Abstract
Purpose
This study aim was to detect the impact of lateral ankle ligaments injury on syndesmotic laxity when evaluated arthroscopically in a cadaveric model. The null hypothesis was that lateral ankle ligament injury does not affect the stability of syndesmosis.
Methods
Sixteen fresh-frozen above-knee amputated cadaveric specimens were divided into two groups of eight specimens that underwent arthroscopic evaluation of the distal tibiofibular joint. In both the groups, the assessment was first done with all syndesmotic and ankle ligaments intact. Thereafter, Group 1 underwent sequential transection of the three lateral ankle ligaments first to identify the effects of lateral ligament injury: (1) anterior talofibular ligament (ATFL), (2) calcaneofibular ligament (CFL), (3) posterior talofibular ligament (PTFL), then followed by the syndesmotic ligaments, (4) AITFL, (5) Interosseous ligament (IOL), and (6) PITFL. Group 2 underwent sequential transection of the (1) AITFL, (2) ATFL, (3) CFL, (4) IOL, (5) PTFL, and (6) PITFL, which represent the most commonly injured pattern in ankle sprain. In all scenarios, four loading conditions were considered under 100 N of direct force: (1) unstressed, (2) a lateral fibular hook test, (3) anterior to posterior (AP) fibular translation test, and (4) posterior to anterior (PA) fibular translation test. Distal tibiofibular coronal plane diastasis at the anterior and posterior third of syndesmosis, as well as AP and PA sagittal plane translation, were arthroscopically measured.
Results
The distal tibiofibular joint remained stable after transection of all lateral ankle ligaments (ATFL, CFL, and PTFL) as well as the AITFL. However, after additional transection of the IOL, the syndesmosis became unstable in both the coronal and sagittal plane. Syndesmosis laxity in the coronal plane was also observed after transection of the ATFL, CFL, AITFL, and IOL. Subsequent transection of the PITFL precipitated syndesmosis laxity in the sagittal plane, as well.
Conclusions
The findings from the present study suggest that lateral ankle ligament injuries itself do not directly affect the stability of syndesmosis. However, if it combines with IOL injuries, even partial injuries cause syndesmotic laxity. As a clinical relevance, accurate diagnosis is the key for surgeons to determine syndesmosis fixation whether there is only AITFL injury or combined IOL injury in concomitant acute syndesmotic and lateral ligament injury.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Injury to the syndesmotic ligaments, including the anteroinferior tibiofibular ligament (AITFL), interosseous ligament (IOL), and posteroinferior tibiofibular ligament (PITFL), occurs in an estimated 18% of all ankle sprains [10, 25, 28]. Severe ankle sprains can combine lateral ligament injuries with syndesmotic injuries, affecting long-term recovery and longer return to sports compared to isolated lateral ankle ligament injuries [19, 35]. Critical to the successful clinical management of syndesmotic injuries, however, is not necessarily the identification of the injury, but rather the effective diagnosis of any resultant laxity of the distal tibiofibular articulation. If left unaddressed, syndesmotic instability can lead to severe residual pain and irreversible osteoarthritic changes [19]. While the diagnosis of syndesmotic laxity is relatively straightforward in the setting of frank distal tibiofibular diastasis, it becomes increasingly difficult in the setting of more subtle laxity [32].
Ankle arthroscopy currently represents the gold standard for diagnosing subtle syndesmotic laxity by virtue of its ability to directly visualize the distal tibiofibular articulation [6, 11, 20, 21, 31, 32]. A previous arthroscopic, cadaveric study by Lubberts et al. found that the syndesmosis is destabilized only after transection of all three syndesmotic ligaments (AITFL, IOL, and PITFL) [15]. On the other hand, partial injuries to the AITFL and IOL can still precipitate syndesmotic laxity if associated with an injury to the deltoid ligaments (DL), [23] presumptively due to the deltoid’s ability to tether the fibula via its attachment through the talus and lateral ankle ligaments. These studies, however, only focused the association between three syndesmosis ligaments and deltoid ligament injury, which in the so-called clinical practice corresponds to pronation-external rotation or pronation-abduction injury. The effect of lateral ankle ligament injury on the stability of syndesmosis has not been investigated.
While the presence of combined lateral ankle and syndesmotic ligamentous injuries is not uncommon, the contribution of the lateral ligaments toward stabilizing the syndesmosis remains unclear. Therefore, this study aim was to detect the impact of lateral ankle ligaments injury on syndesmotic laxity when evaluated arthroscopically. In addition, this result can be an important criterion in deciding how severe ankle ligament injury should be considered to fix syndesmosis as clinical relevance. The null hypothesis was that lateral ankle ligament injury does not affect the stability of syndesmosis.
Materials and methods
This study was approved by the Institutional Review Board of Massachusetts General Hospital (USA), Protocol number, 2016P001295.
Specimen preparation
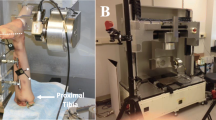
Sixteen nonpaired fresh-frozen, above-knee amputated cadaveric specimens were used, that were purchased from MedCure.inc (RI, USA). The mean age at the time of death was 66 (31–90) years. Thirteen were males and three were females. Specimens were thawed at room temperature 24 h before the start of the experiment. Prior to the experiment, each ankle was evaluated by fluoroscopy (OrthoScan FD Pulse C-Arm, OrthoScan, Scottsdale, AZ). Specimens were excluded if there were any signs of ankle laxity, previous surgeries, fractures, ligamentous injuries, or pre-existing ankle osteoarthritis, and all specimens in this sample were ultimately included. Subsequently, specimens were secured to a wooden board using 5-mm Schanz pins inserted anteroposteriorly into the proximal, middle, and distal aspect of the tibia.
Sequential transection of ligaments
To randomize the intact cadaveric specimen into two groups with equal sample size, a block randomization method was used. None of the raters had been involved in the randomization process. In both groups, arthroscopic assessment (Arthrex, Naples, FL) of the distal tibiofibular joint was performed first with all syndesmotic and ankle ligaments intact and then after a progressive sequence of ligamentous transections. Group 1 underwent sequential transection of the lateral three ankle ligaments first to identify the effects of lateral ligament injury (1) anterior talofibular ligament (ATFL), (2) calcaneofibular ligament (CFL), (3) posterior talofibular ligament (PTFL), followed by the syndesmotic ligaments, (4) AITFL, (5) IOL, and (6) PITFL. Group 2 underwent sequential transection of the (1) AITFL, (2) ATFL, (3) CFL, (4) IOL, (5) PTFL, and (6) PITFL. (Fig. 1) The sequence of ligament transection in Group 2 was based on the most commonly understood progression of injury severity among lateral ankle ligament injuries with associated high ankle sprain [7, 27, 31]. At that time, the ligaments tend to be injured in sequence from the anterolateral to the posterolateral element in the varus ankle position.
Arthroscopic assessment
Arthroscopic evaluation of the distal tibiofibular joint was performed using a 30-degree 2.7-mm arthroscope through standard anterolateral and anteromedial portals. To test laxity of the distal tibiofibular joint at each sequence of ligament transection, stress was applied to the distal fibula using a bone hook. A small incision was made lateral to the fibula 5 cm proximal to the ankle joint, a bone hook was placed around the distal fibular diaphysis, and a 100-N standardized force was applied in the lateral direction to assess coronal and sagittal plane laxity. The 100-N force used in this study was based on a cadaveric study performed by Stoffel et al. who found that forces of more than 100-N did not show a substantial increase in syndesmotic displacement [30]. An electronic force gauge was used to standardize and measure the exact amount of applied force. Halo digital goniometer (Halo Medical Devices, Australia) was used to assure that the applied forces were applied parallel (coronal plane) and perpendicular (sagittal plane) to the ground surface [23].
Coronal plane tibiofibular diastasis was measured at the anterior third of the incisura immediately posterior to the anterior lip, as well as at the posterior third of the incisura immediately anterior to the posterior lip. The measurements were performed using precision-manufactured, spherical arthroscopic probes with diameter increments of 0.2 mm. Displacement in the sagittal plane was assessed by measuring translation of the fibula in both the anterior to posterior (AP) and posterior to anterior (PA) direction relative to the fixed tibia. To do so, a bony mark was made at the center of the intra-articular, medial fibula. An intra-articular probe with a scaled laser mark was used to measure the translation distance between the laser mark and the bony mark with application of a sagittal stress (Fig. 2). Arthroscopic images were captured during the experiment and the precise amount of sagittal translation was measured using imaging software (Image J; NIH 2019). During arthroscopic measurements, the ankle was manually kept in neutral position and was not towed due to a prior study, highlighting that the applied tension on the ankle ligaments, capsular elements, and surrounding soft tissues can mask syndesmotic laxity [16].
Arthroscopic assessment of the syndesmosis in the sagittal plane under a 100 N hook force directed from anterior to posterior (AP) (a, b) or from posterior to anterior (PA) (c, d). The force was measured and standardized using an electronic force gauge and digital goniometer. One-headed arrows represent the direction of force applied. Two-headed arrows represent the distances from the bony landmark at the fibula (Fib) relative to the laser mark at the arthroscopic probe (P) (mm)—before and after applied stress. Fib Fibula, Tib Tibia, P Probe
Two orthopaedic fellowship-trained foot and ankle surgeons performed all arthroscopic probes measurements and sagittal translation measurements with image software independently in two randomly selected specimens to assess interobserver agreement using the intraclass correlation coefficient (ICC) through a two-way mixed-effects model with absolute agreement. The interobserver agreement for the arthroscopic coronal plane translation measurements at the anterior and the posterior third of syndesmosis was thus calculated based on 28 observations, while the interobserver agreement for the arthroscopic AP and PA sagittal plane translation measurements was calculated using 14 observations. Absolute agreement in an ICC assesses how much each measurement performed per observer differs from the other observer. Interpretation of the ICC values was carried out according to the guidelines proposed by Shrout as follows: 0.00–0.10, virtually none; 0.11–0.40, slight; 0.41–0.60, fair; 0.61–0.80, moderate; and 0.81–1.00, substantial [29].
Statistical analysis
Arthroscopic measurements were summarized using means and standard deviations (SD). In each group, Wilcoxon signed-rank test were used to determine differences between the intact stage and the six stages of ligamentous transection. A p value of < 0.05 was considered statistically significant.
With reference to a previous study by Bart Lubberts et al. as the primary outcome, [18] the fibula translational cut off was set to 2 mm for both anterior–posterior and posterior-anterior directions. Then, to achieve 80% statistical power with an overall two-tailed Type-1 rate of 2.5%, the moderate effect of ligamentous transection (partial eta-squared = 0.03), and met sphericity assumption (Nonsphericity correction E = 1) for one-way repeated analysis of variance. It was detected that eight specimens were needed in each group. The sample size calculation was performed using G*Power Version 3.1.9.4. All analyses were performed using Stata 14.2 (StataCorp LP, College Station, TX).
Results
In Group 1, compared to the intact ligamentous stage, the distal tibiofibular joint remained stable in both the coronal and sagittal plane after transection of all the lateral ankle ligaments (ATFL, CFL, and PTFL) and the AITFL. However, after additional transection of the IOL, the syndesmosis became unstable in both the coronal and sagittal planes. Coronal plane diastasis increased at both the anterior and posterior third of the incisura (p < 0.001 both), as well as with both AP and PA translation of the fibula in the sagittal plane (p < 0.001 both (Table 1). This laxity worsened further with subsequent transection of the PITFL.
In Group 2, the syndesmosis remained stable in the coronal plane after transection of the AITFL, ATFL, and CFL. However, after additional transection of the IOL, the syndesmosis similarly became unstable in both the coronal plane sagittal planes. Coronal plane diastasis increased at both the anterior and posterior third of the incisura (p < 0.001 and p < 0.001, respectively), as well as with both AP and PA translation of the fibula in the sagittal plane (p = 0.008 and p = 0.028, respectively) (Table 2). This laxity worsened further with subsequent transection of the PITFL.
The interobserver reliability for the arthroscopic coronal plane translation measurement at the anterior (0.99; 95% confidence interval [CI] 0.95–1.0) and the posterior third of syndesmosis (0.97; 95% CI 0.84–0.99) were substantial. The interobserver reliability for the AP and PA sagittal translation measurements was substantial, as well (0.86; 95% CI 0.79–0.92 and 0.85; 95% CI 0.73–0.92, respectively).
Discussion
This study highlights that, under arthroscopic assessment, the lateral ankle ligaments injury indirectly contributes to syndesmotic stability if the damage extends to the IOL injury. In other words, stable partial syndesmotic ligamentous injuries can be rendered unstable if the lateral ankle ligaments are also injured. As stated anatomically, a high ankle sprain with injury to the AITFL and IOL that would otherwise have been stable can be destabilized if the ATFL and CFL are also ruptured.
This result has taken a great step in prior studies, which have highlighted the association between lateral ankle sprains and high ankle sprains. The concomitant presence of both injuries did not hitherto delineate whether the lateral ankle ligaments actually contribute to syndesmotic stability, or whether both may simply be impacted by the same injury mechanism [7, 24, 27, 33].
The critical role of the syndesmosis toward maintaining the ankle mortise is empirically highlighted by numerous studies demonstrating the significant morbidity associated with leaving syndesmotic instability unaddressed [6, 26, 34]. In turn, the need for the talus to be bracketed by the fibula laterally and tibia medially intuits the need to preserve the distal tibiofibular relationship, historically understood to be maintained by the syndesmotic ligaments that directly bind the fibula to the tibia. In the same manner that walls of a house may be bound to each other not only by the roof but also through the foundation, the fibula and tibia are bound together not only through the syndesmotic ligaments above the ankle joint but also through their respective attachments to the talus below. The lateral ankle ligaments and the multiple components of the deltoid ligament therefore directly contribute toward maintaining the distal tibiofibular relationship by virtue of bridging their respective bony origins to the same bone—the talus. Thus, partial syndesmotic injuries to the AITFL and IOL that have been shown to be stable in isolation may not predicate that the intact PITFL alone can stabilize the syndesmosis, but rather that the residual attachment of the fibula to the tibia through the talus can continue to prevent abnormal motion at the distal tibiofibular articulation. In such scenarios, additional injury to the deltoid ligament has been shown to destabilize the syndesmosis [23]. This study highlights that the mirrored scenario is also true. Concomitant lateral ankle ligament injury can also destabilize otherwise stable syndesmotic injuries.
It is critical to differentiate injury patterns from mechanisms of injury. Calder et al. found that athletes with AITFL ruptures who also had a deltoid injury were 11-fold more likely to have an unstable syndesmosis than when injuring the AITFL alone, and that lateral ligament injury to the ATFL was actually protective, making it less likely that the syndesmosis was destabilized [5]. Part of this is structural, wherein the deltoid has been shown to contribute to syndesmotic stability as discussed above. But overwhelmingly this likely relates to mechanism of injury, wherein external rotation injuries are not only effective at injuring the syndesmosis, but also at tearing the multiple components of the deltoid ligament. Inversion injuries are highly effective at tearing the lateral ankle ligaments but much less effective at tearing the syndesmotic ligaments to the point of instability. On the other hand, this does not predicate that the lateral ankle ligaments do not contribute to syndesmotic stability, simply that the injury mechanism is less effective at destabilizing the distal tibiofibular articulation. When an inversion moment is severe enough, so that the AITFL and IOL are torn, alongside the ATFL and CFL, this study highlights that the distal tibiofibular joint is indeed rendered unstable.
From a practical point of view, how much fibular motion at the distal tibiofibular articulation should a clinician consider to be abnormal under arthroscopic stress examination? Prior studies have highlighted that approximately 3 mm of coronal plane diastasis and a total of 2 mm of total AP and PA sagittal plane motion can be considered reasonable thresholds for diagnosing syndesmotic laxity [12, 13, 17]. The practicality of these thresholds is heightened by the fact that while the precision tools used to conduct measurements in this study are not readily available in the operating room, 2 mm and 3 mm probes are standard to many instrumentation kits. The values measured in this study and displayed in Tables 1 and 2 corroborate these threshold values.
There are some limitations to this study. First, this study evaluated the translation of the fibula in the coronal and sagittal directions as the laxity of syndesmosis, but not in fibula rotation. Markus et al. demonstrated that an unstable AITFL should be repaired and augmented, as it represents an important stabilizer of external rotation of the distal fibula [22]. Given those ligament injuries of the ankle generally occur from the anterolateral side in clinical situation, fibula laxity in the external rotation can occur in the early stages of ligament injury, compared to the appearance of coronal and sagittal laxity. Second, the diagnosis of syndesmotic laxity was a statistical one, wherein laxity was judged to be present when distal tibiofibular motion after ligamentous transection was significantly greater than the intact state. It remains to be seen whether the threshold values discussed directly translate into clinical significance. Third, there may be variation in normal distal tibiofibular motion between individuals. Juan et al. demonstrated that measuring parameters indicating syndesmosis alignment should be compared to the contralateral ankle [14]. While arthroscopy allows direct evaluation of the distal tibiofibular relationship, it is invasive and does not allow a contralateral comparison in vivo. In a cadaveric model, one benefits from being able to examine the intact state and thereafter create the injury via controlled ligamentous transections. In the clinical setting, threshold values are useful, but a contralateral comparison arguably serves as a better internal control. Therefore, noninvasive, dynamic studies such as weight bearing CT with volumetric measurements of the distal tibiofibular space [1,2,3, 8, 9] or bedside ultrasound may better overcome some of these challenges [13]. Additional studies are necessary to better delineate their role.
Conclusions
The findings from the present study underscore that syndesmosis is not directly destabilized by injury to the lateral ankle ligaments. However, when combined with IOL injuries, syndesmosis can be destabilized. As a clinical relevance, clinicians must be aware the combination of IOL injury is the key to make clinicians consider the fixation of syndesmosis.
References
Ashkani Esfahani S, Bhimani R, Lubberts B, Kerkhoffs GM, Waryasz G, DiGiovanni CW et al (2022) Volume measurements on weightbearing computed tomography can detect subtle syndesmotic instability. J Orthop Res 40(2):460–467
Bhimani R, Ashkani-Esfanhani S, Lubberts B, Daniel G, Hgemeijer NC, Waryasz G et al (2020) Utility of volumetric measurement via weight-bearing computed tomography scan to diagnose syndesmotic instability. Foot and Ankle Int 41(7):859–865
Bhimani R, Ashkani-Esfanhani S, Lubberts B, Kaiser P, Kerkhoffs GMMG, Waryasz G et al (2022) Utility of WBCT to diagnose syndesmotic instability in patients with Weber B lateral malleolar fractures. J Am Acad Orthop Surg 30(3):423–433
Brown KW, Morrison WB, Schweizer ME, Parellada JA, Nothnagel H (2004) MRI findings associated with distal tibiofibular syndesmosis injury. Am J Roentgenol 182(1):131–136
Calder JD, Bamford R, Petrie A, McCollum GA (2016) Stable versus unstable grade II high ankle sprains: a prospective study predicting the need for surgical stabilization and time to return to sports. Arthroscopy 32(4):634–642
Candal-Couto JJ, Burrow D, Bromage S, Briggs PJ (2004) Instability of the tibiofibular syndesmosis: Have we been pulling in the wrong direction? Injury 35(8):814–818
Chun KY, Choi YS, Lee SH, Kim JS, Young KW, Jeong MS et al (2015) Deltoid ligament and tibiofibular syndesmosis injury in chronic lateral ankle instability: magnetic resonance imaging evaluation at 3t and comparison with arthroscopy. Korean J Radiol 16(5):1096–1103
Daniel G, Olivia L, AshkaniEsfahani S, Bhimani R, Waryasz G, Gino K et al (2022) Automated volume measurement of the syndesmosis using 3D weightbearing CT. Foot Ankle Orthop. 7(1):2473011421S00031
Del Rio A, Bewsher SM, Roshan-Zamir S, Tate J, Eden M, Gotmaker R et al (2020) Weightbearing cone-beam computed tomography of acute ankle syndesmosis injuries. J Foot Ankle Surg 59(2):258–263
Dubin JC, Comeau D, McClelland RI, Dubin RA, Ferrel E (2011) Lateral and syndesmotic ankle sprain injuries: a narrative literature review. J Chiropr Med 10(3):204–219
Feller R, Borenstein T, Fantry AJ, Kellum RB, Machan JT, Nickisch F et al (2017) Arthroscopic quantification of syndesmotic instability in a cadaveric model. Arthroscopy 33(2):436–444
Hagemeijer NC, Elghazy MA, Waryasz G, Guss D, DiGiovanni CW, Kerkhoffs GMMJ (2020) Arthroscopic coronal plane syndesmotic instability has been over-diagnosed. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-020-06067-5
Hagemeijer NC, Saengsin J, Chang SH, Waryasz GR, Kerkhoffs GM, Guss D et al (2020) Diagnosing syndesmotic instability with dynamic ultrasound—establishing the natural variations in normal motion. Injury 51(11):2703–2709
Juan CV, Mercedes VM, Ahmed EG, Sergio T (2021) Analysis of the uninjured tibiofibular syndesmosis using conventional CT-imaging and axial force in different foot positions. Foot Ankle Surg S1268–7731(21):00169–00177
Lubberts B, Guss D, Vopat BG, Johnson AH, van Dijk CN, Lee H et al (2018) The arthroscopic syndesmotic assessment tool can differentiate between stable and unstable ankle syndesmoses. Knee Surg Sports Traumatol Arthrosc 28(1):193–201
Lubberts B, Guss D, Vopat BG, Wolf JC, Moon DK, DiGiovanni CW (2017) The effect of ankle distraction on arthroscopic evaluation of syndesmotic instability: a cadaveric study. Clin Biomech 50:16–20
Lubberts B, Massri-Pugin J, Guss D, Wolf JC, Bhimani R, Waryasz GR et al (2020) Arthroscopic assessment of syndesmotic instability in the sagittal plane in a cadaveric model. Foot Ankle Int 41(2):237–243
Lubberts B, Massri-Pugin J, Guss D, Wolf JC, Bhimani R, Waryasz GR et al (2019) Arthroscopic assessment of syndesmotic instability in the sagittal plane in a cadaveric model. Foot Ankle Int 41(2):237–243
Lubberts B, van Dijk PA, Donovan N, van Dijk CN (2016) Stable and unstable grade II syndesmotic injuries require different treatment strategies and vary in functional outcomes: a systematic review. J ISAKOS 1:192–197
Lucas DE, Watson BC, Simpson GA, Berlet GC, Hyer CF (2016) Arthroscopic evaluation of syndesmotic instability and malreduction. Foot Ankle Spec 9(6):500–505
Lui TH, Ip K, Chow HT (2005) Comparison of radiologic and arthroscopic diagnoses of distal tibiofibular syndesmosis disruption in acute ankle fracture. Arthroscopy 21(11):1370
Markus R, Gordon M, Owen N, Wolfgang B, Christian E (2022) Evidence-based surgical treatment algorithm for unstable syndesmotic injuries. J Clin Med 11(2):331
Massri-Pugin J, Lubberts B, Vopat BG, Wolf JC, DiGiovanni CW, Guss D (2018) Role of the deltoid ligament in syndesmotic instability. Foot Ankle Int 39(5):598–603
Miller JR, Dunn KW, Ciliberti LJ, Eldridge SW, Reed LD (2017) Diagnostic value of early magnetic resonance imaging after acute lateral ankle injury. J Foot Ankle Surg 56(6):1143–1146
Osbahr DC, Drakos MC, O’Loughlin PF, Lyman S, Barnes R, Kennedy JG et al (2013) Syndesmosis and lateral ankle sprains in the National football league. Orthopedics 36(11):1378–1384
Ramsey P (1976) Changes in tibiotalar area of contact caused by lateral talar shift. J Bone Joint Surg 58(3):356–357
Roemer FW, Jomaah N, Niu J, Almusa E, Roger B, D’Hooghe P et al (2014) Ligamentous injuries and the risk of associated tissue damage in acute ankle sprains in athletes: a cross-sectional MRI study. Am J Sports Med 42(7):1549–1557
Shawen SB, Dworak T, Anderson RB (2016) Return to play following ankle sprain and lateral ligament reconstruction. Clin Sports Med 35(4):697–709
Shrout PE (1998) Measurement reliability and agreement in psychiatry. Stat Methods Med Res 7(3):301–317
Stoffel K, Wysocki D, Baddour E, Nicholls R, Yates P (2009) Comparison of two intraoperative assessment methods for injuries to the ankle syndesmosis: a cadaveric study. J Bone Jt Surg - Ser A 91(11):2646–2652
Takao M, Ochi M, Naito K, Iwata A, Kawasaki K, Tobita M et al (2001) Arthroscopic diagnosis of tibiofibular syndesmosis disruption. Arthroscopy 17(8):836–843
Tourné Y, Molinier F, Andrieu M, Porta J, Barbier G (2019) Diagnosis and treatment of tibiofibular syndesmosis lesions. Orthop Traumatol Surg Res 105(8S):S275–S286
Uys HD, Rijke AM (2002) Clinical association of acute lateral ankle sprain with syndesmotic involvement: a stress radiography and magnetic resonance imaging study. Am J Sports Med 30(6):816–822
Wagener ML, Beumer A, Swierstra BA (2011) Chronic instability of the anterior tibiofibular syndesmosis of the ankle. Arthroscopic findings and results of anatomical reconstruction. BMC Musculoskelet Disord 27(12):212
Williams GN, Jones MH, Amendola A (2007) Syndesmotic ankle sprains in athletes. Am J Sports Med 35(7):1197–1207
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: this study was supported by a grant from the Arthroscopy Association of North America (grant 2017D009573). In addition, the author(s) received research support from Arthrex Inc.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author(s) report grants from the Arthroscopy Association of North America, during the conduct of the study. ICMJE forms for all authors are available online.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sato, G., Saengsin, J., Bhimani, R. et al. Isolated injuries to the lateral ankle ligaments have no direct effect on syndesmotic stability. Knee Surg Sports Traumatol Arthrosc 30, 3881–3887 (2022). https://doi.org/10.1007/s00167-022-06985-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-022-06985-6