Abstract
Purpose
There remains a lack of consensus on the patient factors associated with graft rupture following anterior cruciate ligament (ACL) reconstruction. This study aimed to identify the rate of revision and surgeon-reported graft rupture and clarify the patient risk factors for failure.
Methods
Analysis was conducted on prospective data captured by the New Zealand ACL registry. All primary isolated ACL reconstructions recorded between April 2014 and December 2018 were reviewed to identify the rate of revision and surgeon-reported graft rupture. Univariate and multivariate survival analysis was performed to identify patient factors associated with revision and graft rupture.
Results
A total of 7402 primary isolated ACL reconstructions were reviewed and had a mean follow-up time of 23.1 (SD ± 13.9) months. There were 258 surgeon-reported graft ruptures (3.5%) of which 175 patients underwent subsequent revision ACL reconstruction (2.4%). Patients younger than 18 years had the highest risk of revision (adjusted HR = 7.29, p < 0.001) and graft rupture (adjusted HR = 4.26, p < 0.001) when compared to patients aged over 36 years. Male patients had a higher risk of revision (adjusted HR = 2.00, p < 0.001) and graft rupture (adjusted HR = 1.70, p < 0.001) when compared to their female counterparts. Patients who underwent ACL reconstruction within 6 months of their injury had a two times increased risk of revision compared to patients who had surgery after 12 months (adjusted HR = 2.15, p = 0.016).
Conclusion
Younger age, male sex and a shorter injury-to-surgery time interval increased the risk of revision, while younger age and male sex increased the risk of surgeon-reported graft rupture.
Level of evidence
II.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Rupture of the anterior cruciate ligament (ACL) is a common knee injury and is frequently managed with surgical reconstruction [1,2,3,4,5]. However, graft failure remains a major complication following ACL reconstruction, resulting in significant patient disability and economic cost. Various patient factors including age, gender, activity at the time of injury and concomitant injuries have been associated with repeat injury, but a lack of consensus remains [6,7,8,9,10,11]. Clarifying characteristics which may predispose patients to treatment failure may guide surgical and rehabilitation practice to prevent poor outcomes following ACL reconstruction.
The New Zealand ACL registry was recently implemented in 2014 following the success of the national and community ACL registries in Scandinavia, the United States, the United Kingdom and Luxembourg. In comparison to traditional cohort studies and randomised controlled trials, registry studies allow for large population-specific analysis and cross-country comparisons where different patient demographics and surgical practice are observed [12,13,14].
Revision ACL reconstruction is a common primary outcome that is used to measure failure following primary ACL reconstruction as it is well defined and captured in a registry design. However, revision reconstruction underestimates the true rate of graft rupture as not all patients proceed to have a revision. As a result, current registry studies have reported difficulty with defining the true rate of failure associated with ACL reconstruction [15,16,17,18,19,20]. The New Zealand ACL registry is the only nation-wide registry to capture graft ruptures that are reported by surgeons following post-operative patient follow-up. This provides an alternative outcome measure that attempts to capture the true rate of treatment failure.
The aim of this study was to analyse prospective data captured by the New Zealand ACL registry to identify both the rates of ACL revision and surgeon-reported graft rupture, and the patient factors that increase the risk of treatment failure.
Materials and methods
A prospective cohort study was performed using data extracted from the New Zealand ACL registry. 7612 primary ACL reconstructions have been recorded by the registry since its inception in April 2014–December 2018. Patients undergoing multi-ligament reconstruction or any concurrent surgery such as osteotomy or unicompartmental knee replacement were excluded (N = 146). Only the patient’s first primary isolated ACL reconstruction recorded in the registry was eligible for analysis (N = 7402) and was followed up until either a revision or surgeon-reported graft rupture was recorded, or to the end of the study period.
The New Zealand ACL Registry
The New Zealand ACL registry is a nation-wide registry that began in 2014 and prospectively captures patient, surgical and follow-up data. Since 2017, it is mandatory for all orthopaedic surgeons who perform ACL reconstructions to actively participate in the registry to achieve re-certification [21]. All patients recorded in the registry have signed consent forms to participate. In addition, this analysis has been approved by the Health and Disability Ethics Committee (HDEC) as an audit activity. As of 2018, based on comparisons to government healthcare data, it is estimated that approximately 85% of all ACL reconstructions performed in New Zealand are captured by the registry [22]. Patient demographic data are collected through a pre-operative form. An operative data form detailing each reconstruction procedure is completed by the surgeon. In addition, surgeons can fill out a post-operative complication form that details any early and late complications relating to the procedure. Patient-reported complications are confirmed with the treating surgeon.
Outcome of interest and predictor variables
The primary outcome for this study was revision ACL reconstruction as recorded in the registry during the study period (April 2014–December 2018). The secondary outcome measure was surgeon-reported graft rupture as captured by the registry’s post-operative complication form. Surgeon-reported graft rupture was defined as a patient who re-presented to the orthopaedic clinic for follow-up and was deemed to have sustained a graft rupture following clinical assessment and examination documenting knee laxity, with confirmation of graft injury on radiological imaging. Patients were included in this group regardless of whether they eventually proceeded to have a revision.
The predictor variables of interest included all patient demographic factors that are recorded by the registry using both a patient questionnaire that is completed prior to the operation and an intra-operative data form that is filled out by the surgeon. Variables analysed from the patient questionnaire included patient sex, age and activity at the time of injury. The activity at the time of injury was subcategorised into sporting versus non-sporting injuries, which included ACL injuries sustained during work, traffic or other non-sporting activities. Surgeon-reported variables analysed from the intra-operative data form included injury side, time from injury-to-surgery, previous history of surgery on the index knee, and the presence of meniscal and/or cartilage injury.
Statistical analyses
All statistical analyses were performed using IBM SPSS Statistics version 25 and results were considered statistically significant at p < 0.05. Age and injury-to-surgery time were analysed as both categorical and continuous variables following normality assessment with Q–Q plots and histograms. Kaplan–Meier survival analysis was performed to calculate the cumulative probability of graft survival following primary ACL reconstruction. Univariate analysis of categorical variables was performed via Chi-square test or Fisher’s exact test, while continuous variables were analysed via Student’s t tests. In addition, incidence densities per 100 observed person-years were calculated. Statistically significant factors on univariate analysis were entered into a multivariate Cox proportional hazards regression model to produce hazard ratios (HR) with 95% confidence intervals (CI). The validity and robustness of the subsequent model was checked against forward and backward stepwise models. The assumption of proportional hazards was assessed via log(− log) plots.
Results
7402 primary isolated ACL reconstructions were performed during the study period (April 2014–December 2018) (Table 1). The mean time of follow-up was 23.1 (SD ± 13.9) months. The mean age of patients was 29.1 (SD ± 10.9) years. The median time from injury-to-surgery was 4.2 (IQR = 5.2) months. Fifty-eight percent of the patients were male. 50% of reconstructions were performed on the patient’s right knee. Twenty-eight percent of patients had a concomitant meniscal injury reported by the surgeon. Fifty-seven percent of patients had a concomitant cartilage injury reported by the surgeon. Eighty-two percent of reconstructions were caused by a sporting injury.
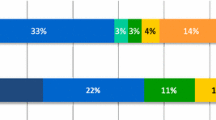
175 revision ACL reconstructions were performed out of 7402 primary isolated ACL reconstructions producing an overall revision rate of 2.4% over the study period. The number of revisions per 100 observed person-years was 1.3 (Table 1). The number at risk at 2 years was 3453 patients and the cumulative survival probability was 97.3% (95% CI, 96.8–97.7) (Fig. 1).
A total of 258 graft ruptures were reported by surgeons using the post-operative complication form producing a rate of 3.5%. As a result, there were 83 patients who had a graft rupture that did not proceed to have a revision (32.2%). The number of reported ruptures per 100 observed person-years was 1.9 (Table 1).
3558 patients had a minimum follow-up duration of 2 years. In these patients, the 2-year revision rate was 3.0% (N = 106). The 2-year surgeon-reported graft rupture rate was 4.4% (N = 157).
Revision ACL reconstruction
On univariate analysis, patient sex, age, time to surgery, concomitant cartilage injury and cause of injury (sporting vs non-sporting) had a statistically significant association with the rate of revision ACL reconstruction (Table 2). Injury side, history of previous surgery on the index knee and concomitant meniscal injury were not associated.
On multivariate analysis, patient sex, age and time from injury-to-surgery were statistically significant risk factors for revision ACL reconstruction (Table 3). Male patients were two times more at risk of revision than female patients (HR = 2.00; 95% CI, 1.42–2.81; p < 0.001). Patients aged less than 18 years were the most at-risk age bracket with a seven times higher risk of revision compared to patients older than 36 years (HR = 7.29; 95% CI, 3.66–14.53; p < 0.001). Furthermore, patients aged 19–36 years also had a higher risk of revision compared to patients in the oldest age bracket (HR = 4.08; 95% CI, 2.05–8.15; p < 0.001, HR = 3.25; 95% CI, 1.60–6.61; p = 0.001 and HR = 2.32; 95% CI, 1.04–5.18; p = 0.04). Patients who underwent reconstruction within 6 months were two times more likely to undergo revision compared to patients who underwent delayed reconstruction 1 year from the initial injury date (HR = 2.15; 95% CI, 1.16–4.00; p = 0.016).
Concomitant cartilage injury and cause of injury (sporting versus non-sporting) were not risk factors for revision.
Surgeon-reported graft rupture
On univariate analysis, patient sex, age, concomitant cartilage injury and cause of injury (sporting versus non-sporting) had a statistically significant association with the rate of surgeon-reported graft rupture (Table 2). Injury side, time to surgery, previous history of surgery, concomitant meniscal injury were not associated.
On multivariate analysis, patient sex and age were statistically significant risk factors for surgeon-reported graft rupture (Table 3). Male patients had a 1.70 times higher risk of graft rupture compared to females (95% CI, 1.30–2.23; p < 0.001). All patients aged 36 years or younger had a higher risk of graft rupture compared to patients aged 37 or older. The highest risk of graft rupture was observed in patients younger than 18 years (HR = 4.26; 95% CI, 2.62–6.95; p < 0.001). There was no difference in the risk of graft rupture between sporting injuries and non-sporting injuries (n.s.).
Discussion
The most important finding of the present study was that patient age, sex and time from injury-to-surgery were associated with a higher risk of ACL revision, while age and sex were significant predictors for graft rupture.
Younger age has been a commonly reported risk factor for ACL revision [23,24,25,26,27,28,29,30]. In comparison to patients older than 36 years, we found patients aged less than 18 years had a seven times higher risk of revision ACL reconstruction (HR = 7.3). Amongst registry studies from the United States, Sweden and Norway, this is the highest reported risk of revision for the youngest age category in comparison to the oldest age category, however, different age brackets are reported by each registry [15, 16, 26, 31, 32]. Furthermore, patients aged 19–24, 25–30 and 31–36 had a 4.1, 3.3 and 2.3 times higher revision risk. The association between younger age and an increased risk of revision may be explained by various reasons. First, younger patients are more likely to return to high-contact pivoting sports which increases the risk of graft rupture [29, 30, 33,34,35,36]. Second, older patients may be less likely to undergo revision as they are more tolerant of reduced knee stability due to lower activity demands [32, 37]. Finally, younger patients may be under higher sporting expectations to return to sport following an ACL tear, and do so at an earlier stage in their recovery [38]. There may also be anatomical, biomechanical and neuromuscular factors that predispose them to injury at a younger age, which in turn may predispose them to reinjury [39].
This study demonstrated that male patients were two times more likely than females to undergo revision ACL reconstruction. This is comparable to a study by Maletis et al. who found a 1.4 times higher risk of revision in males in the Kaiser Permanente ACL registry [40]. The higher risk of revision observed in male patients may be explained by their tendency to return to sport earlier than females. Webster et al. investigated the return to sport following ACL reconstruction in 1440 patients and reported that males younger than 26 years had a 1.7 times higher odds of returning to sport within 1 year post-reconstruction compared to their female counterparts (p < 0.001), while males aged 26–35 years had 2.6 times higher odds of an early return to sport compared to females (p < 0.001) [35]. An earlier and higher rate of return to sport can be correlated to a higher risk of revision [30]. Despite these findings, the Scandinavian registries and a meta-analysis by Tan et al. did not find an association between patient gender and the risk of ACL revision [17, 23, 32, 41]. The lack of consensus between studies may be explained by different patient demographics, rates of return to sport and potentially different levels of participation in different high-risk sports, especially between males and females. Regardless, the conflicting results reported between countries demonstrate the benefits of implementing a nation-wide registry that can provide population-specific data and direct feedback to hospitals and surgeons.
A shorter injury-to-surgery time interval was associated with an increased risk of revision. This finding is comparable to Fältström et al. from the Swedish ACL registry who demonstrated that patients who underwent ACL reconstruction within 90 days of the initial ACL rupture were three times more likely to have a revision compared to patients who had surgery after 1 year from the initial injury (HR = 3.07, p < 0.001) [16]. Similarly, patients who had a reconstruction within 6 months of the initial ACL rupture had a two times higher risk of revision compared to patients who underwent primary reconstruction 1 year after the initial rupture (HR = 2.15, p = 0.016). It is possible this reflects a shorter time available for appropriate prehabilitation, however, it is more likely that higher level athletes who are more likely to return to play (and risk subsequent re-rupture) are also more likely to proceed to earlier surgical intervention following the initial ACL injury.
The New Zealand ACL registry is the only national registry that allows surgeons to report graft ruptures that require revision following appropriate clinical and radiological examinations. Using this method, 258 graft ruptures that were deemed to require revision (3.5%) were reported, with only 175 of these patients proceeding to undergo a revision ACL reconstruction. A similar rate of graft rupture has been reported by Kaeding et al. who analysed the multicentre orthopaedic outcomes network (MOON) cohort and reported a re-tear rate of 4.4% in 2684 patients after 2 years of follow-up [24]. We found patient age and gender were statistically significant risk factors for surgeon-reported graft rupture. Patients aged less than 18 years were 4.26 times more likely to have a graft rupture compared to patients aged over 36 years (p < 0.001). Furthermore, patients aged 19–36 years were between 3.1 and 1.8 times more likely to have a graft rupture (p < 0.001, p = 0.034). In addition, males had a 1.7 times higher risk of graft rupture compared to females (p < 0.001). No other patient variables influenced the risk of surgeon-reported graft rupture. The rate of patients with a reported graft rupture proceeding to subsequent revision was higher with younger age (Fig. 2). Eighty-five percent of patients younger than 18 years who had a graft rupture proceeded to have a revision. In contrast, 43% of patients aged over 36 years who had a graft rupture proceeded to have a revision.
As the New Zealand ACL registry began in 2014, this study represents early follow-up following ACL reconstruction only. To adjust for differences in follow-up duration, the rate of revision and graft rupture was calculated per 100 observed person-years and a Cox regression survival analysis was performed. Furthermore, our findings were consistent when multivariate analysis was performed on only patients with a minimum follow-up of 2 years (Appendix 1).
Although revision ACL reconstruction is a well-defined primary endpoint, it is likely to underestimate the true rate of graft rupture. To mitigate against this, we investigated the rate of surgeon-reported graft rupture as captured by the registry. These data are a strength of this study and are a unique feature of the New Zealand ACL registry that is not utilised by any other national or community ligament registry. However, this process relies on patients re-presenting to the orthopaedic follow-up clinic and, therefore, not all graft ruptures would be recorded.
The registry does not currently record patients lost to emigration or death, therefore, there is a potential for bias in our analysis. However, we expect this number to be low and to not differ greatly between the patient populations compared. Additionally, large observational studies such as this are useful in identifying associations, however, they do not provide evidence of causation.
These findings allow clinicians to identify patients who may be more at-risk of reinjury following primary ACL reconstruction. Clinicians should be aware of the higher rate of reinjury in younger patients, male patients and those with a shorter time from injury-to-surgery, especially when making rehabilitative decisions such as return-to-activity.
Conclusion
The rate of revision was 2.4% and the rate of surgeon-reported graft rupture was 3.5% in 7402 primary isolated ACL reconstructions. Younger age, male sex and a shorter injury-to-surgery time interval are risk factors for revision ACL reconstruction, while younger age and male sex increased the risk of a graft rupture proceeding to revision surgery.
References
Giugliano DN, Solomon JL (2007) ACL tears in female athletes. Phys Med Rehabil Clin N Am 18:417–438
Griffin LY, Agel J, Albohm MJ, Arendt EA, Dick RW, Garrett WE et al (2000) Noncontact anterior cruciate ligament injuries: risk factors and prevention strategies. J Am Acad Orthop Surg 8:141–150
Lyman S, Koulouvaris P, Sherman S, Do H, Mandl LA, Marx RG (2009) Epidemiology of anterior cruciate ligament reconstruction. Trends, readmissions, and subsequent knee surgery. J Bone Joint Surg 91:2321–2328
Mall NA, Chalmers PN, Moric M, Tanaka MJ, Cole BJ, Bach BR et al (2014) Incidence and trends of anterior cruciate ligament reconstruction in the United States. Am J Sports Med 42:2363–2370
Sanders TL, Maradit Kremers H, Bryan AJ, Larson DR, Dahm DL, Levy BA et al (2016) Incidence of anterior cruciate ligament tears and reconstruction: a 21-year population-based study. Am J Sports Med 44:1502–1507
Gifstad T, Foss OA, Engebretsen L, Lind M, Forssblad M, Albrektsen G et al (2014) Lower risk of revision with patellar tendon autografts compared with hamstring autografts: a registry study based on 45,998 primary ACL reconstructions in Scandinavia. Am J Sports Med 42:2319–2328
Ponce BA, Cain EL, Pflugner R, Fleisig GS, Young BL, Boohaker HA et al (2016) Risk factors for revision anterior cruciate ligament reconstruction. J Knee Surg 29:329–336
Salmon LJ, Refshauge KM, Russell VJ, Roe JP, Linklater J, Pinczewski LA (2006) Gender differences in outcome after anterior cruciate ligament reconstruction with hamstring tendon autograft. Am J Sports Med 34:621–629
Schlumberger M, Schuster P, Schulz M, Immendörfer M, Mayer P, Bartholomä J et al (2017) Traumatic graft rupture after primary and revision anterior cruciate ligament reconstruction: retrospective analysis of incidence and risk factors in 2915 cases. Knee Surg Sports Traumatol Arthrosc 25:1535–1541
Stevenson H, Jennifer Webster B, Robert Johnson B, Beynnon B, Beynnon BD (1998) Gender differences in knee injury epidemiology among competitive alpine ski racers. Iowa Orthop J 18:64–66
Yabroudi M, Björnsson H, Lynch A, Muller B, Samuelsson K, Tarabichi M et al (2016) Predictors of revision surgery after anterior cruciate ligament reconstruction. Am J Sports Med 4:1–7
Benjamin B, Magnussen RA, Abraham GT, Mamman KG (2013) ACL reconstruction registry in Brunei Darussalam: a comparison with European and North American cohorts. Eur Orthop Traumatol 4:173–176
Magnussen RA, Trojani C, Granan LP, Neyret P, Colombet P, Engebretsen L et al (2015) Patient demographics and surgical characteristics in ACL revision: a comparison of French, Norwegian, and North American cohorts. Knee Surg Sports Traumatol Arthrosc 23:2339–2348
Svantesson E, Hamrin Senorski E, Baldari A, Ayeni OR, Engebretsen L, Franceschi F et al (2018) Factors associated with additional anterior cruciate ligament reconstruction and register comparison: a systematic review on the Scandinavian knee ligament registers. Br J Sports Med 53:418–425
Andernord D, Desai N, Björnsson H, Ylander M, Karlsson J, Samuelsson K (2015) Patient predictors of early revision surgery after anterior cruciate ligament reconstruction: a cohort study of 16,930 patients with 2-year follow-up. Am J Sports Med 43:121–127
Fältström A, Hägglund M, Magnusson H, Forssblad M, Kvist J (2016) Predictors for additional anterior cruciate ligament reconstruction: data from the Swedish national ACL register. Knee Surg Sports Traumatol Arthrosc 24:885–894
Lind M, Menhert F, Pedersen AB (2012) Incidence and outcome after revision anterior cruciate ligament reconstruction: results from the Danish registry for knee ligament reconstructions. Am J Sports Med 40:1551–1557
Maletis GB, Chen J, Inacio MCS, Love RM, Funahashi TT (2017) Increased risk of revision after anterior cruciate ligament reconstruction with soft tissue allografts compared with autografts: graft processing and time make a difference. Am J Sports Med 45:1837–1844
Spragg L, Chen J, Mirzayan R, Love R, Maletis G (2016) The effect of autologous hamstring graft diameter on the likelihood for revision of anterior cruciate ligament reconstruction. Am J Sports Med 44:1475–1481
Svantesson E, Sundemo D, Hamrin Senorski E, Alentorn-Geli E, Musahl V, Fu FH et al (2017) Double-bundle anterior cruciate ligament reconstruction is superior to single-bundle reconstruction in terms of revision frequency: a study of 22,460 patients from the Swedish National Knee Ligament Register. Knee Surg Sports Traumatol Arthrosc 25:3884–3891
New Zealand ACL registry annual report 2017. https://www.aclregistry.nz/reports/. Accessed 1 Nov 2019
New Zealand ACL registry annual report 2018. https://www.aclregistry.nz/reports/. Accessed 1 Nov 2019
Faunø P, Rahr-Wagner L, Lind M (2014) Risk for revision after anterior cruciate ligament reconstruction is higher among adolescents: results from the Danish registry of knee ligament reconstruction. Orthop J Sport Med. https://doi.org/10.1177/2325967114552405
Kaeding CC, Pedroza AD, Reinke EK, Huston LJ, Spindler KP (2015) Risk factors and predictors of subsequent ACL injury in either knee after ACL reconstruction: Prospective analysis of 2488 primary ACL reconstructions from the MOON cohort. Am J Sports Med 43:1583–1590
Magnussen RA, Lawrence JTR, West RL, Toth AP, Taylor DC, Garrett WE (2012) Graft size and patient age are predictors of early revision after anterior cruciate ligament reconstruction with hamstring autograft. Arthroscopy 28:526–531
Maletis GB, Chen J, Inacio MCS, Funahashi TT (2016) Age-related risk factors for revision anterior cruciate ligament reconstruction: a cohort study of 21,304 patients from the Kaiser Permanente anterior cruciate ligament registry. Am J Sports Med 44:331–336
Maletis GB, Inacio MCS, Desmond JL, Funahashi TT (2013) Reconstruction of the anterior cruciate ligament: association of graft choice with increased risk of early revision. Bone Joint J 95:623–628
Wasserstein D, Khoshbin A, Dwyer T, Chahal J, Gandhi R, Mahomed N et al (2013) Risk factors for recurrent anterior cruciate ligament reconstruction: a population study in Ontario, Canada, with 5-year follow-up. Am J Sports Med 41:2099–2107
Webster KE, Feller JA, Leigh WB, Richmond AK (2014) Younger patients are at increased risk for graft rupture and contralateral injury after anterior cruciate ligament reconstruction. Am J Sports Med 42:641–647
Wiggins AJ, Grandhi RK, Schneider DK, Stanfield D, Webster KE, Myer GD (2016) Risk of secondary injury in younger athletes after anterior cruciate ligament reconstruction. Am J Sports Med 44:1861–1876
Desai N, Andernord D, Sundemo D, Alentorn-Geli E, Musahl V, Fu F et al (2017) Revision surgery in anterior cruciate ligament reconstruction: a cohort study of 17,682 patients from the Swedish National Knee Ligament Register. Knee Surg Sports Traumatol Arthrosc 25:1542–1554
Persson A, Fjeldsgaard K, Gjertsen JE, Kjellsen AB, Engebretsen L, Hole RM et al (2014) Increased risk of revision with hamstring tendon grafts compared with patellar tendon grafts after anterior cruciate ligament reconstruction: a study of 12,643 patients from the Norwegian Cruciate Ligament Registry, 2004–2012. Am J Sports Med 42:285–291
Edwards PK, Ebert JR, Joss B, Ackland T, Annear P, Buelow JU et al (2018) Patient characteristics and predictors of return to sport at 12 months after anterior cruciate ligament reconstruction: the importance of patient age and postoperative rehabilitation. Orthop J Sport Med. https://doi.org/10.1177/2325967118797575
Paterno MV, Rauh MJ, Schmitt LC, Ford KR, Hewett TE (2012) Incidence of contralateral and ipsilateral anterior cruciate ligament (ACL) injury after primary ACL reconstruction and return to sport. Clin J Sport Med 22:116–121
Webster KE, Feller JA (2018) Return to level I sports after anterior cruciate ligament reconstruction: evaluation of age, sex, and readiness to return criteria. Orthop J Sport Med. https://doi.org/10.1177/2325967118788045
Webster KE, Feller JA, Whitehead TS, Myer GD, Merory PB (2017) Return to sport in the younger patient with anterior cruciate ligament reconstruction. Orthop J Sport Med 5:1–4
Marx RG, Stump TJ, Jones EC, Wickiewicz TL, Warren RF (2001) Development and evaluation of an activity rating scale for disorders of the knee. Am J Sports Med 29:213–218
De Valk EJ, Moen MH, Winters M, Bakker EWP, Tamminga R, Van Der Hoeven H (2013) Preoperative patient and injury factors of successful rehabilitation after anterior cruciate ligament reconstruction with single-bundle techniques. Arthroscopy 29:1879–1895
Smith HC, Vacek P, Johnson RJ, Slauterbeck JR, Hashemi J, Shultz S et al (2012) Risk factors for anterior cruciate ligament injury: a review of the literature-part 1: neuromuscular and anatomic risk. Sports Health 4:69–78
Maletis GB, Inacio MCS, Funahashi TT (2015) Risk factors associated with revision and contralateral anterior cruciate ligament reconstructions in the Kaiser Permanente ACLR registry. Am J Sports Med 43:641–647
Tan SHS, Lau BPH, Khin LW, Lingaraj K (2016) The importance of patient sex in the outcomes of anterior cruciate ligament reconstructions. Am J Sports Med 44:242–254
Acknowledgements
The authors would like to acknowledge Charlotte Smith from the New Zealand ACL registry for her ongoing support and assistance with data administration. RR would to like to acknowledge the Maurice and Phyllis Paykel Trust for providing student support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
We, the authors, declare that we have no conflicts of interest with relation to this study. MGC reports that he does consulting for Johnson & Johnson, receives fellowship funding from Johnson & Johnson and Arthrex, and receives royalties from Arthrex, none of which are related to this study.
Funding
There is no funding source.
Ethical approval
Health and Disability Ethics Committee approval as an audit activity.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Rights and permissions
About this article
Cite this article
Rahardja, R., Zhu, M., Love, H. et al. Rates of revision and surgeon-reported graft rupture following ACL reconstruction: early results from the New Zealand ACL Registry. Knee Surg Sports Traumatol Arthrosc 28, 2194–2202 (2020). https://doi.org/10.1007/s00167-019-05773-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-019-05773-z