Abstract
Introduction and hypothesis
The objective of this study was to determine the effect of external anal sphincter repair on fecal incontinence symptoms, quality of life, and anal sphincter squeeze pressures.
Methods
The fecal incontinence symptoms and impact on quality of life, patient satisfaction, and anorectal manometry were assessed pre- and post-operatively.
Results
One hundred four women were eligible and 74/104 (71%) returned post-operative questionnaires. Fifty-four of 74 (73%) had pre- and post-operative questionnaires. Twenty-five of 74 (34%) had pre- and post-operative anorectal manometry measures. Mean length of follow-up for participants (n = 54) was 32 ± 19 months. Modified Manchester Health Questionnaire scores decreased from 47.3 ± 21.9 to 28.4 ± 24.3 (p < 0.01) and Fecal Incontinence Severity Index scores from 30.6 ± 13.0 to 21.6 ± 15.5 (p < 0.01). Seventy-seven percent of the participants was satisfied. Sphincter squeeze pressures increased from 53.4 ± 25.0 to 71.8 ± 29.1 mmHg (p < 0.01).
Conclusions
External anal sphincter repair resulted in sustained improvements in fecal incontinence severity and quality of life along with improved anal sphincter squeeze pressures.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Fecal incontinence (FI), the involuntary loss of feces that is a social or hygienic problem, affects 4–24% of women [1–7]. FI has devastating consequences and is a major reason for admission to nursing home care [8]. FI prevalence increases with age and will become a greater burden as the U.S. population continues to age [1, 2].
However, in younger women, vaginal delivery may result in mechanical and neurologic damage to the pelvic floor and cause FI [9, 10]. Damage to the pelvic floor may include a defect in the external and/or internal anal sphincters. Other causes of FI may be iatrogenic injuries resulting from procedures such as hemorrhoidectomy or sphincterotomy.
External anal sphincter (EAS) repair is a common treatment for FI with an evident muscular EAS defect. Short- and medium-term reports of anal sphincter repairs have shown success rates up to 86% [11]. However, longer-term success rates (69–120 months) have ranged from 14% to 80% [10, 12–16]. Results following anal sphincter repair vary in the literature reflecting dissimilar populations, inconsistent FI measures, a variety of definitions of treatment response, and surgical technique [10–17]. Furthermore, these studies do not include any validated measure of patient satisfaction or symptom improvement and most describe their outcome as “cure” vs “no cure.” Repair of the external anal sphincter is a part of the multicomponent treatment for fecal incontinence and, therefore, success should be measured by its ability to improve symptoms rather than to cure them.
Three studies have assessed post-operative changes in anal squeeze pressures with anorectal manometry (ARM) after sphincter repair and reported inconsistent changes in EAS squeeze pressure improvement. Two of the studies had very short-term follow-up and showed improvements in squeeze pressures [18, 19]. The one longer-term study showed no difference in squeeze pressures after 45 months of follow-up [20].
The aim of this study was to describe changes in FI symptom severity, quality of life, and patient satisfaction using validated measures to assess degree of improvement. We also aimed to describe changes in anal squeeze pressures at a minimum of 12 months after surgical repair.
Materials and methods
Participants in this study were 104 women with fecal incontinence who presented to the University of Alabama at Birmingham between January 1, 2003 and April 1, 2009 and subsequently underwent an EAS repair. All participants had a defect of the EAS identified by physical examination and/or endoanal ultrasound. Demographic information, medical history, preoperative symptoms and severity of FI, risk factors, baseline ARM, and endoanal ultrasound findings were collected from a combination of an institutional review board-approved database and clinic chart abstraction. The complications were abstracted from the medical record and were defined as wound breakdown, abscess, or reoperation. The UAB Institutional Review Board approved all data collection and all participants provided informed consent.
External anal sphincter repair was performed under general anesthesia with the patient in the dorsal lithotomy position. A horizontal incision was made along the vaginal introitus. The distal vaginal epithelium was sharply dissected off of the perineal body. Metzenbaum scissors were used to dissect around the external anal sphincter and its surrounding capsule in order to optimally mobilize. End to end repair was performed by reapproximating the ends of the EAS capsule and muscle. Overlapping repair was performed when the length of available EAS allowed. The sphincter was sutured using 0-polydioxanone. In the case of a partial sphincter tear where there was partial intact sphincter and capsule, the residual muscle was not cut, but was incorporated into the closure. The vaginal epithelium was repaired using polyglactin 910 delayed absorbable suture. Other pelvic floor repairs were performed and included hysterectomy, prolapse repairs, and midurethral slings as indicated.
Health-related quality of life (HR-QOL) and FI symptoms were assessed using the Modified Manchester Health Questionnaire (MMHQ), a previously validated measure that also includes the Fecal Incontinence Severity Index (FISI) [21]. The MMHQ measures HR-QOL for FI and includes eight subscales: overall impact, role, physical, social, relationships, emotion, sleep/energy, and severity/adaptation. The MMHQ is scaled from 0 to 100, for total and subscale scores, where higher scores represent greater impact on HR-QOL. The FISI measures the severity of liquid, solid, mucus, or gas incontinence that occurs from “2 or more times per day,” “once per day,” “2 or more times per week,” “once a week,” to “1–3 times per month.” Patient-weighted scores were used to determine severity of symptoms with scores ranging from 0 to 61, where higher scores indicate worse FI severity. A FISI score of 0 indicated continence.
The SF-12 was utilized to measure the general impact of FI on HR-QOL [22]. The SF-12 has two summary scores, the Physical Component Summary (PCS) and the Mental Component Summary (MCS), which assess physical and mental functioning, respectively. The PCS and MCS are scaled from 0 to 100, with higher scores indicating better QOL. Participant satisfaction with surgery was assessed using the validated Patient Satisfaction Question (PSQ) and the Patient Global Impression of Improvement (PGI-I). The PGI-I and PSQ are validated indices of global response to medical and behavioral therapy for urinary incontinence and for prolapse surgery [23, 24]. There is no validated measure for assessing global response to procedures for the treatment of FI, thus we adopted the PSQ and PGI-I and utilized them for the condition under study. The PSQ consists of a single item, “How satisfied are you with your progress?” The three possible responses are “completely,” “somewhat,” and “not at all.” The PGI-I consists of a single item, “Check the number that best describes how your post-operative fecal incontinence condition is now compared with how it was before you had the surgery.” There are seven possible responses ranging from “very much better” to “very much worse.”
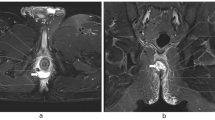
Women referred for FI treatment provided baseline data on their medical and surgical histories and completed questionnaires. Sixty of 104 (57.7%) of all patients undergoing surgery had complete preoperative questionnaires. The participants were mailed follow-up questionnaires at a minimum of 12 months following external anal sphincter repair. They were also asked to return to UAB for a follow-up ARM. At baseline ARM was completed by a physician using a water-perfused disposable catheter system (Medtronic, Inc, Minneapolis, MN). Pressures were recorded during resting, squeezing, and pushing at 1-cm intervals starting at 3 cm from the anal verge. Rectal capacity was measured in milliliters using an air-filled balloon. To evaluate for disruption of the internal and external anal sphincters prior to surgery, endoanal ultrasounds were performed using a 10-MHz, 360° window endoanal probe at 5-mm intervals (B&K Medical Systems, Inc, Wilmington, MA). Women who returned for ARM underwent the same procedures using the same equipment and protocol.
The characteristics of participants with and without both pre- and post-operative questionnaires were compared using Pearson chi-square tests for categorical measures and the Student t test for continuous measures. Fisher’s exact test and the Wilcoxon rank-sum test were used where nonparametric counterparts where appropriate. The paired t test was used to identify differences in the baseline assessment for the FISI, MMHQ, MMHQ subscales, and ARM findings compared with the follow-up scores. The signed rank test was used as a nonparametric counterpart where appropriate. Multivariable logistic regression was used to investigate baseline FISI score, age, BMI, and overlapping sphincter repair as potential predictors of a decrease in FISI score of greater than or equal to 3.56 points (minimum clinically important difference) [25]. These are recognized as measurable factors that may impact on fecal incontinence outcomes after sphincter repair. SAS 9.2 (SAS Institute, Cary, NC) was used for all statistical analyses. An alpha level of 0.05 indicated statistical significance and all tests were two sided.
Results
All women (n = 104) who underwent external anal sphincter repairs from January 2003 to April 2009 were identified; 74/104 (71%) responded to the follow-up questionnaire. Subjects (n = 54/74, 73%) who completed both pre- and post-operative questionnaires comprised our primary analytic sample. Mean ± SD time from surgery for participants (n = 54) was 32 ± 19 months (median 32, range 12–87). Important baseline demographic and clinical information for our responders and non-responders are presented in Table 1. The mean age was 49.2 ± 13.4 years and the majority was non-Hispanic white participants (85%) with a mean BMI of 29.6 ± 8.4. There were no significant differences in important baseline demographic or clinical characteristics and FISI score between the analyzed sample and non-responders. The only significant difference between the analyzed sample (n = 54) and non-responders was a higher rate (44% vs 24%, p = 0.03) of midurethral slings.
Overlapping repairs were performed on 21/54 (39%) and concurrent pelvic organ prolapse surgery was performed in 37/54 (69%) of subjects. Concurrent apical support procedures were performed on 4/54 (7.4%) of subjects. Concurrent rectocele repairs without graft material were performed on 33/54 (61.1%) of subjects. One subject (2%) had a post-operative perineal abscess that resulted in wound breakdown.
Significant improvements were seen in HR-QOL and FI symptoms as measured by mean MMHQ scores decreasing from 47.3 ± 21.9 to 28.4 ± 24.3 (p < 0.01) and mean FISI scores from 30.6 ± 13.0 to 21.6 ± 15.5 (p < 0.01; Table 2). Significant improvements were also seen in all subscale scores of the MMHQ (Table 3). The health-related QOL scale that saw the greatest improvement was “impact” on quality of life (69.0 to 43.1, p < 0.01). Fifty-three percent of the participants reported that their symptoms were “very much better” or “much better.” Seventy-eight percent of the participants reported that they were “completely” or “somewhat” satisfied with their progress (Table 2). A total of 9/54 (16.7%) were completely continent for stool at follow-up. There was no difference in post-operative FI symptom scores in responders that had both pre- and post-operative questionnaires (n = 54) as compared to those who only had complete post-operative questionnaires for analysis (n = 19).
Overall general QOL as measured by the SF-12 showed no improvements in the mental component summary score, but a small improvement in the physical component summary score was found (p = 0.03; Table 2). ARM testing in a subset of women (n = 25) demonstrated significant increases in resting (p = 0.02) and squeeze pressures (p < 0.01; Table 4).
In the multivariable model including increasing age, BMI, baseline FISI score, and type of sphincter repair, none were associated with achieving a minimum clinically important change in FISI score (p > 0.05).
Discussion
Women who underwent an EAS repair, and were assessed greater than 1-year after surgery, experienced improvement in fecal incontinence symptom distress, bowel-specific impact on QOL, and perceived that their condition was improved. Resting and squeeze EAS pressures increased significantly after physiologic evaluation with anorectal manometry post-EAS repair in a subset of women. Patients with evident muscle defects in the anal sphincter who had a repair obtained modest, durable clinical improvements post-operatively.
Short- and medium-term improvements (7–29 months) in FI have been previously reported after EAS repair to be as high as 86%, as defined by continence as measured by St. Marks Incontinence Scoring [11]. However, longer-term studies (40–120 months) have reported successful outcomes from EAS repair ranging from 14% to 80% of subjects [10, 12–16]. This large range of successful outcomes may be a result of different primary outcome measures utilized for symptom characterization and the definitions of treatment success or different patient populations. None of these studies included a validated measure of patient satisfaction.
Minimum clinically important differences (MID) have recently been reported for the FISI and MMHQ in women with fecal incontinence [25]. Estimates of a MID of 3 and 4 points were reported for the MMHQ and the FISI, respectively, in a cohort of 133 subjects undergoing both behavioral and surgical treatment for fecal incontinence corresponding to improvement of one scale on the PGI-I scale 3 months post-treatment. Improvement in the MMHQ score that we report (18.9 points) exceeds the cut off (16.9 points) that corresponds to a patient global impression of being “much better.” Improvements in the FISI score reported here (9 points) exceeds the cut off (4.7 points) that corresponds to a patient global impression of “a little better” and approaches the cut off (11.5 points) that corresponds to “much better.” This finding is consistent with the patient global impression of improvement that we report of “much better.” Therefore, improvements in MMHQ and FISI score correlate similarly with the PGI-I in our study, at a mean/median of 32 months post-surgical repair. This finding further validates the recently reported MID for the FISI and MMHQ.
Our finding of increased squeeze pressure (baseline, 53.1 mmHg; post-operative, 71.8 mmHg) after anal sphincter repair on ARM is similar to two short-term studies and is dissimilar to one longer-term study [18–20]. The short-term studies had only 6 weeks and 12 weeks of follow-up time after surgery [18, 19]. The one study (n = 38) with longer-term outcomes at 45.2 months demonstrated a higher baseline squeeze pressure (mean 73.6 mmHg) and no significant improvement in post-operative squeeze pressure (mean 81.9 mmHg) [20]. Our findings suggest that increases in post-operative squeeze pressures that are noted in other studies of shorter duration follow-up may endure to a mean follow-up time of 32 months.
The increase in squeeze pressure after EAS repair may be important. It has been previously reported that fair/strong EAS contraction on a digital rectal examination was associated with a positive change in FISI score in women treated with combined pharmacologic therapy and pelvic floor muscle exercises [26]. One small trial (n = 31) that compared EAS repair alone with EAS repair with biofeedback showed no overall difference in continence rates, but significant differences in favor of repair with biofeedback was found in quality of life scores for higher lifestyle, less depression, and less embarrassment as measured by the Fecal Incontinence Quality of Life Scale [27].
This study is limited by a moderately small sample size, response rate, limited racial representation, performance at a single site, and the lack of post-operative ARM data for some participants. Also, 50% (27/54) of our sample underwent post-operative behavioral therapy and this may have influenced fecal incontinence outcomes. We were unable to robustly assess the effect of behavioral therapy due to variations in therapy, performance by multiple providers, variability in the temporal relationship of therapy to surgery, and variations in the indications for the use of behavioral therapy. This study is strengthened by a mean and median of 32 months follow-up, the use of validated measures, the assessment of patient satisfaction, and global impression of improvement and ARM findings. Improved symptoms may have also been affected by a contribution of other pelvic floor surgery that was performed in a majority of patients.
In conclusion, anal sphincter repair resulted in improvements in FI symptom distress, symptom-specific impact on quality of life, and increased EAS resting and squeeze pressures. Women who underwent anal sphincter repair reported overall symptom improvement. A recent Cochrane review revealed that there are no acceptable randomized trials comparing EAS repair and non-surgical management [17]. Future research evaluating the effect of adjunctive behavioral/medical therapy in the setting of anal sphincter repair may help to improve long-term outcomes and durability after surgical intervention for FI.
References
Whitehead WE, Borrud L, Goode PS, Meikle S, Mueller ER, Tuteja A, Weidner A, Weinstein M, Ye W, Pelvic Floor Disorders Network (2009) Fecal incontinence in US adults: epidemiology and risk factors. Gastroenterology 137:512–517
Nygaard I, Barber MD, Burgio KL, Kenton K, Meikle S, Schaffer J, Spino C, Whitehead WE, Wu J, Brody DJ, Pelvic Floor Disorders Network (2008) Prevalence of symptomatic pelvic floor disorders in US women. JAMA 300:1311–1316
Melville JL, Fan MY, Newton K, Fenner D (2005) Fecal incontinence in US women: a population-based study. Am J Obstet Gynecol 193:2071–2076
Goode PS, Burgio KL, Halli AD, Jones RW, Richter HE, Redden DT, Baker PS, Allman RM (2005) Prevalence and correlates of fecal incontinence in community-dwelling older adults. J Am Geriatr Soc 53:629–635
Varma M, Brown JS, Creasman JM, Thom DH, Van Den Eeden SK, Beattie MS, Subak LL, Reproductive risks for incontinence study at Kaiser (RRISK) research group (2006) Fecal incontinence in females older than aged 40 years: who is at risk? Dis Colon Rectum 49:841–851
Bharucha AE, Zinsmeister AR, Locke GR, Schleck C, McKeon K, Melton LJ (2006) Symptoms and quality of life in community women with fecal incontinence. Clin Gastroenterol Hepatol 4:1004–1009
Macmillan AK, Merrie AEH, Marshall RJ, Parry BR (2004) The prevalence of fecal incontinence in community dwelling adults: a systematic review of the literature. Dis Colon Rectum 47:1004–1009
Kamm MA (1998) Faecal incontinence. BMJ 316:528–532
Abramov Y, Sand PK, Botros SM, Gandhi S, Miller JJR, Nickolov A, Goldberg RP (2005) Risk factors for female anal incontinence: new insight through the Evanston Northwestern Twin Sisters Study. Obstet Gynecol 106:726–732
Malouf AJ, Norton CS, Engel AF, Nicholls RJ, Kamm MA (2000) Long-term results of overlapping anterior anal-sphincter repair for obstetric trauma. Lancet 355:260–265
Young CJ, Mathur MN, Eyers AA, Solomon MJ (1998) Successful overlapping anal sphincter repair: relationship to patient age, neuropathy, and colostomy formation. Dis Colon Rectum 41:344–349
Halverson AL, Hull TL (2002) Long-term outcome of overlapping anal sphincter repair. Dis Colon Rectum 45:345–348
Bravo Gutierrez A, Madoff RD, Lowry AC, Parker SC, Buie WD, Baxter NN (2004) Long-term results of anterior sphincteroplasty. Dis Colon Rectum 47:727–732
Zorcolo L, Covotta L, Bartolo DC (2005) Outcome of anterior sphincter repair for obstetric injury: comparison of early and late results. Dis Colon Rectum 48:524–531
Maslekar S, Gardiner AB, Duthie GS (2007) Anterior anal sphincter repair for fecal incontinence: good longterm results are possible. J Am Coll Surg 204:40–46
Karoui S, Leroi A, Koning E, Menard J, Michot F, Denis P (2000) Results of sphincteroplasty in 86 patients with anal incontinence. Dis Colon Rectum 43:813–820
Brown SR, Washawan H, Nelson RL (2007) Surgery for faecal incontinence in adults. Cocnhrane Database Syst Rev 2:CD001757
Gearhart S, Hull T, Floruta C (2005) Anal manoetric parameters: predictors of outcome following anal sphincter repair? J Gastro Surg 9:115–120
Zutshi M, Salcedo L, Hammel J, Hull T (2010) Anal physiology testing in fecal incontinence: is it of any value? Int J Colorectal Dis 25:277–282
Evans C, Davis K, Kumar D (2006) Overlapping anal sphincter repair and anterior levatorplasty: effect of patient’s age and duration of follow-up. Dis Colon Rectum 21:795–801
Kwon S, Visco AG, Fitzgerald MP, Ye W, Whitehead WE, Pelvic Floor Disorders Network (2005) Validity and reliability of the Modified Manchester Health Questionnaire in assessing patients with fecal incontinence. Dis Colon Rectum 48:323–331
Jenkinson C, Layte R, Jenkinson D, Lawrence K, Petersen S, Paice C, Stradling J (1997) A shorter form health survey: can the SF-12 replicate results from the SF-36 in longitudinal studies? J Public Health Med 19:179–186
Yalcin I, Viktrup L (2007) Comparison of physician and patient assessments of incontinence severity and improvement. Int Urogynecol J Pelvic Floor Dysfunct 18:1291–1295
Srikrishna S, Robinson D, Cardozo L (2010) Validation of the patient global impression of improvement (PGI-I) for urogenital prolapse. Int Urogynecol J 21:523–528
Jelovsek JE, Chen Z, Markland AD, Brubaker L, Dyer KY, Meikle S, Rahn DD, Siddiqui NY, Tuteja A, Barber MD (2010) Minimum important differences for scales assessing symptom severity and quality of life in patients with fecal incontinence. Supplement to Fem Pelv Med Recon Surg S66
Markland AD, Richter HE, Burgio KL, Wheeler TL, Redden DT, Goode PS (2008) Outcomes of combination treatment of fecal incontinence in women. Am J Obstet Gynecol 199:699e1–699e7
Davis KJ, Kumar D, Poloniecki J (2004) Adjuvant biofeedback following anal sphincter repair: a randomized study. Aliment Pharmacol Ther 20:539–549
Acknowledgments
National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) ARRA Administrative Supplement 3K24DK068389-05S1 and 2DK24-DK068389 granted financial support to HER.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Oral presentation of this study was made at the 37th Annual Meeting of the Society of Gynecologic Surgeons at San Antonio, TX, on April 11–13, 2011.
Rights and permissions
About this article
Cite this article
Gleason, J.L., Markland, A., Greer, W.J. et al. Anal sphincter repair for fecal incontinence: effect on symptom severity, quality of life, and anal sphincter squeeze pressures. Int Urogynecol J 22, 1587–1592 (2011). https://doi.org/10.1007/s00192-011-1551-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-011-1551-8