Results
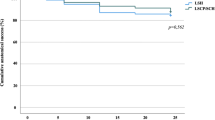
Compared with the OSH group, the RLSH group had shorter operating time (120.2 vs 187.5 min, p < 0.0001), less operative bleeding (median estimated blood loss 50 vs 150 ml; p < 0.0001; mean hemoglobin drop 1.4 vs 2.0 g/dl; p < 0.0001), and fewer postoperative symptoms (13 vs 45.6 %; p < 0.0001). Patients’ overall satisfaction (94.4 vs 91.2 %; p = 0.717) and required reoperation due to postoperative complications (3.7 vs 1.8 %; p = 0.611) did not differ between groups.
Conclusions
RLSH could be a feasible and safe procedure in patients with POP and should be considered as a surgical option that allows preservation of the uterus. Prospective randomized trials will permit the evaluation of potential benefits of RLSH as a minimally invasive surgical approach.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Introduction
Pelvic organ prolapse (POP) is a common problem in parous women. About 40 % of all women develop POP in their lifetime [1]. Its incidence increases with age, and its etiology is believed to arise from a combination of genetic and environmental risk factors [2–4]. As life expectancy and patients’ complaints increase, a significantly greater number of women need to undergo surgery [5]. The types of repair vary depending on the type of prolapse and associated symptoms. Of these, abdominal approaches using mesh have been regarded as a gold standard. Abdominal sacrocolpopexy is durable and effective for correcting apical prolapse [6]; however, it remains unknown whether concomitant hysterectomy at the time of POP surgery is essential, and few randomized trials of hysterectomy versus no hysterectomy have been performed [7]. Moreover, two independent studies showed many women with POP preferred to retain their uterus at the time of surgery in the absence of a substantial benefit from hysterectomy [8, 9]. In a recent review article, Ridgeway described that uterine preservation at the time of POP surgery had several advantages, including reduced surgical time and blood loss, maintenance of fertility, avoidance of an unnecessary procedure, perceived role of the uterus and cervix in pelvic stability and sexual satisfaction, less invasiveness, quicker recovery, and decreased risk of mesh exposure [7]. Several studies showed that sacrohysteropexy was as effective as sacrocolpopexy following hysterectomy in anatomical outcomes and supported the expected advantages of sacrohysteropexy [10–14]. In addition, sacrohysteropexy is associated with less mesh exposure because it avoids placing a foreign body near the colpotomy site [15]. Although sacrocolpopexy following subtotal hysterectomy (sacrocervicopexy) may be an option to overcome problems that might follow performing hysterectomy prior to sacrocolpopexy, it can induce a longer operating time and more perioperative blood loss compared with sacrohysteropexy [16–18].
Compared with laparotomy, which can induce complications such as hemorrhage, bowel obstruction, and wound infection [19, 20], minimally invasive surgery can be performed to meet female patients’ demands for less surgical scarring and fewer possible complications. Technology and techniques related to robotic or laparoscopic surgery are still evolving in the direction of easier, minimally invasive, surgery [21–23]. Laparoscopic surgery combines the benefits of the abdominal procedure with those of transvaginal surgery. Additionally, because robotic surgery has greatly improved surgeon dexterity, surgical precision, visualization, and ergonomics and allowed procedures that were performed by laparotomy to be performed by laparoscopy [24], we expected the robotic approach might allow surgeons to more easily perform surgical procedures of sacrohysteropexy. The purpose of this study was to compare robotic or laparoscopic sacrohysteropexy (RLSH) and open sacrohysteropexy (OSH) as surgical treatment for POP.
Materials and methods
Patients
Written informed consent was obtained from all patients prior to surgery. Between January 2006 and June 2014, we identified 111 consecutive patients who underwent RLSH or OSH for POP with symptomatic stage ≥2. The degree of prolapse was evaluated using an international unified classification of POP. All patients who wanted minimally invasive surgery underwent RLSH instead of OSH. We analyzed all patients enrolled during this period and reviewed their medical records retrospectively. The enrolled patients were divided into two groups based on surgical approach: the RLSH group (n = 54) and the OSH group (n = 57). The RLSH group comprised 14 robotic and 40 laparoscopic surgeries; the 14 robotic surgeries were performed by a single surgeon (JP), with experience in >250 cases of robotic surgery and 900 of laparoscopic surgery for gynecologic disease. In addition, 40 laparoscopic and 57 open surgeries were performed by two surgeons (YK and ML), who were experienced laparoscopic gynecologic surgeons. This study was exempt from Institutional Review Board approval due to its retrospective nature. Patient status was estimated in terms of POP Quantification (POP-Q) the presence of peritoneal adhesion, operating time, estimated blood loss, serum hemoglobin (Hb) drop (change between preoperative Hb and Hb 1 day after surgery), and operative complications. Peritoneal adhesion was defined as a condition in which pathological bonds had formed between the omentum, the small and large bowels, the abdominal wall, and other intra-abdominal organs. Operating time was defined as time from first incision to closure. All patients filled in a questionnaire created by our institution regarding subjective evaluation of related symptoms before and 12 months after surgery. Patients reported overall satisfaction with surgery and discomfort from accompanying symptoms, including abdominal pain, voiding dysfunction, urinary incontinence, overactive bladder, constipation, and dyspareunia. Urinary incontinence and overactive bladder were diagnosed on the basis of urodynamic studies by urologists. Objective failure was defined as POP-Q stage >2 at 12 months after surgery. Patients who needed additional surgery within 12 months were regarded as both subjective and objective failures.
Surgical techniques
For the robotic approach, the da Vinci Si Surgical System (Intuitive Surgical, Inc., CA, USA) was used. After a vertical skin incision was made in the umbilicus, the abdominal cavity was entered using the open technique. We used three robotic arms and one camera port. The instruments and accessories included a ProGrasp grasper, monopolar scissors, fenestrated bipolar cautery, and mega SutureCut needle driver. For the laparoscopic approach, three laparoscopic ports were placed after pneumoperitoneum was created. A 30° laparoscope was used for RLSH. The RLSH procedure was equal to that of OSH. A RUMI uterine manipulator was placed with a KOH colpotomizer system (Cooper Surgical, CT, USA) in the RLSH group. Because the uterine manipulator allowed an assistant to push up the vaginal wall and the posterior fornix, surgeons could achieve the vesicovaginal and the rectovaginal plane without difficulty. The peritoneum was incised from the sacral promontory, and dissection was performed until the anterior longitudinal ligament was identified (Fig. 1a). After the right ureter was identified, a peritoneal tunnel from the sacral promontory to the uterosacral ligament was created (Fig. 1b). The bladder was mobilized from the cervix to expose 3 cm of the underlying pubocervical fascia. The windows were made in the bilateral broad ligament at the level of the cervicouterine junction lateral to the uterine artery. The rectovaginal space was entered at the level of the uterosacral ligaments and developed using blunt dissection to expose the rectovaginal fascia. Consequently, tunnels were created bilaterally from the windows to the uterosacral ligament (Fig. 1c). A self-styled nonabsorbable polypropylene monofilament Gynemesh (Ethicon Endo-surgery, OH, USA) was used. The left and right arms of the mesh were passed through the bilateral tunnels created around the uterus, attached to the cervix, and passed through the peritoneal tunnel to the sacral promontory. Both ends of the mesh were fixed to the anterior vagina (Fig. 1d) and the sacral promontory (Fig. 1e) with two nonabsorbable 1-0 polydioxanone sutures (Ethicon Endo-surgery). The peritoneum was approximated with 2-0 Vicryl sutures in order to cover the mesh (Fig. 1f).
Procedures of robotic sacrohysteropexy: a identification of anterior longitudinal ligament, b peritoneal tunnel from sacral promontory to the uterosacral ligament, c opening of anterior broad ligament and tunnel from anterior broad ligament to the uterosacral ligament, d, e fixation of both ends of mesh on the anterior vagina and sacral promontory, f approximation of peritoneum to cover the mesh
Statistical analysis
All continuous data are expressed as mean ± standard deviation (SD), and categorical data are reported as absolute number or percentage. Frequency distributions were compared using the chi-square and Fisher’s exact tests, and mean or median values were compared using Student’s t and Mann–Whitney U tests. All p values were two sided, and p < 0.05 was considered statistically significant. Data were analyzed using SAS/STAT software, version 9.4 (SAS Institute Inc., NC, USA).
Results
A summary of patient characteristics is presented in Table 1. Although the RLSH group had a history of fewer previous pelvic surgeries compared with the OSH group (25.9 vs 73.7 %; p < 0.0001), there was no difference in presence of peritoneal adhesions between groups (p = 0.690). Median POP-Q stage before surgery was three in both groups (p = 0.378). Table 2 shows comparison data in terms of surgical outcomes. Compared with the OSH group, the RLSH group had shorter operating time (120.2 vs 187.5 min; p < 0.0001), less operative bleeding (median 50 vs 150 ml; p < 0.0001, mean Hb drop 1.4 vs 2.0 g/dl; p < 0.0001), and fewer postoperative symptoms (13 vs 45.6 %; p < 0.0001). According to the clinical protocol urinary Foley catheters were removed on the morning 3 days after surgery, and patients were discharged from hospital on the same day without complication in either group. For some patients who complained of abdominal discomfort or wanted to delay discharge, we removed urinary catheters when they were discharged from hospital. Median follow-up was 30 (range 12–108) months. Patients’ overall satisfaction (94.4 vs 91.2 %; p = 0.717) and required reoperation due to postoperative symptoms (3.7 vs 1.8 %; p = 0.611) did not differ between groups. Of patients in the RLSH group, two underwent laparoscopic hysterectomy followed by sacrocolpopexy because they complained of voiding dysfunction, which was related to bulging of the vagina 6 months after initial surgery. Of the OSH group, one patient needed fixed mesh removal due to persistent abdominal pain 5 months after surgery. The three patients who needed additional surgery within 12 months were regarded as both subjective and objective failures. Therefore, the objective success rate was 96.3 % and 98.2 % (RLSH vs OSH; p = 0.611), In relation to the number of patients who experienced relevant symptoms at least once during the follow-up period, the RLSH group was smaller than the OSH group (13 vs 45.6 %; p < 0.0001) (Table 3).
Discussion
Several advantages of uterine preservation in pelvic reconstructive surgery have been described in the literature. These include maintaining pelvic anatomy, decreased operating time, less intraoperative blood loss, and faster recovery time. Increasingly, patients prefer preservation of the uterus; it appears to contribute positively to self-esteem, confidence, and sexuality [25]. In conventional laparoscopy with uterine preservation, success rates of 97.4 % are reported, but classic laparoscopy is mainly used in vaginal-vault prolapse [25]. Another prospective study in which laparoscopic sacrohysteropexy was performed in 51 women showed no objective recurrence of uterine prolapse during a 10-week follow-up [26]; however, comparison of efficacy between sacrohysteropexy and vaginal techniques that preserve the uterus may be necessary. We found no well-designed study on that topic and must await results of a multicenter randomized controlled noninferiority trial of a Dutch group that compares laparoscopic sacrohysteropexy with vaginal sacrospinous hysteropexy [27]. Additionally, following their multicenter randomized non-inferiority trial, Detollenaere and colleagues showed uterus preservation by sacrospinous hysteropexy was not inferior to vaginal hysterectomy with suspension of the uterosacral ligaments in relation to surgical failure of the apical compartment at 12 months’ follow-up [28]. Nevertheless, there are few studies reporting on feasibility or outcomes of laparoscopic sacrohysteropexy. Because it is not so easy to the laparoscopic procedures for sacrohysteropexy are performed popularly. In particular, inserting laparoscopic sutures using standard laparoscopic needle drivers is technically challenging. Seror et al. showed robotic sacrohysteropexy to be potentially superior to classic laparoscopy in terms of operative time and blood loss. Furthermore, better long-term outcomes are expected due to improved suturing and dissection techniques [29]. Also, its minimally invasive character leads to better hemostasis, shorter hospital stay, reduced morbidity, and less postoperative pain as opposed to the open procedure [30, 31].
In this study, we compared a robotic or laparoscopic approach to an open method, regarding the former as being minimally invasive. The reasons we considered robotic and laparoscopic surgery patients as one group is that. first, we felt there would be no significant difference in surgical outcomes and objective failure rates between robotic and laparoscopic sacrohysteropexy. Second, we expected that the characteristics of the robotic system, including wristed instruments and good visualization, would help surgeons perform intracorporeal suturing and allow mesh placement on correct sites. In addition, the number of robotic sacrohysteropexies was too small to be compared with other approaches.
The RLSH group had fewer previous pelvic surgeries compared with the OSH group (25.9 vs 73.7 %), and there was no difference of in presence of peritoneal adhesions between groups (p = 0.690). However, the difference in previous pelvic surgery history was accidental and not a selection bias. In addition, the factor related to surgical outcomes—including operating time and perioperative complications—was not prior abdominal surgery but the presence of adhesion. Therefore, we made the determination that there was no statistically significant difference in patient characteristics between groups. As a result, the RLSH group showed shorter operating time, less operative bleeding, and less postoperative symptoms compared with the OSH group. To suture and tie intracorporeally is more challenging than in any other surgical procedure for RLSH, and as this was a retrospective study, we were unable to determine a proficiency and learning curve with regard to suturing and tieing. However, we performed the procedure without technical difficulty or considerable increase in time because we already had much experiences with robotic and laparoscopic surgery. Moreover, advantages of the robotic system allowed ease of operation. Any difference in operating time between groups was due to the time required for wound opening and closure. Although RLSH showed a shorter operating time, it was not clinically significant. In addition, the robotic group required a longer operating time than the laparoscopic or open approach (Table 2). However, robotic surgery generally requires additional time besides actual operating time during other gynecologic surgeries and sacrohysteropexy. Regardless, studies show that robotic surgery is not inferior to laparoscopic or open surgery in terms of surgical outcomes, including postoperative pain [32, 33]. We removed urinary catheters 3 days after surgery in both groups according to our clinical protocol. Except for case reports, very few studies indicate when urinary catheters were removed: Pan et al. removed urinary catheters a mean of 2.3 days after surgery in 65 patients who underwent laparoscopic sacrohysteropexy [34]. Mesh or suture complications have been reported in 4.2 % of cases using polypropylene mesh in abdominal correction of POP [35].
Although mesh erosion was seen in the RLSH group but there were three patients in the OSH group, there was no statistically significant difference (p = 0.244).;clinical significance could not be determined because of the small number of patients. Overall patient satisfaction or required reoperation due to postoperative complications did not differ between groups, and the RLSH group had favorable outcomes compared with the OSH group. Because this was a retrospective study, we could not completely avoid selection bias. Additionally, for the reason mentioned above, we could not determine the POP-Q value of all pelvic floor compartments before and after surgery. Regarding costs related to robotic surgery, the controversy is likely to continue; several studies showed the increased costs were unacceptable from an economic perspective [36], and some studies report that the longer operating time required for robotic surgery causes the increased costs [37]. However, it is expected that competition between robotic system manufacturing companies and improving surgeon skills will decrease costs in the near future.
In conclusion, RLSH could be a feasible and safe procedure in patients with POP and should be considered a surgical option that allows uterus preservation. Prospective randomized trials will permit the evaluation of the potential benefits of RLSH as a minimally invasive surgical approach.
References
Olsen AL, Smith VJ, Bergstrom JO, Colling JC, Clark AL (1997) Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence. Obstet Gynecol 89:501–506. doi:10.1016/s0029-7844(97)00058-6
Jelovsek JE, Maher C, Barber MD (2007) Pelvic organ prolapse. Lancet 369:1027–1038. doi:10.1016/s0140-6736(07)60462-0
Dietz HP (2008) The aetiology of prolapse. Int Urogynecol J Pelvic Floor Dysfunct 19:1323–1329. doi:10.1007/s00192-008-0695-7
Mothes AR, Radosa MP, Altendorf-Hofmann A, Runnebaum IB (2015) Risk index for pelvic organ prolapse based on established individual risk factors. Arch Gynecol Obstet. doi:10.1007/s00404-015-3863-2
Thys SD, Roovers JP, Geomini PM, Bongers MY (2012) Do patients prefer a pessary or surgery as primary treatment for pelvic organ prolapse. Gynecol Obstet Investig 74:6–12. doi:10.1159/000336634
Nygaard IE, McCreery R, Brubaker L, Connolly A, Cundiff G, Weber AM, Zyczynski H, Network PFD (2004) Abdominal sacral colpopexy: a comprehensive review. Obstet Gynecol 104:805–823
Ridgeway BM (2015) Does prolapse equal hysterectomy? The role of uterine conservation in women with uterovaginal prolapse. Am J Obstet Gynecol. doi:10.1016/j.ajog.2015.07.035
Korbly NB, Kassis NC, Good MM, Richardson ML, Book NM, Yip S, Saguan D, Gross C, Evans J, Lopes VV, Harvie HS, Sung VW (2013) Patient preferences for uterine preservation and hysterectomy in women with pelvic organ prolapse. Am J Obstet Gynecol 209:470–e1-6. doi:10.1016/j.ajog.2013.08.003
Frick AC, Barber MD, Paraiso MF, Ridgeway B, Jelovsek JE, Walters MD (2013) Attitudes toward hysterectomy in women undergoing evaluation for uterovaginal prolapse. Female Pelvic Med Reconstr Surg 19:103–109. doi:10.1097/SPV.0b013e31827d8667
Barranger E, Fritel X, Pigne A (2003) Abdominal sacrohysteropexy in young women with uterovaginal prolapse: long-term follow-up. Am J Obstet Gynecol 189:1245–1250. doi:10.1067/S0002-9378(03)00665-3
Leron E, Stanton SL (2001) Sacrohysteropexy with synthetic mesh for the management of uterovaginal prolapse. BJOG 108:629–633. doi:10.1111/j.1471-0528.2001.00138.x
Moiety FM, Hegab HM, Ghanem IA, Zedan WM, Salem HA (2010) Abdominal sacrohysteropexy for uterovaginal prolapse: a prospective study on 33 cases. Arch Gynecol Obstet 281:631–636. doi:10.1007/s00404-009-1146-5
Jeon MJ, Jung HJ, Choi HJ, Kim SK, Bai SW (2008) Is hysterectomy or the use of graft necessary for the reconstructive surgery for uterine prolapse? Int Urogynecol J Pelvic Floor Dysfunct 19(3):351–355
Costantini E, Porena M, Lazzeri M, Mearini L, Bini V, Zucchi A (2013) Changes in female sexual function after pelvic organ prolapse repair: role of hysterectomy. Int Urogynecol J 24:1481–1487. doi:10.1007/s00192-012-2041-3
Gutman R, Maher C (2013) Uterine-preserving POP surgery. Int Urogynecol J 24:1803–1813. doi:10.1007/s00192-013-2171-2
Rosati M, Bramante S, Bracale U, Pignata G, Azioni G (2013) Efficacy of laparoscopic sacrocervicopexy for apical support of pelvic organ prolapse. JSLS 17:235–244. doi:10.4293/108680813X13654754535115
Rosati M, Bramante S, Conti F (2014) A review on the role of laparoscopic sacrocervicopexy. Curr Opin Obstet Gynecol 26:281–289. doi:10.1097/GCO.0000000000000079
Li S, Ji M, Zhao Z (2015) The effectiveness of two different laparoscopic surgeries for apical support of pelvic organ prolapse. Eur J Obstet Gynecol Reprod Biol 188:74–78. doi:10.1016/j.ejogrb.2015.03.007
Demirci F, Ozdemir I, Somunkiran A, Topuz S, Iyibozkurt C, Duras Doyran G, Kemik Gul O, Gul B (2007) Perioperative complications in abdominal sacrocolpopexy and vaginal sacrospinous ligament fixation procedures. Int Urogynecol J Pelvic Floor Dysfunct 18:257–261. doi:10.1007/s00192-006-0134-6
Richter HE, Goode PS, Kenton K, Brown MB, Burgio KL, Kreder K, Moalli P, Wright EJ, Weber AM (2007) The effect of age on short-term outcomes after abdominal surgery for pelvic organ prolapse. J Am Geriatr Soc 55:857–863. doi:10.1111/j.1532-5415.2007.01178.x
Germain A, Thibault F, Galifet M, Scherrer ML, Ayav A, Hubert J, Brunaud L, Bresler L (2013) Long-term outcomes after totally robotic sacrocolpopexy for treatment of pelvic organ prolapse. Surg Endosc 27:525–529. doi:10.1007/s00464-012-2472-4
Yoo HN, Kim TJ, Lee YY, Choi CH, Lee JW, Bae DS, Kim BG (2015) Single-site robotic surgery in gynecologic cancer: a pilot study. J Gynecol Oncol 26:62–67. doi:10.3802/jgo.2015.26.1.62
Buchs NC, Pugin F, Ris F, Volonte F, Morel P, Roche B (2013) Early experience with robotic rectopexy. Int J Med Robot 9:e61–e65. doi:10.1002/rcs.1498
Barbash GI, Glied SA (2010) New technology and health care costs--the case of robot-assisted surgery. N Engl J Med 363:701–704. doi:10.1056/NEJMp1006602
Zucchi A, Lazzeri M, Porena M, Mearini L, Costantini E (2010) Uterus preservation in pelvic organ prolapse surgery. Nat Rev Urol 7:626–633. doi:10.1038/nrurol.2010.164
Price N, Slack A, Jackson SR (2010) Laparoscopic hysteropexy: the initial results of a uterine suspension procedure for uterovaginal prolapse. BJOG 117:62–68. doi:10.1111/j.1471-0528.2009.02396.x
van IJsselmuiden MN, Coolen AL, Detollenaere RJ, den Boon J, Bongers M, van de Pol G, Vollebregt A, Radder CM, Deprest J, van Eijndhoven HW (2014) Hysteropexy in the treatment of uterine prolapse stage 2 or higher: a multicenter randomized controlled non-inferiority trial comparing laparoscopic sacrohysteropexy with vaginal sacrospinous hysteropexy (LAVA-trial, study protocol). BMC Womens Health 14:112. doi:10.1186/1472-6874-14-112
Detollenaere RJ, den Boon J, Stekelenburg J, IntHout J, Vierhout ME, Kluivers KB, van Eijndhoven HW (2015) Sacrospinous hysteropexy versus vaginal hysterectomy with suspension of the uterosacral ligaments in women with uterine prolapse stage 2 or higher: multicentre randomised non-inferiority trial. BMJ 351:h3717. doi:10.1136/bmj.h3717
Seror J, Yates DR, Seringe E, Vaessen C, Bitker MO, Chartier-Kastler E, Roupret M (2012) Prospective comparison of short-term functional outcomes obtained after pure laparoscopic and robot-assisted laparoscopic sacrocolpopexy. World J Urol 30:393–398. doi:10.1007/s00345-011-0748-2
Geller EJ, Siddiqui NY, Wu JM, Visco AG (2008) Short-term outcomes of robotic sacrocolpopexy compared with abdominal sacrocolpopexy. Obstet Gynecol 112:1201–1206. doi:10.1097/AOG.0b013e31818ce394
Vitobello D, Siesto G, Bulletti C (2012) Robotic sacral hysteropexy for pelvic organ prolapse. Int J Med Robot 8:114–117. doi:10.1002/rcs.447
Wright JD, Ananth CV, Lewin SN, Burke WM, Lu YS, Neugut AI, Herzog TJ, Hershman DL (2013) Robotically assisted vs laparoscopic hysterectomy among women with benign gynecologic disease. JAMA 309:689–698. doi:10.1001/jama.2013.186
Serati M, Bogani G, Sorice P, Braga A, Torella M, Salvatore S, Uccella S, Cromi A, Ghezzi F (2014) Robot-assisted sacrocolpopexy for pelvic organ prolapse: a systematic review and meta-analysis of comparative studies. Eur Urol 66:303–318. doi:10.1016/j.eururo.2014.02.053
Pan K, Cao L, Ryan NA, Wang Y, Xu H (2015) Laparoscopic sacral hysteropexy versus laparoscopic sacrocolpopexy with hysterectomy for pelvic organ prolapse. Int Urogynecol J. doi:10.1007/s00192-015-2775-9
Siddiqui NY, Grimes CL, Casiano ER, Abed HT, Jeppson PC, Olivera CK, Sanses TV, Steinberg AC, South MM, Balk EM, Sung VW, Society of Gynecologic Surgeons Systematic Review Group (2015) Mesh sacrocolpopexy compared with native tissue vaginal repair: a systematic review and meta-analysis. Obstet Gynecol 125:44–55. doi:10.1097/AOG.0000000000000570
Desille-Gbaguidi H, Hebert T, Paternotte-Villemagne J, Gaborit C, Rush E, Body G (2013) Overall care cost comparison between robotic and laparoscopic surgery for endometrial and cervical cancer. Eur J Obstet Gynecol Reprod Biol 171:348–352. doi:10.1016/j.ejogrb.2013.09.025
Fader AN, Seamon LG, Escobar PF, Frasure HE, Havrilesky LA, Zanotti KM, Secord AA, Boggess JF, Cohn DE, Fowler JM, Skafianos G, Rossi E, Gehrig PA (2012) Minimally invasive surgery versus laparotomy in women with high grade endometrial cancer: a multi-site study performed at high volume cancer centers. Gynecol Oncol 126:180–185. doi:10.1016/j.ygyno.2012.04.028
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Additional information
Jiheum Paek and Maria Lee contributed equally to this work.
Rights and permissions
About this article
Cite this article
Paek, J., Lee, M., Kim, B.W. et al. Robotic or laparoscopic sacrohysteropexy versus open sacrohysteropexy for uterus preservation in pelvic organ prolapse. Int Urogynecol J 27, 593–599 (2016). https://doi.org/10.1007/s00192-015-2869-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-015-2869-4