Abstract
Introduction and hypothesis
The objective was to evaluate the effect of myogenic stem cells on histological properties and the volume of striated muscle of the external anal sphincter after transection and repair.
Methods
Histological analysis was performed on the external anal sphincters of 40 young female rats euthanized at 7 or 90 days after transection and repair and randomization to injection of either phosphate buffered solution (PBS) or myogenic stem cells (SC) at the transection site. Sphincter complexes, previously evaluated for neurophysiological function, were processed for histology and analyzed for possible disruption, amount of inflammation, and volume of striated muscle. The relationship between the muscular disruption and contractile force of sphincters was evaluated.
Results
Disruption was seen in 100 % of sphincters 7 days after repair for both SC and control animals. Eighty-nine percent of controls and 78 % of SC-administered animals had intact sphincters at 90 days. Significant inflammatory infiltrate was seen in repaired anal sphincters for both the PBS and the SC groups at 7 days, and persisted at 90 days, with no difference between treatment groups. Striated muscle volume increased from 7 to 90 days for both control and SC-administered animals. Although there was no difference in volume between treatments, there was substantial temporal improvement in contractile force generation of the sphincters receiving SC compared with those receiving PBS.
Conclusion
In this animal model, administration of myogenic stem cells to transected/repaired anal sphincters did not alter the amount of inflammation nor the volume of striated muscle, suggesting that stem cells might improve contractile function through other cellular processes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
One of the major causes of anal incontinence in women is the mechanical disruption of the external anal sphincter [1–3]. Under most circumstances, healing of the external anal sphincter, which is composed mainly of striated muscle, is unremarkable, providing certain conditions are met and select processes involved with healing take place. Events that occur during healing include angiogenesis, fibroblast in-growth and collagen deposition, formation of granulation tissue, epithelial cell proliferation and migration, and wound contraction [4]. In addition to these, the ends of the healing muscle must be in close apposition, myofibroblast proliferation and collagen deposition must occur appropriately, and the necessary growth factors should be present for optimal wound healing. Failure of any one, or a combination, of these criteria can compromise healing and result in persistent disruption or functional impairment of the anal sphincter complex.
There are instances where wound healing is impaired from either a functional or morphological standpoint and enhancing the healing process is desirable. Although stem cell therapy has been shown to be beneficial in the treatment of urinary incontinence secondary to a deficient urethral sphincter [5, 6] and injured detrusor muscle [7], its effects on the anal sphincter have not been clearly defined. Administration of stem cells has shown some potential of improving functional healing of a compromised external anal sphincter. Previously, we demonstrated that local injection of myogenic stem cells at the time of external anal sphincter (EAS) repair resulted in functional improvement with superior contractile function of the sphincter at 90 days compared with repair alone [8]. Others have also demonstrated improvement in contractility [9] and recovery of anal sphincter pressures and electromyographic parameters [10] after injury and subsequent treatment with stem cell injection. However, it was unknown whether stem cell-associated increases in contractile force were accompanied by changes in muscle volume or resulted from alterations of other histomorphological properties.
The objective of this investigation was to evaluate the effect of myogenic stem cells on histological properties and volume of striated muscle of the external anal sphincter after transection with repair.
Materials and methods
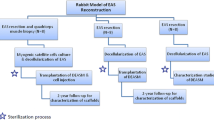
Histological analysis was performed on anal sphincter complexes from 40 young (2–3 months) virginal female Sprague–Dawley rats previously euthanized at 7 or 90 days after undergoing sphincter transection with repair and receiving either phosphate buffered solution (PBS), or myogenic stem cells (SC) at the repair site. They had also undergone prior neurophysiological testing (Fig. 1), the results of which have been previously reported [8].
Research design. Virginal female rats (n = 40) underwent anal sphincter transection with repair and injection with either phosphate-buffered saline (PBS, n = 20) or myogenic stem cells (n = 20) at the transection site. After neurophysiology (previously reported) had been completed at 7 days or 90 days [8], tissues were processed for histology and analysis for both time points
As previously described [8], all procedures were approved by the Institutional Animal Care and Use Committee (IACUC) at the University of Texas Southwestern Medical Center. A 7-mm incision was made through the anal sphincter complex. For the PBS group, each end of the transection was identified microscopically before repair and was injected with 20 μL of PBS using a 20-μL Hamilton syringe (Hamilton, Reno, NV, USA) for a total volume of 40 μL. For the stem cell group, each side of the anal sphincter complex was injected with 1.6 × 106 myogenic stem cells (20 μL) using a 20-μL Hamilton syringe, for a total of 3.2 × 106 cells for each rat. The preparation of myogenic cells was acquired from a commercially available H9c2 myoblast cell line (American Type and Culture Company, Manassas, VA, USA) derived from Sprague–Dawley rats. Cells were cultured in DMEM with 10 % FBS, 25 mM HEPES, and 1 % Ab-Am. To maintain the myoblastic component of the population the cells were subcultured frequently to maintain pre-confluence at all times. Immediately before injection, preconfluent cells were rinsed with PBS and harvested by trypsin (0.25 % v/v)-EDTA (1 mM). Cells (4 × 106) were suspended in PBS (50 μL).
The rectal mucosa was then re-approximated with single interrupted stitches (1 mm apart) of 5–0 braided polyglactin suture (Vicryl; Ethicon, Piscataway, NJ, USA) with a second layer of single interrupted stitches (1 mm apart) of the same suture and caliber used as a reinforcing layer. The external anal sphincter was re-approximated with two single interrupted stitches of 5–0 braided polyglactin suture.
Anal sphincter complexes from animals euthanized at 7 or 90 days after transection and repair previously evaluated for neurophysiologic function [8] were processed for histology. Tissues were fixed at optimal length in neutral buffer formalin (10 %) for 24 h. Five-micrometer cross-sections of formalin-fixed, paraffin-embedded tissues were obtained at 100-μm intervals throughout the entire complex. Tissues were stained with hematoxylin and eosin and analyzed with a Nikon Eclipse E1000N microscope (Nikon Instruments, Melville, NY, USA) for striated muscle volume, graded for the amount of inflammation, and examined for possible disruption.
Volumetric analysis was performed on sphincters from each treatment group. Images of each histological section of sphincter were obtained on Nikon ACT-1c acquisition software version 1.02 (Nikon Instruments). The surface area of striated muscle on each section was imported into, traced, and measured using NIS-Elements AR 2.30 (Nikon Instruments). An estimate of the total volume of striated muscle per sphincter was determined for the 5-μm-thick section of tissue and then by extrapolating the volume between 100-μm serial sections for the entire sphincter complex.
Inflammation was graded by the degree of inflammation present in the histological sections of the anal sphincter complex and were scored as follows: 0 (none—no inflammatory cells); 1 (mild: 1–10 cells per high-power field [HPF]); 2 (moderate: 10–20 cells per HPF); 3 (severe >20 WBC per HPF). For the analysis of sphincter integrity, the striated muscle of the external anal sphincter was identified in sections and noted as intact or disrupted in each section. The sphincter was considered disrupted if an intact ring of striated muscle could not be visualized in any of the sections or if it appeared disrupted in all sections but attenuated in only one section. Also, the relationship between muscular disruption and previously determined values of maximal electrical field stimulation (EFS) of sphincters was evaluated.
As a negative control for sphincter integrity, a group of nonrepaired transected sphincters that had received either PBS or stem cell injection and harvested from animals at 90 days were also processed and examined histologically. Statistical comparisons of sphincter volume in treatment groups were performed using ANOVA with Tukey–Kramer adjustment for multiple testing and for sphincter integrity with Fisher’s exact test. P ≤ 0.05 was considered significant.
Results
The effect of myogenic stem cells on the volume of striated muscle of repaired transected external anal sphincter. The volume of striated muscle of repaired external anal sphincters was evaluated at 7 and 90 days after administration of PBS or myogenic stems cells at the site of sphincter transection (Fig. 2). Seven days after sphincter transection with repair, striated muscle volume was significantly reduced in sphincters injected with either PBS-administered controls or stem cells. There was no significant difference in the volumes between the two groups (P = 0.271) at this time point. Compared with 7 days after transection and repair, mean ± SEM striated muscle volume increased after 90 days for both control animals (7 days, 6.9 ± 0.4 vs 90 days, 11.2 ± 0.8 mm3, P = 0.0005) and those receiving stem cells (7 days, 7.7 ± 0.7 vs 90 days, 11.0 ± 0.5 mm3, P = 0.0002). Further, compared with unoperated controls, the volume of striated muscle increased significantly for both groups. Although there was a trend toward an increased volume in SC-administered animals compared with PBS-administered controls as early as 7 days after repair, there was no statistically significant difference in striated muscle volume between the treatment groups at either 7 days (P = 0.271) or 90 days (P = 0.999).
Effect of myogenic stem cells on histological and inflammatory characteristics of repaired transected external anal sphincter
The sections through the anal canal show circular muscle comprising the internal and external anal sphincters. Subcutaneous adipose tissue and skin could be visualized external to the anal sphincters. Internal to the anal sphincters were mucosa and submucosa. Proximally, the epithelium was colonic. The transition zone was seen more distally, eventually becoming squamous epithelium.
Significant inflammatory infiltrate accompanied repaired anal sphincters of animals receiving PBS (Fig. 3a) or SC at 7 days. Muscle bundles were separated and the space between filled with this acute inflammatory infiltrate and granulation tissue. Further inspection of the disrupted site in these repaired animals at 7 days showed significant amounts of fibroblast in-growth bridging the gap between the ends of the striated muscle. Foreign body, presumably suture material, was also seen surrounded by histiocytes and multinucleated giant cells (Fig. 3d).
Representative cross-sections of repaired anal sphincter complex with myogenic stem cell administration. a Anal sphincter complex of PBS-administered animals at 7 days at low magnification (×10) showing disruption of the external and internal anal sphincter associated with a dense inflammatory infiltrate. b Stem cell-administered anal sphincter complex at 90 days at low magnification (×10). There is suture material, an abscess, and significant amounts of fibroblast in-growth bridging the gap between the ends of the striated muscle. c High magnification (×40) of abscess containing entrapped mucin-like material in stem cell-treated animals at 90 days. d Higher magnification (×200) showing histiocytes and multinucleated giant cells, surrounded by inflammatory cells in stem cell-treated animals at 7 days. abs abscess, d disruption, eas external anal sphincter, epi epithelium lining the internal anal canal, g multinucleated giant cells, ias smooth muscle of the internal anal sphincter, inf inflammation, s suture material
Severe inflammation persisted in both SC- and PBS-administered animals with repaired sphincters at 90 days (Fig. 3b). There was fibrosis and circumferential continuity of muscle was commonly seen in both groups of repaired anal sphincters. Abscesses containing entrapped mucin-like material were present and consisted of lymphocytes surrounding a collection of histiocytes with abundant neutrophils in a central location (Fig. 3c, d).
Effect of myogenic stem cells on external anal sphincter integrity
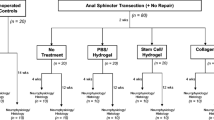
As expected, the external anal sphincter was intact in all unoperated controls. Disruption was seen in 100 % of sphincters 7 days after repair for both SC and control animals. Because of the damage to one sphincter specimen for each treatment group (PBS and SC) during histological processing, analysis at the 90-day time point included only 9 of the 10 sphincters. Eight out of nine PBS-administered controls (89 %) and 7 out of 9 stem cell-administered animals (78 %) had intact sphincters at 90 days, with no statistically significant difference between the two groups (P = 0.527). The relationship between disruption of the external anal sphincter and maximal force generation of the sphincter is illustrated in Fig. 4. At 7 days, as expected with 100 % sphincter disruption, maximal forces in response to EFS were significantly impaired in all sphincters compared with unoperated controls (PBS, 0.9 ± 0.2, P < 0.001; SC, 2.2 ± 0.5 g/sphincter, P < 0.001) [8]. By 90 days, compared with unoperated controls, field-stimulated contractile forces were greater for SC (10.6 ± 1.2 g/sphincter, P < 0.001) as the proportion of intact:disrupted sphincters increased, but not for PBS-administered sphincter-repaired controls (6.4 ± 1.2 g/sphincter, P = 0.9) [8].
Relationship between force generation and disruption of the external anal sphincter at 90 days. The relationship between muscular disruption of the external anal sphincter and the contractile force generation in response to the maximal electrical field stimulation of each sphincter was plotted. The striated muscle of the external anal sphincter was identified in sections and noted as being intact or disrupted in each section. The sphincter was considered disrupted if an intact ring of striated muscle could not be visualized in any of the sections, or if it appeared disrupted in all sections but attenuated in only one section. Each point represents maximal force generation of transected and repaired external anal sphincters injected with either PBS or myogenic stem cells in animals euthanized at 7 (n = 10 for each group) or 90 (n = 9 for each group) days and in sphincters of unoperated controls (n = 10). Force measured in grams per sphincter (g/sphincter). Unoperated controls (purple crosses), PBS 7 days (blue triangles), stem cell 7 days (pink diamonds), PBS 90 days (purple triangles), stem cell 90 days (red diamonds)
The group of nonrepaired transected sphincters harvested from animals at 90 days that had received either PBS or stem cell injection and were used as a negative control for sphincter integrity, all remained disrupted and had minimal to very mild amounts of inflammation.
Discussion
In this animal model of anal sphincter transection with repair, striated muscle volume of the sphincter complex increased significantly for both PBS-administered controls and animals receiving myogenic stem cell injections. Additionally, both treatment groups had an accompanying acute and dramatic inflammatory process that persisted even remote from the injury site.
Wound healing in striated muscle is a complex process that involves degeneration and regeneration of muscle, inflammation, and fibrosis. The role of inflammation in the healing of the external anal sphincter and the balance needed between the proinflammatory and anti-inflammatory pathways in muscle regeneration are unclear. The significant inflammatory component seen in both treatment groups of this current study was unaltered by the administration of myogenic stem cells, suggesting that this amount of inflammation might be a normal sequelae in the healing process. Given the finding that inflammation was more prominent in both of these repaired sphincter groups, we surmise that perhaps it may have been associated with physiological tissue reaction to a foreign body, such as the suture material. Indeed, the normal tissue reactions to acute and chronic healing (the presence of multinucleated giant cells and histiocytes) were seen in the vicinity of the repair site. Furthermore, fewer of these cell types and less inflammation in general were seen in the sphincters of nonrepaired animals.
Although the volume of striated muscle for both treatment groups at 90 days increased compared with unoperated controls, stem cell administration did not have an additional influence on this increase in comparison with PBS-administered controls. Despite this lack of difference in the volume of striated muscle, there was substantial temporal improvement in contractile force generation of the sphincter after injury and repair with animals receiving myogenic stem cells compared with those receiving PBS. Although individual muscle fiber hypertrophy may be an explanation, further study regarding wound healing is necessary before being able to arrive at this conclusion. Interestingly, stem cells did not alter the inflammatory process compared with PBS-administered controls either. Taken together, these findings suggest that there might be other factors or mechanisms (besides merely the volumetric or morphological findings seen in this study) that contribute to the enhanced contractility of the sphincter complex with stem cell administration.
Of note, the beneficial effect of stem cell administration did not appear to translate to nonrepaired sphincters, which had significantly lower proportions of intact:disrupted sphincters, contractile forces, and amounts of inflammation. We speculate that perhaps the ends between the healing musculature might not have been in close enough proximity for local release of growth factors to regulate proliferation and differentiation of myoblasts at the injured site and, in turn, ultimately affected muscle regeneration and repair [11, 12]. Studies are in progress to determine whether enhancement of the microenvironment through matrix reconstruction between the healing ends of the sphincter enhances the reparative potential of stem cells.
Some have reported on the utility of stem cell injection for anal incontinence treatment in humans [13]. Frudinger and co-investigators found that fecal incontinence severity and quality of life improved after injection of autologous myoblasts into sphincters of women with severe anal incontinence [13]. However, the initial increase in anal squeeze pressures seen at 1 and 6 months were transient and not sustained at 12 months. Clearly, further study into the process of injury and wound healing is warranted and we are hesitant to prematurely extrapolate our findings to human application based on our current data.
We acknowledge the limitation that estimation of the striated volume of the sphincter complex was based on the assumptions that there was uniformity to the diameter of the sphincter and that it was a regular torus of tissue. Also, this method of estimation of the volume of striated muscle was associated with some degree of extrapolation, where 5 μm for each 100 μm of semi-serial sectioning was measured, with the remaining volume being extrapolated. The presence of a significant amount of inflammation in the tissue may also have obscured some of the striated muscle component during measurement, resulting in underestimation of the volume of muscle. Additionally, transection and repair of the sphincter in this investigation were performed under ideal surgical conditions, with a precise and clean surgical transection and repair assisted by a dissecting microscope. In practice, injuries usually occur in less optimal conditions where there is potential contamination of the surgical site, irregular tissue planes at the site of injury, and suboptimal visualization and lighting during repair.
In conclusion, this study demonstrates that the administration of myogenic stem cells enhances contractile function of repaired external anal sphincters in an animal model after 90 days, without significantly altering a number of morphological characteristics compared with PBS-treated controls. As we continue to explore the potential role of stem cell therapy in wound healing, our study suggests that, in an animal model, myogenic stem cells might serve as positive adjunctive therapy for a repaired anal sphincter, with no significant histological change from regular healing.
References
American College of Obstetricians-Gynecologists (2006) ACOG Practice Bulletin. Episiotomy. Clinical management guidelines for obstetricians-gynecologists. Number 71, April 2006. Obstet Gynecol 107:957–962
Fornell EK, Berg G, Hallböök O, Matthiesen LS, Sjödahl R (1996) Clinical consequences of anal sphincter rupture during vaginal delivery. J Am Coll Surg 183:553–558
Sultan AH, Kamm MA, Hudson NH, Thomas JM, Bartram CI (1993) Anal-sphincter disruption during vaginal delivery. N Engl J Med 329:1905–1911
Kumar V, Abbas AK, Aster JC, Fausto N (2009) Robbins & Cotran pathologic basis of disease, 8th edn. Saunders/Elsevier, Philadelphia
Cannon TW, Lee JY, Somogyi G, Pruchnic R, Smith CP, Huard J (2003) Improved sphincter contractility after allogenic muscle-derived progenitor cell injection into the denervated rat urethra. Urology 62:958–965
Chancellor MB, Yokoyama T, Tirney S, Mattes CE, Ozawa H, Yoshimura N (2000) Preliminary results of myoblast injection into the urethra and bladder wall: a possible method for the treatment of stress urinary incontinence and impaired detrusor contractility. Neurourol Urodyn 19:279–287
Kwon D, Minnery B, Kim Y, Kim JH, de Miguel F, Yoshimura N, Chancellor MB (2005) Neurologic recovery and improved detrusor contractility using muscle-derived cells in rat model of unilateral pelvic nerve transection. Urology 65:1249–1253
White AB, Keller PW, Acevedo JF, Word RA, Wai CY (2010) Effect of myogenic stem cells on contractile properties of repaired and non-repaired external anal sphincter transection. Obstet Gynecol 115:815–823
Kang SB, Lee HN, Lee JY, Park JS, Lee HS, Lee JY (2008) Sphincter contractility after muscle-derived stem cells autograft into the cryoinjured anal sphincters of rats. Dis Colon Rectum 51:1367–1373
Lane FL, Jacobs SA, Craig JB, Nistor G, Markle D, Noblett KL, Osann K, Keirstead H (2013) In vivo recovery of the injured anal sphincter after repair and injection of myogenic stem cells: an experimental model. Dis Colon Rectum 56:1290–1297
Merly F, Lescaudron L, Rouaud T, Crossin F, Gardahaut MF (1999) Macrophages enhance muscle satellite cell proliferation and delay their differentiation. Muscle Nerve 22:724–732
Warren GL, O′Farrell L, Summan M, Hulderman T, Mishra D, Luster MI, Kuziel WA, Simeonova PP (2004) Role of CC chemokines in skeletal muscle functional restoration after injury. Am J Physiol Cell Physiol 286:C1031–C1036
Frudinger A, Kölle D, Schwaiger W, Pfeifer J, Paede J, Halligan S (2010) Muscle-derived cell injection to treat anal incontinence due to obstetric trauma: pilot study with 1 year follow-up. Gut 59:55–61
Acknowledgement
Supported in part by a research grant from the American College of Obstetricians and Gynecologists/Ortho Women’s Urology Fellowship Training Grant.
Conflicts of interest
None of the authors declare any conflicts of interest with regard to this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fitzwater, J.L., Grande, K.B., Sailors, J.L. et al. Effect of myogenic stem cells on the integrity and histomorphology of repaired transected external anal sphincter. Int Urogynecol J 26, 251–256 (2015). https://doi.org/10.1007/s00192-014-2496-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-014-2496-5