Abstract
We set out to identify predictors of successful voiding immediately after outpatient mid-urethral sling. The charts of 126 patients who underwent an outpatient mid-urethral sling procedure were identified. Using discharge without a urinary catheter as the dependent variable, logistic regression analysis modeled the relationship of independent variables including demographic, preoperative urodynamic, and perioperative variables. Sixty-one percent of the patients passed their immediate postoperative voiding trial. Logistic regression analysis revealed that parity ≥3, Valsalva leak point pressure >60 cm H2O, and high preoperative anxiety remained independently associated with successful voiding. Identifying preoperative variables that are associated with successful voiding after mid-urethral sling may be useful in helping to accurately shape patient expectations and identify those most likely to benefit from preoperative teaching of self-catheterization.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Stress urinary incontinence is increasingly being recognized as a problem of epidemic proportions for women across the globe [1, 2]. An estimated 12–34% of women in the US suffer from some form of urinary incontinence [3, 4]. Over 100 surgical methods have been used to treat stress urinary incontinence, including colposuspension, suburethral slings, and newer mid-urethral slings [5]. The Tension-free Vaginal Tape procedure has recently been shown to have a 7-year cure rate of over 80% [6].
Short- and long-term urinary retention are major concerns with any anti-incontinence procedure. While mid-urethral sling procedures are generally performed without major complications, published series report that 23–50% of patients are unable to void immediately after the procedure and are discharged either with a catheter in place or the need to self-catheterize for some period of time after surgery [7–10]. Several studies have identified previous incontinence or prolapse surgery, concomitant pelvic surgery, age, surgeon experience, and peak urinary flow rate on preoperative uroflowmetry as potentially affecting postoperative voiding function [6, 7, 11–13]. However, these studies report the percentage of patients who resumed normal voiding function anywhere from 48 h to 2 weeks after surgery rather than immediately postoperatively. Little has been said about which characteristics will predict that a patient will be discharged without the requirement for an indwelling catheter or self-catheterization after outpatient mid-urethral sling. The prospect of leaving the hospital with a catheter in place or having to perform self-catheterization understandably produces anxiety for many patients. If we can better predict who will be able to void immediately postoperatively, we can more effectively manage patient expectations and concerns. In addition, more precise selection of patients who are likely to benefit from learning self-catheterization would lead to better resource allocation and clinic efficiency. To improve patient satisfaction, it is essential that patients be informed about the minor and major risks of a surgical procedure, including short-term urinary retention. The object of this study was to identify preoperative variables that could be used to predict resumption of adequate voiding function after outpatient, mid-urethral sling.
Materials and methods
At our institution, the Tension-free Vaginal Tape or TVT (vaginal to suprapubic approach) was the mid-urethral sling procedure performed by all three surgeons who participated in this study. We reviewed the medical records of all women who underwent a TVT (Gynecare, a division of Ethicon, Somerville, NJ, USA) procedure at the UMass Memorial Hospital between January 2001 and June 2004. Patients were identified by searching the operating room logs for all procedures performed by the members of the Division of Urogynecology that included a TVT procedure. All TVT procedures for which the patient was discharged on the same day as their surgery (with or without concurrent procedures) were included in the analysis. All patients had a preoperative diagnosis of stress urinary incontinence or mixed urinary incontinence. Patients without urethral hypermobility and patients with intrinsic sphincter deficiency were included.
We excluded all patients who sustained a cystotomy because divisional protocol is to send these patients home with a Foley catheter for 3–5 days without a voiding trial.
Data were compiled from the patients’ clinic and hospital records by a single, unblinded investigator (KIB). Information from each patient’s clinic chart included preoperative history and physical, preoperative urodynamic studies, voiding diary, and postoperative clinic notes. Information from the hospital chart included demographics, operative record and report, anesthesia record, pre- and postoperative nursing records, amount of postoperative narcotics, and discharge instructions.
Preoperatively, each patient underwent testing that included a full history and physical, urine dipstick, and assessment of urethral mobility. Thirty-two percent underwent a simple office filling and 68% had a multichannel urodynamic study. These two groups were demographically similar with the exception of greater age in the group that underwent simple office fillings. A post-void residual volume was determined by catheterization. Urethral hypermobility was defined as a cotton swab excursion of ≥30 degrees of mobility with either cough or Valsalva [14]. Simple office filling was performed with the patient in the supine position. Multichannel urodynamic study was performed using either a Dantec Duet with dual microtip transducer catheter (January 2001–February 2004), or a Laborie Aquarius with dual air-charged transducer catheter system (February 2004–June 2004). Urodynamic studies were performed with the patient in the seated or semi-lithotomy position. The maximum cystometric capacity, maximum urinary flow rate, mean urinary flow rate, time to maximum urinary flow rate, maximum urethral closure pressure, functional urethral length, Valsalva leak point pressure, and presence of detrusor overactivity were the urodynamic variables assessed in this study. The standard bladder volume for the maximum urethral closure pressure, Valsalva leak point pressure, and stress test was 300 ml or cystometric capacity, whichever was smaller [6, 7, 15, 16]. A “normal” Valsalva leak point pressure was defined as leakage at an intra-abdominal pressure >60 cm H2O, and a “normal” maximum urethral closure pressure was defined as >20 cm H2O.
Members of the Division of Urogynecology at the UMass Memorial Hospital performed all procedures. The TVT procedure was performed as previously described [17], with the exception that mesh positioning was not determined by an intra-operative cough stress test. Instead, the mesh was positioned so there was 2–3 mm between the mesh and the mid-urethra. Local with monitored intravenous analgesia (18%), spinal anesthesia (18%), or general anesthesia (64%) was used. The need for catheterization upon discharge was not significantly lower in the spinal group as had been noted by some reports [18]. Regardless of the type of anesthesia, each patient also received approximately 60 ml of 0.25% bupivicaine suprapubically and 3–5 ml periurethrally. Data on the length of the procedure, length of time in the operating room, and estimated blood loss were also collected. The preoperative anxiety score was obtained in the holding area by a nurse asking the patient to rate her own anxiety level on a scale of 1 to 10, with 1 representing minimal anxiety. A holding area anxiety score ≥6 was considered high for the purpose of dichotomizing this variable.
Postoperative bladder function was assessed either by measuring spontaneous urination and post-void residuals or a bladder challenge using retrograde filling of the Foley catheter. This was done within 2–4 h of surgery in the postanesthesia care unit. If a bladder challenge was used, the patient’s bladder was filled with water through a Foley catheter to a volume of at least 200 ml. Then, the catheter was removed, and the patient was asked to void. Regardless of whether spontaneous voiding or bladder challenge was used, patients were considered to have adequate bladder emptying if they were able to void more than 100 ml and had a post-void residual less than 150 ml and less than 50% of the total bladder volume. Patients who did not meet these criteria were considered to have immediate postoperative urinary retention. These patients were discharged with a Foley catheter or with instructions to perform intermittent self-catheterization if they had chosen to learn self-catheterization preoperatively.
Postoperative narcotic use was determined by conversion of medications to oral morphine equivalents utilizing the Narcotics Calculator v1.1 (GlobalRPH; http://www.globalrph.com/narcoticonv.htm). Tramadol was considered equivalent to codeine in potency [19].
Follow-up visits were scheduled at 3 weeks, 6 weeks, 3 months, and 1 year. Patients who were discharged from the hospital with a Foley catheter were seen in the clinic within 4 days for a bladder challenge in addition to the normal follow-up schedule. The clinical outcome with regard to urinary leakage was not the focus of this study; however, patients who reported complete absence of stress incontinence at the last clinic visit were counted as subjectively cured. Patients were counted as improved if they reported a smaller number of stress urinary incontinence events than before surgery regardless of whether they had urge symptoms. Patients who continued to have stress-related urine loss at or near the same level as before surgery were considered treatment failures.
We used SPSS (v12.0) for all statistical analyses. Bivariate analyses were performed utilizing discharge without catheterization (either indwelling or self-catheterization) as the primary outcome measure. We evaluated patient demographic, clinical, and urodynamic variables, as well as perioperative variables, to determine their relationship to the primary outcome. We used Pearson’s chi-square test for categorical variables and Student’s t test for continuous variables, as appropriate, to determine which of the independent variables to include in subsequent logistic regressions. A liberal p value <0.2 was used to identify potential independent predictors and a p value <0.05 was used in the regression analyses to define statistical significance. Most data elements were converted to dichotomous variables for ease of interpretation of the independent variable’s likelihood of impact on the outcome. A backward elimination logistic regression model with age as a continuous variable was used in the final multivariate analysis.
This study was approved by the institutional review board at the University of Massachusetts Medical School. The definitions used in this paper conform to the standards proposed by the International Continence Society unless otherwise noted [20].
Results
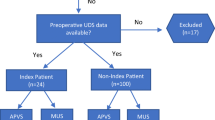
Three hundred and eighty-four procedures that included a mid-urethral sling were performed at the UMass Memorial Hospital between January 1, 2001 and June 30, 2004. Of these, 258 procedures were inpatient, two were misclassified, four were excluded for cystotomy, and 126 patients were discharged on the day of the procedure. Discharge voiding status was available for 94% (119/126) of these eligible patients.
Patient characteristics are listed in Table 1 and perioperative variables in Table 2. One hundred and nine of the 119 patients in the analysis were Caucasian and ten were of Hispanic origin.
Sixty-one percent (73/119) of patients voided without assistance before discharge. Of those who failed to void, 72% (33/46) went home with a Foley catheter and 28% (13/46) went home self-catheterizing. The incidence of urinary retention lasting >14 days was 1.7% (2/119). Subjective success rate at 6–12 weeks was 93% (104/112). Seventy-seven percent (86/112) met criteria for subjective “cure” and 16% (18/112) met criteria for “improved,” as described in the “Materials and methods” section. Two patients (1.7%) required mesh sectioning for long-term urinary retention.
Table 3 reports the results from the bivariate analyses. Surgeon, parity ≥3, anxiety score ≥6 in the holding area, Valsalva leak point pressure >60 cm H2O, maximum urethral closure pressure >20 cm H2O, and functional urethral length >2.4 mm all demonstrated independent associations with discharge without catheterization at a significance level of p<0.2. Menopausal status, detrusor overactivity, incontinence type (stress vs mixed), age greater than the median, preadmission anxiety, body mass index, the performance of concomitant procedures, estimated blood loss, amount of postoperative narcotic use, outcome, PVR, and cystometric capacity did not show a significant association with immediate postoperative voiding function.
Table 4 reports results from the logistic regression analysis. Parity ≥3 (OR 5.1, 95% CI: 1.4–18.9), high holding area anxiety (OR 5.8, 95% CI: 1.5–23.2), and Valsalva leak point pressure >60 cm H2O (OR 7.4, 95% CI: 2.0–27.3) remained independently associated with a successful immediate postoperative voiding trial after controlling for age. In the regression analysis, both Valsalva leak point pressure >60 cm H2O and maximum urethral closure pressure >20 cm H2O were equally strong predictors of immediate resumption of normal voiding, but keeping both variables in the regression model was not superior to using one or the other. Therefore, maximum urethral closure pressure was eliminated from the final model.
Comments
Our results suggest that parity ≥3, Valsalva leak point pressure >60, and higher preoperative anxiety level in the holding area may be associated with a lower likelihood of immediate postoperative urinary retention. The percentage of patients discharged with a need for catheterization (39%) is comparable to other series reported in the literature [7, 8]. Likewise, a comparably small percentage of patients required mesh sectioning for long-term urinary retention (1.7%) [7, 21].
Valsalva leak point pressure is a measure of the integrity of the urinary sphincter when it is exposed to increased intra-abdominal pressure. Urinary leakage at a pressure <60 cm H2O is considered a strong indicator of the presence of intrinsic sphincter deficiency. The presence of intrinsic sphincter deficiency has been implicated as an important factor in TVT success rates [22, 23]. It is possible that the surgeon’s inclination may be to position the sling more tightly in patients who are thought to have intrinsic sphincter deficiency. This tendency could account for the higher likelihood of continued catheterization at discharge in patients with urodynamic evidence of intrinsic sphincter deficiency.
A potential mechanism for the association between higher parity (≥3) and a higher likelihood of successful voiding before discharge is not immediately apparent. Multiparity has been reported to be a risk factor for stress urinary incontinence and other urinary symptoms [24–26]. The mechanism is thought to be related to muscular damage, denervation, and/or damage to the endopelvic fascia [27]. We speculate that women with higher parity may have more mobility of the periurethral connective tissue and therefore could be less prone to obstruction by the sling than women with lower parity.
We were surprised to find that higher anxiety scores before surgery were associated with a decreased need for continued catheterization at discharge. Anxiety is associated with an increase in sympathetic outflow, and micturition is known to be inhibited by increased sympathetic activity and largely initiated through the parasympathetic system. Whether this is a reproducible association will only be answered by future research in this area.
Unlike some previous studies [6, 7, 11–13], we did not find that age, concomitant surgery, previous surgery, or mean urinary flow rate were predictive of immediate postoperative bladder function. Nor did we find any correlation between the type of incontinence (e.g., mixed vs stress incontinence alone) or the amount of postoperative narcotic usage and the likelihood of discharge without requiring catheterization. Similar results have been published in other recent studies [28]. Our series, however, looked only at immediate postoperative retention rates, and only included day procedures.
A potential limitation of this study is that our method for identifying surgical cases (coded operating logs) does not eliminate the possibility of missing cases by fault of incorrect coding. However, based upon our broad inclusion criteria and the ease of identifying those undergoing mid-urethral sling, we do not believe this is a serious limitation.
Inadequate statistical power is another limitation. The total sample size was 119, but only 68% underwent a multichannel urodynamic evaluation. Therefore, the association between Valsalva leak point pressure and the primary outcome is based on a subsample of 81 patients. Additionally, when we evaluated the population of patients who underwent multichannel vs simple office filling, we found a significant difference in age between the two groups. This finding calls into question the lack of significant association between age and postoperative voiding status in our study.
An additional concern is the validity of the Likert scale used to assess holding area anxiety. The reliability of such an instrument, as well as its psychometric properties, is unknown, and must be taken into account when interpreting the association between preoperative anxiety and likelihood of postoperative voiding. Further examination of this issue is necessary before any clinical conclusions can be drawn. In addition, this variable would not be known until the immediate preoperative period and so would have little practical value in terms of counseling patients or choosing those to teach self-catheterization.
In conclusion, urinary retention requiring discharge with either an indwelling catheter or self-catheterization is a medically minor, but troubling situation for a large minority of mid-urethral sling patients. The ability to predict which patients are likely to require catheterization would enable surgeons to better shape patient expectations and determine who would be most likely to benefit from self-catheterization teaching. Higher parity, absence of urodynamic evidence of intrinsic sphincter deficiency, and higher preoperative anxiety score were all independently associated with a lower likelihood of needing continued catheterization at discharge. The next research phase will be to create a “likelihood of postoperative catheterization” score based on preoperative parameters and test its predictive value prospectively in our practice.
References
Hampel C, Artibani W, Espuna Pons M, Haab F, Jackson S, Romero J, Gavart S, Papanicolaou S (2004) Understanding the burden of stress urinary incontinence in Europe: a qualitative review of the literature. Eur Urol 46:15–27
Minaire P, Jacquetin B (1992) The prevalence of female urinary incontinence in general practice. J Gynecol Obstet Biol Reprod (Paris) 21:731–738
Sze EH, Jones WP, Ferguson JL, Barker CD, Dolezal JM (2002) Prevalence of urinary incontinence symptoms among black, white, and hispanic women. Obstet Gynecol 99:572–575
Brown JS, Grady D, Ouslander JG, Herzog AR, Varner RE, Posner SF (1999) Prevalence of urinary incontinence and associated risk factors in postmenopausal women. Heart and estrogen/progestin replacement study (HERS) research group. Obstet Gynecol 94:66–70
Alcalay M, Monga A, Stanton SL (1995) Burch colposuspension: A 10–20 year follow up. Br J Obstet Gynaecol 102:740–745
Nilsson CG, Falconer C, Rezapour M (2004) Seven-year follow-up of the tension-free vaginal tape procedure for treatment of urinary incontinence. Obstet Gynecol 104:1259–1262
Mutone N, Brizendine E, Hale D (2003) Factors that influence voiding function after the tension-free vaginal tape procedure for stress urinary incontinence. Am J Obstet Gynecol 188:1477–1481 (discussion 1481–1473)
Al-Badr A, Ross S, Soroka D, Minassian VA, Karahalios A, Drutz HP (2003) Voiding patterns and urodynamics after a tension-free vaginal tape procedure. J Obstet Gynaecol Can 25:725–730
Minassian VA, Al-Badr A, Drutz HP, Lovatsis D (2004) Tension-free vaginal tape, burch, and slings: are there predictors for early postoperative voiding dysfunction? Int Urogynecol J Pelvic Floor Dysfunct 15:183–187
Mishra VC, Mishra N, Karim OM, Motiwala HG (2005) Voiding dysfunction after tension-free vaginal tape: a conservative approach is often successful. Int Urogynecol J Pelvic Floor Dysfunct 16:210–214 (discussion 214)
Cetinel B, Demirkesen O, Onal B, Akkus E, Alan C, Can G (2004) Are there any factors predicting the cure and complication rates of tension-free vaginal tape? Int Urogynecol J Pelvic Floor Dysfunct 15:188–193
Bodelsson G, Henriksson L, Osser S, Stjernquist M (2002) Short-term complications of the tension-free vaginal tape operation for stress urinary incontinence in women. BJOG 109:566–569
Hong B, Park S, Kim HS, Choo MS (2003) Factors predictive of urinary retention after a tension-free vaginal tape procedure for female stress urinary incontinence. J Urol 170:852–856
Karram MM, Bhatia NN (1988) The q-tip test: standardization of the technique and its interpretation in women with urinary incontinence. Obstet Gynecol 71:807–811
Meschia M, Pifarotti P, Bernasconi F, Guercio E, Maffiolini M, Magatti F, Spreafico L (2001) Tension-free vaginal tape: analysis of outcomes and complications in 404 stress incontinent women. Int Urogynecol J Pelvic Floor Dysfunct 12(Suppl 2):S24–S27
Wang AC, Chen MC (2003) The correlation between preoperative voiding mechanism and surgical outcome of the tension-free vaginal tape procedure, with reference to quality of life. BJU Int 91:502–506
Ulmsten U, Henriksson L, Johnson P, Varhos G (1996) An ambulatory surgical procedure under local anesthesia for treatment of female urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct 7:81–85 (discussion 85–86)
Pavlin DJ, Pavlin EG, Gunn HC, Taraday JK, Koerschgen ME (1999) Voiding in patients with or without ultrasound monitoring of bladder volume after outpatient surgery. Anesth Analg 89:90–97
Gaynes BI, Barkin RL (1999) Analgesics in ophthalmic practice: a review of the oral non-narcotic agent tramadol. Optom Vis Sci 76:455–461
Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, Van Kerrebroeck P, Victor A, Wein A (2003) The standardization of terminology in lower urinary tract function: report from the standardization sub-committee of the international continence society. J Urol 61:37–49
Klutke C, Siegel S, Carlin B, Paszkiewicz E, Kirkemo A, Klutke J (2001) Urinary retention after tension-free vaginal tape procedure: incidence and treatment. J Urol 58:697–701
Paick JS, Ku JH, Shin JW, Son H, Oh SJ, Kim SW (2004) Tension-free vaginal tape procedure for urinary incontinence with low Valsalva leak point pressure. J Urol 172:1370–1373
Nitti VW, Combs AJ (1996) Correlation of Valsalva leak point pressure with subjective degree of stress urinary incontinence in women. J Urol 155:281–285
Grodstein F, Fretts R, Lifford K, Resnick N, Curhan G (2003) Association of age, race, and obstetric history with urinary symptoms among women in the nurses’ health study. Am J Obstet Gynecol 189:428–434
Rortveit G, Hannestad YS, Daltveit AK, Hunskaar S (2001) Age- and type-dependent effects of parity on urinary incontinence: the Norwegian EPINCONT study. Obstet Gynecol 98:1004–1010
Handa VL, Harvey L, Fox HE, Kjerulff KH (2004) Parity and route of delivery: does cesarean delivery reduce bladder symptoms later in life? Am J Obstet Gynecol 191:463–469
Handa VL, Harris TA, Ostergard DR (1996) Protecting the pelvic floor: obstetric management to prevent incontinence and pelvic organ prolapse. Obstet Gynecol 88:470–478
Sokol AI, Jelovsek JE, Walters MD, Paraiso MF, Barber MD (2005) Incidence and predictors of prolonged urinary retention after TVT with and without concurrent prolapse surgery. Am J Obstet Gynecol 192:1537–1543
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Barron, K.I., Savageau, J.A., Young, S.B. et al. Prediction of successful voiding immediately after outpatient mid-urethral sling. Int Urogynecol J 17, 570–575 (2006). https://doi.org/10.1007/s00192-005-0064-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-005-0064-8