Abstract
Introduction and hypothesis
The discovery of tension-free vaginal tape (TVT) began in 1986 with two unrelated observations: pressure applied unilaterally at the midurethra controlled urine loss on coughing; implanted Teflon tape caused a collagenous tissue reaction.
Methods and results
In 1987, Mersilene tape was implanted retropubically in 13 large dogs, with the aim of creating an artificial collagenous pubourethral neoligament. Extensive testing showed that the operation was safe and effective. In 1988–1989, human testing was carried out (n = 30). Mersilene tape cured 100 % of stress and mixed incontinence with a sling in situ; however, there was simultaneous recurrence of the two symptoms in 50 % on sling removal. X-rays showed no elevation of the bladder neck.
In 1990–1993, collaboration with Ulf Ulmsten took place: a permanently implanted tape was required. Polypropylene was the ideal material. In 2003, the neoligament principle was applied as an adjustable “micro” sling to the arcus tendineus fasciae pelvis (ATFP), cardinal, uterosacral ligaments, and perineal body for cure of cystocele, rectocele, and apical prolapse. It was found that symptoms such as urgency, nocturia, chronic pelvic pain, obstructive defecation syndrome (ODS), and fecal incontinence were frequently cured or improved.
Conclusions
The lecture concluded with advice to younger members. Without new paradigms, there are no randomized controlled trials, no meta-analyses, Cochrane. Indeed, no progress. Be open to new concepts. Read Kuhn’s “The Structure of Scientific Revolutions” to understand the discovery process. Examine the relationship among symptoms, ATFP, cardinal, uterosacral ligaments, and the perineal body. This is the next paradigm. Don’t disregard anomalies. Pursue them. They are the pathway to discovery. Innovation is born from challenge, not conformity. Persist, even when meeting resistance. Resistance is a sign that your discovery is important.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
This is a lecture about discovery. It is therefore given within the context of Thomas Kuhn’s classical work, “The Structure of Scientific Revolutions” (73,650 citations). According to Kuhn [1] changes in science emerge by revolution, not evolution. The discovery of the tension-free vaginal tape (TVT) fits Kuhn’s concept of a “scientific revolution.”
Kuhn made two main points:
-
1.
Crisis leads to innovation
-
2.
Anomaly leads to the discovery of new paradigms
The discovery of the TVT artifical neoligament surgical principle began with two unrelated observations. The first observation was that a hemostat applied immediately behind the pubic symphysis at the level of the midurethra controlled urine loss on coughing. The second observation was that Teflon tape created a collagenous tissue reaction around it when implanted.
These observations led to two hypotheses:
-
1.
A loose pubourethral ligament (PUL) causes urinary stress incontinence.
-
2.
A tape implanted in the exact position of a damaged pubourethral ligament would create a collagenous “neoligament” to reinforce it, restoring function and continence.
At this point in the lecture, I would like to acknowledge an intellectual debt to Dr Robert Zacharin [2], whose 1963 anatomical works provided an inspirational starting point for not only TVT, but also the integral theory.
Animal studies
Following human cadaver testing on a half pelvis, an instrument, as shown in Fig 1, was developed that would precisely insert a tape into the position of the PUL to reinforce it [3].
The prototype tunneler was 30 cm long, with a removable insert containing a fairly blunt tip. The inset was reversed once the penetration was made between the vagina and the rectus sheath, so that the tape was protected at all times. The right angle at the distal end allowed the surgeon to know precisely where the tip was located. The vertical handle likewise indicated the lateral direction of the tip
In 1987, animal studies [3, 4] were commenced at the Royal Perth Hospital animal laboratory in conjunction with Professor John Papadimitriou, Professor of Pathology, University of Western Australia, an acknowledged expert researcher on macrophages, tissue reaction to implanted materials, and inflammation. The animal model chosen was a large dog. The aim was to develop and test the surgical methodology and the Mersilene tape for safety, efficacy, and transferability to humans.
The two ends of the tape remained loose in the vaginal cavity for periods ranging from 6 to 12 weeks [5]. The surgical methodology developed for the dogs was similar to that eventually used in the humans [5–7].
Although 10 out of 13 dogs developed abdominal sinuses, they remained afebrile and well at all times, with normal white cell counts. Radioactive gallium studies showed low inflammatory response in the tissues. Serum and wound lactic acid and LDH studies showed raised levels, while the tapes were in situ. Bacteriological studies of the abdominal and vaginal ends of the tape grew no pathogenic bacteria, only mixed organisms. Histology showed macrophages in the interstices of the Mersilene tape, even though it was made of densely knitted multifilament material. A collagenous cylinder formed to surround the tape (Fig 2). This quarantined any bacteria and allowed tape removal by pulling on the vaginal end [3, 4]. The neoligament was initially collagen III, but had commenced conversion to collagen I by 4–6 weeks. On testing for strength, the neoligament pulled out of the tensiometer grips at 0.64 MPa (92 lb/sq inch) [3].
Conclusions from the animal studies
A safe, minimally invasive technique for the creation of an artificial collagenous neoligament was demonstrated. Other than a sticky yellow vaginal discharge, there were no ill effects from having a tape in the vagina for 6–12 weeks [3]. When the tape was removed, the abdominal sinuses closed within 48 h [3, 4]. The absence of pathogenic bacterial growth on the tapes indicated that the macrophages had adequately eliminated the bacteria [3]. The collagen fibers of the neoligament were aligned in linear formation along the tape [3].
Human studies: prototype TVT operations (1988–1989)
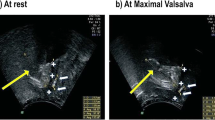
Between 1988 and 1989, 30 women with demonstrable stress incontinence (USI) underwent the prototype TVT operation [5], 25 with mixed incontinence and 5 with only USI. This operation involved insertion of Mersilene tape and removal at 6 weeks as per the animal studies. The tunneler was used to insert the Mersilene tape from the vagina across the rectus sheath (Fig 3) at the level of the midurethra. The tube was secured with interrupted sutures through holes in the distal ends of the tape so that it could be lowered in patients with obstructed micturition by cutting each suture in turn. As the sling was lowered towards the lower end of the symphysis, obstructed urine flow returned to normal and all 30 patients remained continent. Standing lateral X-rays were performed with dye inserted into a Foley catheter balloon before surgery, with the tape in situ, and after removal of the tape during both rest and straining [5].
Prototype tension-free vaginal tape (TVT). Perspective: coronal section immediately behind the pubic symphysis. The tape was configured around the rectus sheath into the vagina, through both ends of a rubber tube, exiting at its inferior end, both ends secured with interrupted sutures in holes set 0.5 cm apart
Results
At the end of 6 weeks, all patients remained continent. In those patients with stress and urge incontinence, the urge incontinence was cured simultaneously with the stress incontinence. However, within 2 weeks of the tape being removed, 50 % of the patients reported simultaneous recurrence of both the stress and the urge incontinence [5]. No bladder neck elevation was seen in any of the patients on post-op xray.
Four anomalies became evident.
-
1.
Stress and urge were cured and recurred simultaneously. Did they have the same origin?
-
2.
Urge incontinence had been surgically cured. This was incommensurable (incompatible) with existing concepts. What was the mechanism for cure?
-
3.
No bladder neck elevation was noted in any of the patients cured of urinary stress incontinence, even in patients where the balloon was sited below the lower end of the symphysis at rest. These data invalidated the pressure equalization theory by Enhorning [8].
-
4.
When the tape was grasped with a hemostat and the patient was asked to strain (Fig 4), three directional vector forces became evident, forward, backward, and downward around the tape. What was their role in urethral closure and urgency control?
Fig. 4 Demonstration of three directional forces acting around the pubourethral ligament (broken lines). On application of a hemostat onto the tape (large arrow) in the position of the pubourethral ligament, three directional forces became evident, backward/downward behind the tape (black arrows) and a forward vector distal to the tape (white arrow). PS pubic symphysis
Birth of a new paradigm: the integral theory
None of these anomalies could be explained using existing concepts. Conceptually, however, the findings were consistent with Kuhn’s comments that it is anomaly that leads to the discovery of new paradigms. A new theory began to evolve. Loose ligaments caused both stress and urge incontinence, albeit for different reasons: inactivation of urethral closure forces for USI and activation of the micturition reflex prematurely for urge incontinence [9].
A full copy of the theory is available on the website www.integraltheory.org
Collaboration with Ulf Ulmsten (1990–1993)
In late 1989, I presented the results of the 30 prototype TVT cases at the Royal Women’s Hospital Melbourne. There I met Ulf Ulmsten for the first time. He was intrigued by the surgery and the results and he visited me in Perth, Western Australia, the next year. Over a period of a week, he reviewed 80 patients and participated in three operating sessions at Royal Perth Hospital. At the end of the week, he said “I think your theory is correct. However, it needs more work.” Our collaboration had commenced.
Over the next 3 years we worked intensively on the further development of what became known as the TVT operation [6, 7]. It soon became evident that a removable tape would only work in half the cases and that a permanent midurethral tape was required. Mersilene was easy to use, non-stretch, and effective, but it had a high erosion rate (14 %). By 1996 polypropylene mesh tape had solved the problem of erosions and become universally accepted [7].
Where are we today (2015)?
The midurethral sling based on reinforcing the PUL has become the gold standard and is already in the category of Kuhn’s “normal science” [1], with hundreds of papers investigating various aspects of the surgery and anatomy. However, we have more crises [1].
-
FDA warnings have highlighted problems with mesh usage.
-
Native tissue repairs have a high failure rate over time.
-
Symptoms such as nocturia, urgency, chronic pelvic pain, abnormal bladder emptying are still considered incurable by “state of the art” publications on these subjects [10].
Yet, an increasing number of publications are confirming that such symptoms can be cured by the surgical repair of posterior fornix laxity [11, 12].
Future directions 2005
Further developments of the TVT paradigm were consistent with Kuhn’s comments: “Crisis leads to innovation.” In 2005, a new surgical tool based on the TVT neoligament surgical principle, an adjustable “micro” sling, was described [13]. Small strips measuring 0.7 mm wide of non-elastic monofilament macropore tape applied precisely to the PUL, uterosacral ligament (USL), arcus tendineus fasciae pelvis (ATFP), cardinal ligaments, and perineal body (Fig. 5) effectively address cystocele, rectocele, uterine prolapse, with high initial cure rates for accompanying symptoms such as urgency, nocturia, chronic pelvic pain, abnormal bladder emptying [12]. Erosion rates similar to those of TVT were reported [12]. This extension of the TVT neoligament paradigm to other ligaments is encouraging, but more extensive and more robust studies will be required before this new direction can emerge as another paradigm.
Top left Suspension of anterior vaginal wall using the TVT neoligament principle. Perspective: looking into the anterior wall of the vagina. The distal inverted U-shaped sling supports the central defect and re-attaches dislocated or loose paravaginal tissues to the arcus tendineus fasciae pelvis (ATFP) at its origins. The proximal transverse sling acts by re-attaching dislocated ATFP to the ischial spine, and then re-attaching dislocated pubocervical fascia and dislocated cardinal ligaments to the anterior cervical ring. Top right Suspension of the apex. Perspective: looking into the pelvic cavity from above. The uterosacral ligaments (USL) sling re-attaches the apex to the sacrum by reinforcing the uterosacral ligaments. The cardinal ligament TFS re-attaches the apex to the lateral side wall. Bottom Suspension of the posterior vaginal wall. Perspective: sitting lateral view. The USL sling re-attaches the apical part of the rectovaginal fascia to the uterosacral ligaments. The distal 50 % of the vagina is supported by repair of the deep transversus perinei, which also repairs descending perineal syndrome
Conclusions
-
Without new paradigms, there are no randomized controlled trials, no meta-analyses, no Cochrane, no science; indeed, no progress.
-
I urge the younger members to read Kuhn “The Structure of Scientific Revolutions.” It will open your minds to the discovery process.
-
Examine the relationship of symptoms to the four suspensory ligaments and perineal body. This is the next paradigm.
-
Do not disregard anomalies. Pursue them. Anomalies are the pathway to discovery.
-
Be open to new concepts.
-
Challenge everything. Innovation is born from challenge, not conformity.
-
Persist, even if you meet resistance. And you will certainly meet resistance, for resistance is a consequence of the incommensurability of competing paradigms.
References
Kuhn T (1996) The structure of scientific revolutions. University of Chicago Press, Chicago, 3rd edn, pp 1–210
Zacharin RF (1963) The suspensory mechanism of the female urethra. J Anat 97(Pt 3):423–427
Petros PEP (1999) Development of the intravaginal slingplasty and other ambulatory vaginal surgical procedures. Doctor of surgery thesis, University of Western Australia
Petros PE, Ulmsten U, Papadimitriou J (1990) The autogenic neoligament procedure: a technique for planned formation of an artificial neo-ligament. Acta Obstet Gynecol Scand Suppl 153:43–51
Petros PE, Ulmsten U (1990) The combined intravaginal sling and tuck operation. An ambulatory procedure for stress and urge incontinence. Acta Obstet Gynecol Scand Suppl 153 69:53–59
Ulmsten U, Petros P (1995) Intravaginal slingplasty (IVS): an ambulatory surgical procedure for treatment of female urinary incontinence. Scand J Urol Nephrol 1:75–82
Ulmsten U, Henriksson L, Johnson P, Varhos G (1996) An ambulatory surgical procedure under local anesthesia for treatment of female urinary incontinence. Int Urogynecol J 7:81–86
Enhorning G (1961) Simultaneous recording of intravesical and intraurethral pressure. A study on urethral closure in normal and stress incontinent women. Acta Chir Scand Suppl 276:1–68
Petros PE, Ulmsten U (1990) An integral theory of female urinary incontinence. Experimental and clinical considerations. Acta Obstet Gynecol Scand Suppl 153 153:7–31
Van Kerrebroeck P, Andersson K-A (2014) Terminology, epidemiology, etiology, and pathophysiology of nocturia. Neurourol Urodyn 33 [Suppl 1]:S2–S5
Lee J, Dwyer P, Rosamilia A, Lim Y, Polyakov A, Stav K (2011) Persistence of urgency and urge urinary incontinence in women with mixed urinary symptoms after midurethral slings: a multivariate analysis. BJOG 118:798–805. doi:10.1111/j.1471-0528.2011.02915.x
Sekiguchi Y, Kinjo M, Maeda Y, Kubota Y (2013) Reinforcement of suspensory ligaments under local anesthesia cures pelvic organ prolapse: 12-month results. Int Urogynecol J 25:783–789. doi:10.1007/s00192-013-2281-x
Petros PEP, Richardson PA (2005) The TFS posterior sling for repair of uterine/vault prolapse—a preliminary report. Aust N Z J Obstet Gynaecol 45:376–379
Conflicts of interest
P. Petros is the co-inventor of TVT. There are no other conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Glossary
- Anomalies
-
Occur with internal logical inconsistencies or especially when experimental findings cannot be explained by the existing paradigm.
- Crisis
-
Crises occur when the dominant paradigm fails to solve problems or when the bases or predictions of the paradigm are invalidated.
- Incommensurability
-
Scientific paradigms preceding and succeeding a paradigm shift are so different that their theories are not able to be judged by the same standards. Nor is the change gradual. “Like a gestalt switch, it must occur all at once, or not at all” [1]. Furthermore, the paradigm shift does not merely involve the revision or transformation of an individual theory, it changes the way in which terminology is defined, how the scientists in that field view their subject, and, perhaps most significantly, what questions are regarded as valid, and what rules are used to determine the truth of a particular theory. Examples: the urodynamic paradigm uses pressure readings to guide whether surgery is performed or not. The integral theory paradigm views prolapse and pelvic symptoms as being mainly secondary to ligament laxity, all being surgically repairable.
- Normal science
-
Is when the paradigm is applied to solve puzzles within the context of the dominant paradigm. Examples are the ICS urodynamic paradigm and the integral theory paradigm
- Paradigm
-
Is a conceptual framework that ultimately leads to a widespread consensus on the appropriate choice of methods, terminology, and on the kinds of experiment that are likely to contribute to increased insights.
- Scientific revolutions
-
A totally different paradigm emerges that seeks to explain the phase in which the underlying assumptions of the field are re-examined and a new paradigm is established.
- Surgical principle of TVT artificial neoligament
-
Using a tape implanted precisely in the anatomical position of a ligament (e.g., pubourethral ligament) to restore its structural function.
Rights and permissions
About this article
Cite this article
Petros, P. Creating a gold standard surgical device: scientific discoveries leading to TVT and beyond. Int Urogynecol J 26, 471–476 (2015). https://doi.org/10.1007/s00192-015-2639-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-015-2639-3