Abstract
Introduction and hypothesis
We aim to report the 3-year outcome and complications of the tension-free vaginal tape obturator (TVT-O) in treating female stress urinary incontinence (SUI).
Methods
Retrospective analysis for complications and outcome of surgery was performed in 419 women undergoing the TVT-O from 2004 to 2006.
Results
Three patients (0.8%) with an isolated TVT-O had a blood loss of more than 200 ml. Two patients (0.5%) had bladder perforation. Out of 11 readmitted patients (2.6%), 10 were due to voiding difficulty. Six patients (1.4%) required tape loosening or division. Persistent pain occurred in 3.6% and erosion in 2.4% of patients. One hundred eighty-five patients (44.2%) came for follow-up at 3 years. The actual subjective and objective success rates were 89.7% and 99.9% at 3 years follow-up, respectively. With imputation, the 3-year subjective and objective success rates were 86.9% and 97.4%, respectively.
Conclusions
The TVT-O is effective in treating female SUI with minimal complications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Stress urinary incontinence (SUI) affects up to 20% of women worldwide and is a social stigma. Multiple behavioral and surgical treatments exist; however, midurethral slings are becoming the gold standard for the correction of SUI [1].
In 2001, Delorme [2] developed the transobturator tape (TOT) which involved passage of the tape through the obturator foramen from outside to inside the vagina. The procedure had comparable cure rates to Ulstem’s tension-free vaginal tape (TVT) with reduced vascular, bladder, and bowel injury as it avoided the space of Retzius. However, it was associated with increased risk of urethral and vaginal injury.
Jean de Leval [3] designed the tension-free vaginal tape obturator (TVT-O) in 2003, placing the tape from inside the vagina to the outside via the obturator foramen, with a reduced incidence of vaginal and bladder injury. Prospective studies of 99 patients in 2006 and 91 patients in 2007 followed up for 1 and 3 years respectively, confirmed high cure rates of 88–91% with no urethral or bladder injury [4, 5]. In 2008, a retrospective study of 102 patients revealed cure rates of 95% with minimal complications [6]. In 2009, a prospective study of 67 patients with 2 years follow-up reported minimal complications [7].
To date, many studies have been done on the TVT-O procedure but none to our knowledge have involved large numbers of patients with longer follow-up duration.
The aim of this study is to report the 3-year outcome and complications of the TVT-O in treating female SUI in a larger group of patients.
Materials and methods
All patients who underwent the TVT-O procedure (Gynecare Worldwide, a division of Ethicon, Inc. Johnson & Johnson) performed or supervised by the same urogynecologist between January 2004 and December 2006 from the Department of Urogynaecology, KK Women’s and Children’s Hospital, Singapore were recruited into the study. This was a retrospective case notes review whereby case notes were requested from the hospital records office and analyzed. Ethical clearance was obtained from the local CIRB prior to proceeding with the study.
All patients who had a TVT-O done had either reported having SUI, which was subjectively troublesome, or had urodynamically proven SUI. In 3 out of 419 women (0.7%), urodynamic study was not performed due to cost constraints. However, before inclusion in the study, it was ascertained that all three did not have documented symptoms of frequency, urgency, or urgency urinary incontinence and all had subjectively troublesome urinary leakage on coughing.
All definitions were in accordance with the latest International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction [8].
The surgical technique used to perform the TVT-O was as originally described by Jean de Leval [3], with the exception that a metal catheter was used to empty the bladder preoperatively and postoperatively as opposed to placing an indwelling catheter from the outset.
Preoperative evaluation consisted of history taking, abdominal and pelvic examination, erect stress test (EST), cough stress test (CST), urinalysis, and multichannel urodynamic study (UDS).
The EST was performed with a subjectively full bladder, with the patient standing over an absorbent sheet and coughing vigorously 10 times. The sheet was then weighed to determine the difference in weight in grams. For the CST, all patients were asked to come for assessment with a full bladder. Before performing the CST, this information was confirmed. Each patient was asked specifically if she had micturated within the last 3 h and, if so, was given 250 ml of water to drink within half an hour, following which the test was performed. The CST was performed with the patient lying down with a subjectively full bladder and coughing vigorously for up to three times. Any demonstrable urinary incontinence was taken as a positive test. UDS consisted of uroflowmetry, multichannel micturating cystourethrogram, and urethral pressure profilometry (Medtronic Duet Logic G/2) but excluded video urodynamics.
Postoperative evaluation consisted of history taking, abdominal and pelvic examination—with UDS and CST at 6 months, and only CST at 1, 2, and 3 years follow-up.
Patient demographics, namely, age, parity, body mass index (BMI), menopausal status, usage of hormone replacement therapy (HRT), and previous surgery; operative details, namely, concomitant surgery, duration of surgery, type of anesthesia, and blood loss; and intraoperative complications, namely, hematoma formation, urethral injury, bladder perforation, vascular injury, and excessive blood loss were recorded. Excessive blood loss was documented in two categories: ≥200 ml and ≥1 L.
Perioperative details, namely, length of hospital stay, number of catheterization days, the presence of voiding difficulty, need for tape loosening or division, presence of fever >37.5°C, groin or thigh pain, and patient readmissions were recorded in two categories: isolated TVT-O and TVT-O with concomitant surgery. The perioperative period was defined as <2 weeks from the date of surgery.
Voiding difficulty was defined as residual urine of more than 150 ml determined by bladder scan (BladderScan BVI 3000, Diagnostic Ultrasound United Kingdom Ltd) or by in–out catheterization. The bladder scan or in–out catheterization was performed immediately after micturition but had to be at least 6 h following urinary catheter removal. Fever was recorded in two categories: 37.6–37.9°C and ≥38.0°C. With regards to pain documentation, patients were asked specifically as to the presence of thigh or groin pain. Their responses were documented as “yes” or “no” in a standardized fashion.
Postoperative complications, the presence of groin or thigh pain, tape erosion, voiding difficulty, need for tape division or loosening, and de novo urgency urinary incontinence were documented in five categories: 2 weeks to <6 months, 6 months, 1 year, 2 years, and 3 years post-surgery.
Subjective cure rates, improved rates, and failure rates were detailed at 6 months, 1 year, 2 years, and 3 years. Subjective cure was defined as the patient reporting the absence of SUI after surgery. Improvement was defined as the patient still having SUI but reporting an improvement following the surgery. Failure was defined as the patient still having SUI of the same severity after the surgery.
Objective cure rates and failure rates with the CST were documented at 6 months, 1 year, 2 years, and 3 years with postoperative UDS performed at 6 months follow-up.
The primary outcome measure was cure rate, improvement rate, and failure rate of the TVT-O procedure. The secondary outcome measures were the intraoperative and perioperative occurrence of hematoma formation, urethral injury, bladder perforation, vascular injury, excessive blood loss, voiding difficulty, tape loosening or division, fever >38°C, groin or thigh pain, and patient readmissions and the postoperative occurrence of groin or thigh pain, tape erosion, voiding difficulty, tape loosening or division, and de novo urgency urinary incontinence.
Data was analyzed using the Microsoft Excel statistical analysis package and the SPSS version 14.
Results
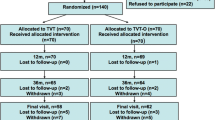
Between January 2004 and December 2006, 422 patients underwent the TVT-O procedure at our urogynecology department, either performed or supervised by the same urogynecologist. Three patient case notes were unavailable for analysis and thus these patients were excluded from the study. The patient demographics, operative characteristics, and intraoperative complications are as outlined in Table 1.
Bladder perforation occurred in two patients. The first patient had an isolated TVT-O. The second patient with a bladder perforation had a concomitant anterior prolift with the perforation occurring during sharp dissection of the periurethral space with a Metzembaum scissors. Following the perforation, an indwelling urinary catheter was kept for 2 days and the patients received antibiotics for 1 week. Both the patients with bladder injury recovered well.
Three out of 178 patients (1.7%) had an isolated TVT-O with blood loss ≥200 ml. Three out of 241 patients (1.2%) who had concomitant surgery had a blood loss ≥1 L—out of which 1 patient with a vaginal hysterectomy had an exploratory laparotomy performed due to intra-abdominal bleeding, revealing a bleeding ovarian ligament. Blood loss was 1.1 L and 2 pints of blood was transfused. The patient was discharged after 3 days.
Perioperative outcome was recorded in two groups as detailed in Table 2. Voiding difficulty occurred in 47 patients (11.2%), with 11 patients (6.2%) having an isolated TVT-O and 36 patients (14.9%) having concomitant surgery. Twenty-four of these 36 patients (9.9%) had an anterior repair or anterior prolift. Readmission was required in 11 patients (2.6%), with 10 patients being readmitted for voiding difficulty. A further 2 out of these 10 patients required tape loosening on the 8th and 13th postoperative day for high residual urines ranging from 700 to 1,350 ml. One patient had an isolated TVT-O and the other had concomitant vaginal hysterectomy and pelvic floor repair. Following tape loosening, residual urine reduced to 50–80 ml.
One patient with a concomitant hysterectomy and pelvic floor repair was readmitted for vaginal bleeding on the 13th postoperative day, having reported vaginal bleeding with clots soaking two sanitary pads. She did not have a temperature and her hemoglobin did not drop significantly from preoperative values. An ultrasound scan of the pelvis was normal. There was no documented bleeding during the inpatient stay and the patient was discharged the following day.
Forty patients (9.5%) developed a temperature of >37.5°C, out of which this persisted beyond the second postoperative day till the fourth postoperative day in 2 patients who had had concomitant total abdominal hysterectomy and bilateral salpingo-oophorectomy. One had an ovarian malignancy. None of the patients had urinary tract infections.
Thigh or groin pain occurred in 175 patients (41.8%). In 156 out of 175 patients (89.1%), pain resolved in <1 week. Postoperative complications are detailed in Table 3. In 7 out of 175 patients (4.0%) who had pain persisting beyond the perioperative period, it resolved by the second postoperative month with the use of nonsteroidal anti-inflammatory analgesics. In 12 out of 175 patients (6.9%) who had pain persisting beyond the perioperative period, pain persisted till 6 months follow-up. At 12 months follow-up, 2 out of the 12 patients who had pain at 6 months still had pain which did not persist in the second or third year. One patient had a previous TVT with anterior repair complicated by bladder perforation 3 years ago. The other patient had an isolated TVT-O.
Seven patients (1.7%) had tape erosion on follow-up at 2 weeks to <6 months. In three patients, the erosion recurred at 6 months. It resolved in one patient at further follow-up but persisted in the other two patients at 1 and 2 years follow-up, respectively. Eight patients had tape erosion diagnosed at 6 months follow-up—out of which five had newly diagnosed erosion and three had recurrent erosion. Three patients had tape erosion diagnosed at 1 year follow-up—out of which one had newly diagnosed tape erosion and two had recurrent erosion.
Two patients had tape erosion at 2 years follow-up—out of which one had newly diagnosed tape erosion and the other one had recurrent erosion. In the single patient with newly diagnosed erosion at 2 years, there was no recurrence at 3 years follow-up. This patient had a concomitant dilatation and curettage with histology reported as endometrial adenocarcinoma. Abdominal computed tomography and pelvic resonance imaging suggested early stage malignancy, hence a vaginal hysterectomy and bilateral salpingo-oophorectomy was performed. This was complicated by the development of a vesicovaginal fistula which was repaired 6 weeks later.
In all patients, the vaginal erosions occurred at the lateral vaginal sulcus and the area exposed was small. Hence, the eroded tape was trimmed in clinic followed by insertion of estradiol 25-μg pessaries at night for 2 weeks and then biweekly up till 3 months.
Eight patients had voiding difficulty from 2 weeks to <6 months which did not persist at further follow-up—out of which one patient with a high residual urine required tape loosening at 22 days postoperatively.
At 6 months follow-up, three patients had voiding difficulty which persisted in two of them at 1 year follow-up. Both had had a concomitant vaginal hysterectomy necessitating tape division due to persistent high residual urines.
One out of these three patients had an isolated TVT-O and defaulted follow-up at 1 year but had voiding difficulty at the 2-year follow-up requiring tape division. Postoperatively, residual urines remained high at 280 ml, necessitating CISC. This patient did not have preoperative voiding difficulty.
De novo urgency urinary incontinence occurred in eight patients (2.4%) at 6 months, three patients (1.1%) at 1 year, and one patient (0.5%) at 3 years follow-up. At 2 years follow-up, none had urgency urinary incontinence.
Table 4 details the subjective and objective outcomes of the TVT-O procedure and the use of various assumptions and imputations to deal with defaulter data. At 6 months and 3 years follow-up, 332 patients (79.2%) and 185 patients (44.2%) came for review, respectively. At 6 months, 306 patients had both UDS and CST done, with 12 patients (3.9%) having conflicting results. The subjective cure rate, improvement rate, and failure rate was 92.7%, 6.9%, and 0.3% and 89.7%, 10.3%, and 0% at 6 months and 3 years, respectively. The objective cure rate and failure rate by UDS was 94.4% and 5.6% at 6 months, respectively. The objective cure rate, improvement rate, and failure rate by CST was 97.6%, 2.4%, and 0% and 99.9%, 0.1%, and 0% at 6 months and 3 years, respectively.
Assuming all the defaulters were failures or cured at 3 years, the subjective and objective cure rates were 39.6% and 43.9%, 95.5% and 99.8%, respectively. Using imputation with the carrying forward of the last observed results, the subjective and objective cure rates at 3 years were 86.9% and 97.4%, respectively.
Discussion
In the last 5 years, the transobturator midurethral slings have become more popular for the surgical management of SUI due to minimal complications and a high cure rate of 85–90%, which compares favorably with the TVT retropubic slings [9, 10].
In our study, the objective cure rate by UDS at 6 months was 94.4%, which is similar to the SUI cure rates using the TVT-O as quoted in the literature [4–7, 11, 12]. The objective assessment of outcome with the UDS has already been proven to be a reliable measure [13, 14].
Utilizing the CST as the objective measure of outcome, the cure rate at 6 months was slightly higher at 97.6%. Of 306 patients (3.9%) who had both the UDS and CST done at 6 months, 12 had conflicting results. Statistical model using the chi-square test comparing CST with UDS as a reliable outcome measure had a p value of 0.096, which is not statistically significant, assuming a 95% confidence level. This suggests that the CST may be as reliable as the UDS when used as an objective measure of SUI [15, 16].
The objective cure rate of 94.4% using the UDS was also similar to the subjective cure rate of 92.7% at 6 months. However, a validated measure of subjective outcome of the TVT-O was not used, for example, a standardized quality of life health questionnaire or, more recently, patient-selected goals, which are the third and fourth dimensions in the assessment of pelvic floor disorders, respectively [17–19]. The objective cure rate was 99.9% using the CST at 3 years. However, the subjective cure rate at 3 years was only 89.7%. This difference may be because the CST was performed with a subjectively full bladder which was not standardized. However, all patients were asked to come for assessment with a full bladder or failing which they were asked to drink 250 ml of water over half an hour. In the literature, it has also been reported that the CST may be performed with an empty bladder or filled up to 300 ml or to subjective fullness [20] and in an upright or lithotomy position, with the patient performing a series of forceful coughs. Despite the limitation of the CST being performed with a subjectively full bladder, we were able to show by comparing our UDS and CST results at 6 months that the CST may be a good surrogate for the UDS.
Due to the high defaulter rate of over 50% at 3 years, we attempted to assess the impact of losses to follow-up using various assumptions as detailed in Table 4. Assuming all defaulters were failures or cured, the subjective and objective cure rates at 3 years, respectively, were very low—39.6% and 43.9% or very high—99.5% and 99.8%. Therefore, a more reliable method of dealing with the defaulter data appeared to be the use of imputation to carry forward the last available result giving subjective and objective cure rates at 3 years of 86.9% and 97.4%, which corresponded with the actual results of 89.7% and 99.9%, respectively.
Complications following the TVT-O quoted in the literature include bladder and urethral injury, mesh erosion, persistent groin pain, neuropathies, hematomas, abscesses, and osteomyelitis [21–26]; however, the incidence of perioperative and postoperative complications is low [4, 11, 12].
In our study, there were no urethral injuries and a low bladder perforation rate of 0.5%. Our mesh erosion rate was 1.7% at <6 months and 2.4% at 6 months, which is higher than the estimated rate of up to 1% [27]. Erosion rates are directly related to the biomechanical properties of the tape with macroporous monofilament tapes with pore size >75 μm being associated with the lowest rates. Erosion is also more likely to happen in infection with poor tissue healing and can be related to poor surgical technique [21].
We used type I polypropylene mesh and gave prophylactic antibiotics for 5 days. All procedures were also performed or supervised by the same urogynecologist. All erosions occurred at the lateral vaginal sulcus, suggesting initial superficial insertion. However, erosion occurred in only one case in the first year (2004) of study, making poor surgical technique unlikely. Atrophic postmenopausal tissue may be related to defective healing, making erosion more likely [21]. However, only two patients with erosion were postmenopausal and, therefore, we are unable to explain the reason for our high erosion rate and this requires further study.
Concomitant anterior repair may carry a higher risk of developing voiding difficulty, as found in the study by Domingo et al. [28]. In our study, voiding difficulty in the immediate postoperative period was also higher at 9.9% in those with additional anterior repair or anterior prolift, compared to 6.2% and 5.0% in those with an isolated TVT-O and TVT-O with concomitant surgery excluding anterior repair or anterior prolift, respectively. In de Leval’s [4] study, 4 out of 253 patients (1.6%) required tape release or division. The incidence of persistent voiding difficulty in our study was similar, with a total of 6 out of 419 patients (1.4%) requiring tape loosening or tape division.
The incidence of vascular injuries quoted by Walgreny [27] was 0.3%. In our study, 16 out of the 19 patients (6.6%) who had a blood loss of at least 200 ml had concomitant surgery performed, which may account for the higher blood loss. We did not have any documented hematomas, but in the single patient who had had a concomitant vaginal hysterectomy and pelvic floor repair and was readmitted for vaginal bleeding, it is possible that the source of bleeding was from a hematoma which had drained prior to the performance of the pelvic ultrasound scan which was normal.
The quoted rates for de novo urge symptoms range from 0% to 13.9% [27] due to different studies using varying definitions of de novo urgency. The incidence of de novo urgency urinary incontinence in our study was up to 2.4%, with the definition in accordance with the latest IUGA/ICS recommendations [8].
de Leval [3] reported a high incidence of pain of 16%, which may be due to the careful recording of pain presence. However, the pain usually abated within two postoperative days.
The incidence of pain in our study was also high, occurring in 175 patients (41.8%) and may be because any groin or thigh pain or discomfort was recorded as actual pain. As the tape passes through the adductor compartment, one would expect most patients to have some discomfort. Unfortunately, we did not employ a visual analogue scale to grade the pain but the pain was short-lived, resolving in <1 week in the majority of patients (89.1%) and a further 4% by the second postoperative month.
Lim et al. [29] and Descazeaud et al. [30] quoted a 3% and 6% incidence of persistent pain, respectively, which was similar to our incidence of persistent pain at 6 months (3.6%). Out of the two patients who had persistent pain at 1 year, in the first patient, it may have been due to the formation of structural adhesions because of tape tensioning caused by previous scarring [24] secondary to the previous anterior repair and TVT. In the second patient, pain may be due to adductor motion causing tension on the tape leading to distortion or pulling of the groin tissue or may be a neuropathic pain caused by entrapment of the anterior branch of the obturator nerve [24]. The pain was not disabling and both patients declined further investigation.
Severe infectious complications following the TVT-O procedure are rare [5]. We did not have any patients developing severe infections. Despite the 9.5% incidence of postoperative fever, it persisted beyond the immediate postoperative period of 2 days in only two patients and did not persist beyond 4 days.
This study has its limitations. For one, it is a retrospective review with a high attrition rate. Additionally, validated measures of subjective outcome were not used. The use of imputation however revealed similar subjective and objective outcomes to actual data.
The strengths of this study include the large numbers of patients available for review with long follow-up despite the high dropout rate and that all procedures were performed or supervised by the same surgeon, limiting operator bias.
In conclusion, our study shows that the TVT-O is an effective surgical treatment for SUI with minimal complications. However, better studies, preferably appropriately designed large prospective randomized control trials with long-term follow-up, are needed to determine if the TVT-O outcome is as quoted here and in the literature.
Abbreviations
- TVT-O:
-
Tension-free vaginal tape obturator
- TVT:
-
Tension-free vaginal tape
- TOT:
-
Transobturator tape
- CIRB:
-
Central Institutional Review Board
- SUI:
-
Stress urinary incontinence
- IUGA:
-
International Urogynecological Association
- ICS:
-
International Continence Society
- EST:
-
Erect stress test
- CST:
-
Cough stress test
- UDS:
-
Urodynamic study
- BMI:
-
Body mass index
- HRT:
-
Hormone replacement therapy
- CISC:
-
Clean intermittent self-catheterization
References
Bemelmans BL, Chapple CR (2003) Are slings now the gold standard treatment for the management of female urinary stress incontinence and if so which technique? Curr Opin Urol 13:301–307
Delorme E (2001) Trans-obturator urethral suspension: a minimally invasive procedure to treat female stress urinary incontinence. Prog Urol 11:1306–1313
de Leval J (2002) Novel surgical technique for the treatment of female stress urinary incontinence: transobturator vaginal tape inside-out. Eur Urol 44:724–730
Waltregny D, Reul O, Mathantu B, Gaspar Y, Bonnet P, de Leval J (2006) Inside out transobturator vaginal tape for the treatment of female stress urinary incontinence: interim results of a prospective study after a 1-year minimum follow up. J Urol 175:2191–2195
Waltregny D, Gaspar Y, Reul O, Hamida W, Bonnet P, de Leval J (2008) TVT-O for the treatment of female stress urinary incontinence: results of a prospective study after a 3-year minimum follow-up. Eur Urol 53:401–410
Feng CL, Chin HY, Wang KH (2008) Transobturator vaginal tape inside out procedure for stress urinary incontinence: results of 102 patients. Int Urogynecol J Pelvic Floor Dysfunct 19:1423–1427
Su TH, Huang WC, Lee MY, Lin TY, Chang HC, Chen CP (2009) Tension-free vaginal tape-obturator procedure for treatment of severe urodynamic stress incontinence: subjective and objective outcomes during 2 years of follow-up. J Obstet Gynaecol 35(6):1077–1082
Haylen BT, Ridder D, Freeman RM et al (2010) An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Int Urogynecol J Pelvic Floor Dysfunct 21:5–26
Liapis A, Bakas P, Giner M, Creatsas G (2006) Tension-free vaginal tape versus tension-free vaginal tape obturator in women with stress urinary incontinence. Gynecol Obstet Invest 62:160–164
Wang W, Zhu L, Lang J (2009) Transobturator tape procedure versus tension-free vaginal tape for treatment of stress urinary incontinence. International Journal of Gynecology and Obstetrics 104:113–116
Debodiance P (2006) Trans-obturator urethral sling for the surgical correction of female stress urinary incontinence: outside-in (Monarc) versus inside-out (TVT-O). Are the two ways reassuring? Eur J Obstet Gynecol RB 133:232–238
Liapis A, Bakas P, Creatsas G (2007) Monarc vs TVT-O for the treatment of primary stress incontinence: a randomized study. Int Urogynecol J 19:185–190
Homma Y, Batista J, Bauer S et al (2002) Urodynamics. In: Abrams P, Cardozo L, Khoury S et al (eds) Incontinence: 2nd International Consultation on Incontinence, Plymouth, UK, p 317
Massey A, Abrams P (1985) Urodynamics of the female lower urinary tract. Urol Clin North Am 12:231–246
Scotti RJ, Myers DL (1993) A comparison of the cough stress test and single-channel cystometry with multichannel urodynamic evaluation in genuine stress incontinence. Obstet Gynecol 81:430–433
Wall LL, Wiskind AK, Taylor PA (1994) Simple bladder filling with a cough stress test compared with subtracted cystometry for the diagnosis of urinary incontinence. Am J Obstet Gynecol 171:1472–1479
Mouritsen L, Larsen JP (2003) Symptoms, bother and POPQ in women referred with pelvic organ prolapse. Int Urogynecol J Pelvic Floor Dysfunct 14:122–127
Brubaker L, Shull B (2005) EGGS for patient-centered outcomes. Int Urogynecol J Pelvic Floor Dysfunct 16:171–173
Hullfish KL, Bovbjerg VE, Christianson LM, Steers WD (2005) Achieving pelvic floor dysfunction (PFD) treatment goals in medically versus surgically managed patients. 26th Annual Scientific Meeting of the American Urogynecologic Society, Atlanta, USA
Swift SE, Yoon EA (1999) Test–retest reliability of the cough stress test in the evaluation of urinary incontinence. Obstet Gynecol 94:99–102
Robert M, Murphy M, Birch C, Swaby C, Ross S (2006) Five cases of tape erosion after transobturator surgery for urinary incontinence. Obstet Gynecol 107:472–474
Abdel-Fattah M, Ramsay I, Pringle S (2006) Lower urinary tract injuries after transobturator tape insertion by different routes: a large retrospective study. BJOG 113(12):1377–1381
Rafii A, Jacob D, Deval B (2006) Obturator abscess after transobturator tape for stress urinary incontinence. Obstet Gynecol 108(3):720–723
Roth TM (2007) Management of persistent groin pain after transobturator slings. Int Urogynecol J 18:1371–1373
Rajan S, Kohli N (2005) Retropubic hematoma after transobturator sling procedure. Obstet Gynecol 106:1199–1202
Haensel A, Naumann G, Hohle P, Rommens PM, Koelbl H (2007) Osteomyelitis following a transobturator sling (TVT-O). BJOG 114(12):1577–1579
Waltregny D, de Leval J (2009) Review article: the TVT-obturator surgical procedure for the treatment of female stress urinary incontinence: a clinical update. Int Urogynecol J 20:337–348
Domingo S, Alama P, Ruiz N, Lazaro G, Morell M, Pellicer A (2007) Transobturator tape procedure outcome: a clinical and quality of life analysis of a 1-year follow-up. Int Urogynecol J Pelvic Floor Dysfunct 18:895–900
Lim JL, Quinlan DJ (2006) Safety of a new transobturator suburethral synthetic sling (TVT-O) procedure during the training phase. J Obstet Gynaecol Can 28(3):214–217
Descazeaud A, Salet-Lizee D, Villet R (2007) TVT-O treatment of stress urinary incontinence: intermediate and one-year results. Gynecol Obstet Fertil 35(6):523–529
Acknowledgements
The authors would like to thank Miss Michelle (research assistant) for her hard work in helping produce this paper; Mr. Wei Xing and Mr. Ng Mor Jack for their statistical input; Dr. Sarita Narang for data collection; and Mrs. Asmah Sani and Mrs. Valemmah Kannapathy from the hospital records department for their help in collecting patient case notes.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rajendra, M., Han, H.C., Lee, L.C. et al. Retrospective study on tension-free vaginal tape obturator (TVT-O). Int Urogynecol J 23, 327–334 (2012). https://doi.org/10.1007/s00192-011-1552-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-011-1552-7