Abstract
Introduction and hypothesis
We evaluated the outcomes and the effect of the Macroplastique Implantation System on the quality of life in women with stress incontinence with or without a history of an anti-incontinence operation during 12 to 62 months follow-up.
Methods
Thirty-five women with urodynamically proven stress incontinence with intrinsic sphincter deficiency were included in this study. Macroplastique injection was performed in all patients. Quality of life was evaluated prior to therapy, in early postoperative time (at the sixth weeks) and in late postoperative time (12 to 62 months follow-up) with the use of three different questionnaires: Incontinence Quality-of-Life Questionnaire (I-QOL), Incontinence Impact Questionnaire-7 (IIQ-7), and Urogenital Distress Inventory-6 (UDI-6). Questionnaires were also compared with those previous to the anti-incontinence operation and to the primary procedure groups.
Results
The median age of the women was 50.00 (interquartile range = 17.00) years. There were 24 primary procedures and 11 had undergone previous anti-incontinence surgery. Maximum follow-up time was 62 months, minimum follow-up time was 12 months, and the median follow-up time of the study was 58 (interquartile range = 44–60) months. When preoperative and postoperative median of the I-QOL, IIQ-7, and UDI-6 scores were compared, the differences between scores were found to be statistically significant. I-QOL, IIQ-7, and UDI-6 scores were related to the previous surgery. The overall I-QOL, IIQ-7, and UDI-6 summary scores showed high internal consistency.
Conclusions
The Macroplastique injection system is an effective, safe, and acceptable option for stress urinary incontinence in women with or without a history of an anti-incontinence operation. Moreover, it can be performed under local anesthesia without cystoscopic guidance; moreover, side effects are rare.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The quality of life for women with urinary incontinence is negatively affected. However, treatment of urinary incontinence is sometimes unsatisfactory both for patients and physicians. There is dissatisfaction especially among those women who have a history of a previous anti-incontinence operation yet have ongoing complaints.
Stress urinary incontinence is defined by the International Continence Society as involuntary urine leakage on effort or exertion, such as with sneezing or coughing, without rise in detrusor pressure [1]. The etiology for stress urinary incontinence is multifactorial: childbirth, aging, menopause, connective tissue weakness, or previous surgery [2]. The cause may be extrinsic, poor anatomic support of the urethra and bladder neck hypermobility resulting in incontinence. Alternatively, urethral failure may be intrinsic, impaired sphincter function due to loss of elasticity and may respond to sphincter augmentation procedures, including periurethral bulking agents. Intrinsic sphincter deficiency has been diagnosed by either a low maximum urethral closure pressure, a low leak point pressure on subtracted cystometry, or an open bladder neck at rest in the absence of a bladder contraction during video urodynamics [1, 3].
For the treatment of stress urinary incontinence in adult women, there is currently a broad variety of therapies. They range from physiotherapy to surgical intervention [2, 4]. A wide range of surgical procedures is available for stress urinary incontinence. However, a proportion of patients are not suitable for anesthesia, or cannot afford the recuperation time following major surgery. Injectable urethral bulking agents may act as a first line of treatment for these patients and offer a solution for those who fail initial surgery. For these patients, periurethral bulking agents are a minimally invasive procedure offering a shorter procedure and hospitalization time with a short recovery period and low morbidity using local anesthesia without cystoscopic guidance.
Macroplastique® is a bulking agent that consists of solid polydimethylsiloxane particles with a mean maximum diameter of 209 μm [5]. After injection, these particles seem to be nonmigratory and will be organized within 6 to 8 weeks in firm nodules with infiltrated collagen and surrounded by a fibrous sheath that is well developed at 9 months [6, 7].
In this study, we evaluated the efficacy of the Macroplastique Implantation System as a minimally invasive procedure and compared quality of life in urinary incontinent women with or without a previous anti-incontinence operation during 12 to 62 months follow-up.
Materials and methods
We evaluated 35 women with urinary stress incontinence with or without a history of a previous incontinence surgery during 12 to 62 months follow-up. Quality of life was evaluated prior to therapy, at the sixth weeks (early postoperative time) and at the 12–62 months (late postoperative time) postoperatively with the use of three different questionnaires.
The patients were evaluated preoperatively by urogynecologic examination including dipstick urinalysis, urine culture, cotton-tipped swap test (Q-tip test) for assessment of bladder neck excursion, and multichannel urodynamic study. The Q-tip test was considered positive if the excursion of a cotton swab placed in the proximal urethra measured during straining exceeded 30° [8]. Pelvic organ prolapse was assessed by using the Baden scale [9] in standing position. By way of addition, a frequency–volume chart and 1-h International Continence Society pad test [10] were performed.
In a urodynamic study, Valsalva leak point pressure was measured for a validated tool to assess urethral function allowing an estimation of the relative contributions of intrinsic sphincter deficiency and urethral hypermobility [11]. The inclusion criteria for Macroplastique injection were as follows: urodynamic stress urinary incontinence and urethral hypermobility, urodynamic assessment of stress incontinence and Valsalva leak pressure point <60 cm water, no pelvic organ prolapse, negative dipstick urinalysis, and postvoid residual urine <100 ml.
The Incontinence Quality of life Questionnaire (I-QOL) [12], Incontinence Impact Questionnaire-7 (IIQ-7) [13], and Urogenital Distress Inventory-6 (UDI-6) [13] (see “Appendix”) were used in this study for evaluation of effect of Macroplastique injection to quality of life. The Turkish-translated and validated versions were used in this study [14, 15].
The I-QOL Questionnaire score lies theoretically between 1 and 5, and the higher the score is, the more satisfied patients are about their continence condition. IIQ-7 and UDI-6 scores lie theoretically between 1 and 3, and the lower scores indicate a positive impact on their continence condition. This study was approved by the Fatih University Ethical Committee and complied with the Helsinki Declaration, including current revisions, and the Good Clinical Practice guidelines. Before surgery, patients received written and verbal information on the purpose and the procedures of the operation, and an informed written consent was obtained from all of them.
The procedure was performed under local anesthesia and in sterile conditions. As prophylaxis postoperatively cefazolin 250 mg twice daily was given for 5 days. The Macroplastique injections were carried out using the Macroplastique Implantation System which consists of a set of three syringes of Macroplastique (2.5 ml), implantation device, and special needles (Figs. 1 and 2). The Macroplastique implantation device is used to standardize the location of periurethral injection as described by Henalla et al. [16]. Three deposits were placed at positions 10 mm distal to the bladder neck as shown in Fig. 3. The injections were administered to the 2, 10, and 6 o’clock points of urethra. Patients were allowed to go home the same day when comfortable and voiding. If the patient was unable to pass urine spontaneously within 3 to 4 h following the procedure, “in and out catheterization” with a catheter 12 was performed to relieve any symptoms of urinary retention. If residuals of more than 100 ml were detected, the patient was followed up in the hospital till voiding.
Statistical analysis
Continuous variables were first inspected for normality of the statistical distribution graphically and by Shapiro–Wilk test. Data are reported as mean ± SD or median with interquartile ranges, as appropriate. Categorical data are presented by frequencies and percentages. To analyze I-QOL, IIQ-7, and UDI-6 data, the general total scale was calculated and then transformed to a 0 to 100 scale for greater interpretability, with the higher scores in I-QOL representing greater quality of life.
Fridman variance analysis was used to examine changes in I-QOL, IIQ-7, and UDI-6 scores. To compare the preoperative, early postoperative, and preoperative late postoperative I-QOL, IIQ-7, and UDI-6 scores, the Bonferroni corrected Wilcoxon signed rank test was used. For non-normally distributed variables, the Mann–Whitney test was used to verify similarity of medians for baseline characteristics. Reliability of the I-QOL, IIQ-7, and UDI-6 were assessed in the form of internal consistency by Cronbach’s alpha coefficient, and values greater than 0.7 were considered acceptable. Statistical analysis was performed using the Statistical Package for the Social Sciences 13 (SPSS Inc., Chicago, IL, USA). P values ≤0.05 were used to define significance in all statistical comparisons.
Results
Thirty five women who elicited the inclusion criteria were included in the study. The median age was 50.00 (interquartile range (IQR) = 17.00) years.
The patients were seen at the sixth weeks after surgery (early postoperative time). In late postoperative time (12 to 62 months), the patients were interrogated by telephone questionnaire. Maximum follow-up time was 62 months, minimum follow-up time was 12 months, and the median follow-up time of the study was 58 (IQR = 44–60) months. We could not contact one woman because of address and phone number change, and one woman refused to answer the questionnaire because of dementia.
Eleven of the patients had a history of a previous anti-incontinence surgery. Three of them had histories of previous Burch colposuspension with laparotomy, and two of them had previous laparoscopic Burch colposuspension. Two of the patients underwent tension-free transvaginal tape, three of them underwent colporaphy anterior–posterior with Kelly plication, and one of the patients previously underwent hyaluronic acid injection. Table 1 shows the demographic characteristics of the patients.
Treatment duration was approximately 5 min. There were no serious complications after the procedure. Five of the patients (14.7%) were unable to pass urine spontaneously within 3 to 4 h following the procedure; “in and out catheterization” with a catheter 12 was performed to relieve any symptoms of urinary retention. If residuals of more than 100 ml were detected, the patient was followed up in the hospital till voiding.
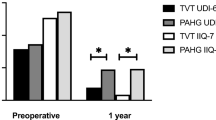
When we examined changes in I-QOL, IIQ-7, and UDI-6 scores by time, statistical significance was found (χ 2 = 61.140, p < 0.01; χ 2 = 63.748, p < 0.01; χ 2 = 61.600, p < 0.01, respectively). When preoperative and postoperative medians of I-QOL, IIQ-7, and UDI-6 scores were compared, the difference between scores was found to be statistically significant (Table 2; Fig. 4). One of the patients developed de novo bladder overactivity after injection.
I-QOL, IIQ-7, and UDI-6 scores were unrelated to the patient’s age, parity, body mass index, type of delivery, menopausal status, need of pediatric use, history of drug use for urinary incontinence, or type of incontinence. The patients who had a history of a previous anti-incontinence treatment were more satisfied with the procedure. There were statistical differences between the previous anti-incontinence surgery group and primary procedure group for I-QOL scores (Z = 4.546, p < 0.001; Z = 4.053, p < 0.001; Z = 3.685, p < 0.001, respectively).
When we analyzed the differences in scores between the previous anti-incontinence surgery group with the others, IIQ-7 and UDI-6 median scores had a statistically significant difference in all periods except the median of preoperative IIQ-7 scores (IIQ-7: Z = 1.410, p = 0.183; Z = 3.653, p < 0.001; Z = 3.559, p < 0.001; UDI-6: Z = 3.428, p < 0.001; Z = 3.586, p < 0.001; Z = 3.356, p < 0.001, respectively; Table 3). The overall I-QOL, IIQ-7, and UDI-6 summary scores showed high internal consistency (Table 4).
Discussion
Treatment of urinary incontinence is a dilemma both for patients and physicians, especially in women with a history of a previous anti-incontinence operation and having continuing complaints. They admit to the hospital in a less satisfied situation. Periurethral bulking agents are a minimally invasive procedure offering a shorter procedure and hospitalization time with a short recovery period and low morbidity.
In their study, Peeker et al. presented their experience of periurethral injection of silicone microimplants and concluded that this may be performed as an outpatient procedure, and moreover, side effects are rare [17]. In another study, Tamanini et al. evaluated the 12-month follow-up outcome of the Macroplastique Implantation System for the treatment of stress urinary incontinence caused by intrinsic sphincter deficiency; 57.1% of their patients considered themselves cured, 19% of them were improved, and 23.8% of them had failure. They concluded that the Macroplastique Implantation System had an acceptable outcome for patient and surgeon [18]. In another study, Tamanini et al. evaluated long-term follow-up treatment with the Macroplastique Implantation System. The overall subjective success rate was 80%. They concluded that it should be considered a good option for certain cases of female SUI [19].
Ghoniem et al. evaluated the durability of the urethral bulking agent Macroplastique for stress urinary incontinence in a 24-month study in women with a previously documented successful outcome, 12 months after the last injection. Substantial, durable results were sustained for 2 years with 84% of patients maintaining significant. The durability of Macroplastique shows its effectiveness as a viable long-term therapy for female stress urinary incontinence primarily due to intrinsic sphincter deficiency [20]. In a prospective randomized controlled trial, Meulen et al. evaluated the efficacy of Macroplastique® in women without previous incontinence surgery. There was a significant higher increase of Incontinence Quality-of-Life Questionnaire. They concluded that Macroplastique implantation was an acceptable option for women with SUI and urethral hypermobility [7].
In our study, similar to those literatures, there was a significant improvement after Macroplastique implantation procedure in women with stress incontinence with or without anti-incontinence surgery. For preoperative I-QOL scores, there was a significant result in favor of previous surgery group. This significant result might be due to the fact that woman had previous surgery. But there was also significant improvement after the procedures for I-QOL scores. Our procedure might be a supplementary procedure for our previous surgery patients.
A remarkable result in our study was that there were statistically significant differences between incontinence questionnaires and quality of life between the women with and without a history of an anti-incontinence operation. The women with a history of a previous anti-incontinence operation were more satisfied with the procedure. This may be attributable to a previously inappropriate treatment or may be because they were already disappointed and had lower expectations from the procedure. Another prospect was that Macroplastique implantation might have been a supplementary procedure for previous surgery patients.
In the present study, one patient was treated with previously performed dextranomer/hyaluronic acid and her complaints returned 12 months later. We performed Macroplastique for this patient, and the 60-month results were positive.
The noteworthy difference in our study was that we included patients who had undergone previous unsuccessful anti-incontinence surgical procedures and we compared the results of Macroplastique injection in these patients with the results of the patients who received a primary Macroplastique injection. Since Macroplastique implantation is a minimally invasive intervention, it can be accepted as an alternative treatment for SUI. Especially when general anesthesia is not suitable for old patients with associated systemic medical problems, Macroplastique implantation can be the first choice of treatment. Moreover, when the long-term results of this procedure are taken into consideration, as a minimally invasive technique, Macroplastique implantation already seems to be the primary choice of treatment for young and otherwise healthy women.
To conclude, treatment of urinary incontinence is a dilemma both for patients and physicians. Expectations of both cosmetic and functional improvement from urinary incontinence treatment are complicated in providing a complete success. To choose an appropriate treatment for urinary incontinence is important. Physicians should also take into account the expectations of patients. Nonetheless, as presented in our study, the Macroplastique Implantation System is a feasible and effective procedure for stress incontinence caused by intrinsic sphincter deficiency. Long-term success rates are remarkable. It can be performed under local anesthesia without cystoscopic guidance, and moreover, side effects are rare.
References
Abrams P, Cardozo L, Fall M et al (2002) The standardisation of terminology of lower urinary tract function: report from the Standardisation Sub-committee of the International Continence Society. Am J Obstet Gynecol 187:116–126
Hay-Smith EJ, BO K, Berhmans LC, et al (2003) Pelvic floor muscle training for urinary incontinence in women. Cochrane Database Syst Rev CDOO1407
Lightner DJ (2002) Review of the available urethral bulking agents. Curr Opin Urol 12(4):333–338
Shah J (1997) Injectables and stress urinary incontinence. Urol News 2:7–11
Solomon LZ, Birch BR, Cooper AJ, Davies CL, Holmes SAV (2000) Nonhomologous bioinjectable materials in urology: ‘size matters’? BJU Int 85:641–645
Radley SC, Chapple CR, Lee JA (2000) Transurethral implantation of silicone polymer for stress incontinence: evaluation of a porcine model and mechanism of action in vivo. BJU Int 85:646–650
Meulen H, Berghmans M, Nieman M, Kerrebroeck V (2009) Effects of Macroplastique Implantation System for stress urinary incontinence and urethral hypermobility in women. Int Urogynecol J 20:177–183
Karram MM, Bhatia NN (1988) The Q-tip test: standardization of the technique and its interpretation in women with urinary incontinence. Obstet Gynecol 6:807–811
Baden W, Walker TA (1972) Physical diagnosis in the evaluation of vaginal relaxation. Clin Obstet Gynecol 15:1055–1061
Abrams P, Blaivas JG, Stanton SL, Anderson JT (1998) The standardization of terminology of lower urinary tract function. The International Continence Society Committee on Standardization of Terminology. Scand J Urol Nephrol 114:5–19
Cummings JM (1997) Leak point pressures in female stress urinary incontinence. Int Urogynaecol J 8:153–155
Wagner TH, Patrick DL, Bavendam TG et al (1996) Quality of life in persons with urinary incontinence: development of a new measure. Urology 47:67–72
Uebersax JS, Wyman JF, Shumaker SA, McClish DK, Fantl JA (1995) Short forms to assess life quality and symptom distress for urinary incontinence in women: the Incontinence Impact Questionnaire and the Urogenital Distress Inventory. Continence Program for Women Research Group. Neurourol Urodyn 14(2):131–139
Cam C, Sakalli M, Ay P, Cam M, Karateke A (2007) Validation of the Short Forms of the Incontinence Impact Questionnaire (IIQ-7) and the Urogenital Distress Inventory (UDI-6) in a Turkish population. Neurol and Urodynamics 26:129–133
Eyigor S, Karapolat H, Akkoc Y, Yesil H, Ekmekci O (2010) Quality of life in patients with multiple sclerosis and urinary disorders: reliability and validity of Turkish-language version of Incontinence Quality of Life Scale. J Rehabil Res Dev 47:67–72
Henalla SM, Hall V, Duckett JRA, Link C, Usman F, Tromans PM et al (2000) A multicentre evaluation of a new surgical technique for urethral bulking in the treatment of genuine stress incontinence. Br J Obstet Gynecol 107:1035–1039
Peeker R, Edlund C, Wennberg L, Fall M (2001) The treatment of sphincter incontinence with periurethral silicone implants (Macroplastique). Scand J Urol Nephrol 36:194–198
Tamanini JT, D’Ancona CA, Tadini V, Netto NR Jr (2003) Macroplastique implantation system for the treatment of female stress urinary incontinence. J Urol 169:2229–2233
Tamanini JT, D'Ancona CA, Netto NR (2006) Macroplastique implantation system for female stress urinary incontinence: long-term follow-up. J Endourol 20:1082–1086
Ghoniem G, Corcos J, Comiter C, Westney OL, Herschorn S (2010) Durability of urethral bulking agent injection for female stress urinary incontinence: 2-year multicenter study results. J Urol 183:1444–1449
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Appendices
Appendix
I-QOL Instrument
Q1. I worry about not being able to get to the toilet on time.
Q2. I worry about coughing and sneezing.
Q3. I have to be careful about standing up after sitting down.
Q4. I worry where the toilets are in new places.
Q5. I feel depressed.
Q6. I don’t feel free to leave my home for long periods of time.
Q7. I feel frustrated because my UI prevents me from doing what I want.
Q8. I worry about others smelling urine on me.
Q9. Incontinence is always on my mind.
Q10. It’s important for me to make frequent trips to the toilet.
Q11. Because of my incontinence, it is important to plan every detail in advance.
Q12. I worry about my incontinence getting worse as I grow older.
Q13. I have a hard time getting a good night’s sleep.
Q14. I worry about being embarrassed or humiliated because of my incontinence.
Q15. My incontinence makes me feel like I’m not a healthy person.
Q16. My UI makes me feel helpless.
Q17. I get less enjoyment out of life because of my UI.
Q18. I worry about wetting myself.
Q19. I feel like I have no control over my bladder.
Q20. I have to watch what I drink.
Q21. My UI limits my choice of clothing.
Q22. I worry about having sex.
All items use the following response scale:
-
1
Extremely
-
2
Quite a bit
-
3
Moderately
-
4
A little
-
5
Not at all
IIQ-7
The questions below refer to areas in your life that may have been influenced or changed by your problem.
For each question, circle the response that best describes how much your activities, relationships, and feelings are being affected by urine leakage.
Has urine leakage affected your…
-
1.
Ability to do household chores (Cooking, housecleaning, laundry)?
-
2.
Physical recreation such as walking, swimming, or other exercise?
-
3.
Entertainment activities (movies, Concerts, etc.)?
-
4.
Ability to travel by car or bus more than 30 minutes from home?
-
5.
Participation in social activities outside your home?
-
6.
Emotional health (nervousness, depression, etc.)?
-
7.
Feeling frustrated?
All items use the following response scale:
-
Not at all 0
-
Slightly 1
-
Moderately 2
-
Greatly 3
UDI-6
Do you experience, and if so, how much are you bothered by:
-
1.
Frequent urination?
-
2.
Urine leakage related to the feeling of urgency?
-
3.
Urine leakage related to physical activity, coughing, or sneezing?
-
4.
Small amounts of urine leakage drops?
-
5.
Difficulty emptying your bladder?
-
6.
Pain or discomfort in the lower abdominal or genital area?
-
Not at all 0
-
Slightly 1
-
Moderately 2
-
Greatly 3
Rights and permissions
About this article
Cite this article
Gumus, I.I., Kaygusuz, I., Derbent, A. et al. Effect of the Macroplastique Implantation System for stress urinary incontinence in women with or without a history of an anti-incontinence operation. Int Urogynecol J 22, 743–749 (2011). https://doi.org/10.1007/s00192-011-1398-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-011-1398-z