Abstract
Purpose
This study aimed to clarify the natural knee kinematics provided by bicruciate-retaining total knee arthroplasty (BCR-TKA) compared with those of unicompartmental knee arthroplasty (UKA) and normal knees.
Methods
Volunteers and patients who had undergone UKA and BCR-TKA with anatomical articular surface performed squatting motion under fluoroscopy. To estimate the knee’s spatial position and orientation, a two-dimensional/three-dimensional registration technique was used. The rotation angle and anteroposterior translation of the medial and lateral sides of the femur relative to the tibia in each flexion angle were directly evaluated using the same local coordinate system and their differences amongst the three groups were analysed using two-way analysis of variance and Bonferroni post hoc pairwise comparison.
Results
From 0° to 10° of flexion, the femoral external rotation angle of BCR-TKA knees was significantly greater than that of normal and UKA knees and the medial side of BCR-TKA knees was significantly more anteriorly located than that of normal and UKA knees. From 40° to 50° of flexion, the medial side of UKA knees was significantly more posteriorly located than that of normal and BCR-TKA knees. From 30° to 120° of flexion, the lateral side of BCR-TKA knees was significantly more anteriorly located than that of normal and UKA knees.
Conclusion
The in vivo kinematics of BCR-TKA knees reproduces those of normal knees to a lower extent than those of UKA knees. Thus, BCR-TKA with anatomical articular surface reproduces in vivo kinematics of normal knees to a lower extent than UKA.
Level of evidence
III.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Total knee arthroplasty (TKA) is one of the most effective orthopaedic procedures for pain relief and functional restoration in osteoarthritic knees. Recently, the indication has been extended from the elderly to younger, more active patients [23]. However, several studies have reported that approximately 20% of patients who undergo TKA remain unsatisfied [26, 27]. This dissatisfaction may be explained by abnormal kinematics due to sacrificing of the anterior cruciate ligament (ACL) [33].
Consequently, bicruciate-retaining TKA (BCR-TKA) was developed in the 1960s by Gunston, who created the polycentric knee [11], which was modified into the geometric knee in the 1970s by Cracchiolo et al. [5]. In addition, Cloutier improved the BCR design and reported 82% survival of up to 22 years [31]. Similarly, Pritchett reported 89% survival of up to 23 years [30]. In addition, some studies reported that BCR-TKA could recreate normal knee kinematics by preserving the ACL and posterior cruciate ligament (PCL) [12, 33]. The BCR-TKA with an anatomical articular surface has a medial concave and lateral convex articular design. The concept of this design provides guidance for axial rotation and posterior translation that are similar to those of normal knees. Zumbrunn et al. performed dynamic computer simulations of BCR-TKA with an anatomical articular surface using a medial concave and lateral convex and reported that the kinematics of the knees such as anteroposterior (AP) translation was similar to that of normal knees [39]. Therefore, knees that underwent BCR-TKA with an anatomical articular surface are expected to show in vivo kinematics that are similar to those of normal knees. However, no study has compared BCR-TKA with an anatomical articular surface with another implant or with normal knees.
Furthermore, several studies have reported that patient satisfaction with unicompartmental knee arthroplasty (UKA) is better than that with TKA [22, 36]. This suggests that preservation of the ACL and lateral compartment results in a good clinical outcome. Moreover, some studies demonstrated that knee kinematics after UKA also replicated normal knee kinematics in the axial rotation, AP translation, and kinematic pathway [15, 29].
Therefore, it is meaningful to evaluate which ACL-preserving arthroplasty has kinematics that are more similar to those of normal knees in terms of clinical outcomes. However, no study directly comparing the kinematics amongst BCR-TKA, UKA, and normal knees has been conducted, possibly because their local coordinate systems (LCSs) are different.
In Asian and Middle-Eastern countries, people bend their knees deeply in activities of daily living such as gardening, using the restroom, and exercising; hence, many patients who underwent arthroplasty desire deep knee bend (DKB). Therefore, it is important to evaluate the DKB activities.
This study aimed to determine whether in vivo kinematic difference amongst BCR-TKA, UKA, and normal knees exists using the same LCS during DKB activities. The hypothesis of this study was that there were differences amongst BCR-TKA, UKA, and normal knees.
Materials and methods
Sixteen knees from eight volunteers, 21 knees from 20 patients who had UKA (Oxford partial knee, Zimmer Biomet G.K., Warsaw, USA) to treat anteromedial osteoarthritis (OA) with intact ACL, and 17 knees from 15 patients who had BCR-TKA (Journey II XR, Smith & Nephew, Memphis, TN, USA) to treat bicompartmental or tricompartmental OA with intact ACL were examined. Twenty-one BCR-TKAs were performed using the same surgical technique by 3 knee surgeons. A senior surgeon (H.I.) participated in all the procedures as either the chief surgeon or the first assistant. Those patients with postoperative 2011 Knee Society Score (KSS 2011) functional activities score > 30 were examined. Patients with severe valgus whose preoperative hip-knee-ankle (HKA) angle was > 185° were excluded. All the volunteers and patients were Japanese and provided written informed consent to participate in this study. Institutional review board approval was obtained, with documentation. Survival of the ACL was confirmed using magnetic resonance imaging. Characteristics of the volunteers and patients are presented in Table 1. The mean preoperative range of motion examined by a goniometer and the mean duration of postoperative follow-up at the time of fluoroscopic analysis in UKA and BCR-TKA knees and the mean HKA angle of UKA and BCR-TKA knees before surgery and at the time of analysis are shown in Table 2. Furthermore, Table 3 shows KSS 2011 of BCR-TKA and UKA knees at the time of analysis. The postoperative AP stability was evaluated using a KT 2000 arthrometer (MEDmetric, San Diego, CA, USA) with a 134-N anterior force applied to the proximal tibia at a 30° flexion angle. The measurement was performed twice and the average values were used. The AP translations of UKA and BCR-TKA knees measured using a KT 2000 arthrometer at 30° flexion angle were 6.8 ± 2.6 and 5.6 ± 1.0 mm, respectively.
Under fluoroscopy, each participant performed a squatting motion at a natural pace as a DKB activity (Online Video 1). The squatting motion was recorded once after practising several times. The patient’s fluoroscopic surveillance was performed > 6 and < 18 months after surgery. The sequential motion was recorded as a series of digital X-ray images (1024 × 1024 × 12 bits/pixel, 7.5-Hz serial spot images as a DICOM file) using a 17-inch (43-cm) flat panel detector system (C-vision Safire L, Shimadzu, Kyoto, Japan and ZEXIRA DREX-ZX80, Toshiba, Tokyo, Japan). Furthermore, all images were processed by dynamic range compression, thereby enabling edge-enhanced images. To estimate the spatial position and orientation of the knee automatically, a two-dimensional/three-dimensional (2D/3D) registration technique [37], based on a contour-based registration algorithm using single-view fluoroscopic images and 3D computer-aided design (CAD) models, was employed. The estimation accuracy of relative motion between metal components was ≤ 0.5° in rotation and ≤ 0.4 mm in translation [37].
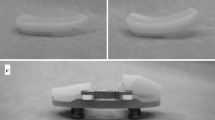
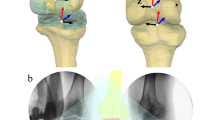
Moreover, to compare BCR-TKA, UKA, and normal knees using the same LCS, 3D bone models were created from computed tomography (CT) and used for the CAD models. The imaging interval of CT was 1 mm. The 3D bone model of UKA and BCR-TKA knees were created from preoperative CT. In BCR-TKA knees, bony contour creation was difficult because of an artefact. Thus, 2D/3D registration of femoral and tibial implants was performed initially; subsequently, 2D/3D registration of femoral and tibial bone models was performed. The relative position between the implant and the bone was matched using surface registration [3] between preoperative 3D models, the 3D bone models were created from preoperative CT, and 3D models created from postoperative CT (Figs. 1 and 2, Online Video 2). Estimation accuracy for the relative motion between the 3D bone models was ≤ 1° in rotation and ≤ 1 mm in translation [21]. The implant’s rotational alignment relative to bone was evaluated using postoperative CT according to previous studies [17, 18]. The rotational femoral component angle was defined as the angle between the line of the anterior cutting surface and the surgical epicondylar axis. The rotational tibial component angle was defined as the angle between the line perpendicular to the line of the medial and lateral parts of the most posterior tibia and the AP line of tibial tray. Both mean femoral components were externally rotated (UKA: 2.1° ± 3.2°; BCR-TKA: 1.0° ± 2.6°). Additionally, both mean tibial components were externally rotated (UKA: 3.6° ± 4.8°; BCR-TKA: 5.3° ± 5.5°).
The LCS at the bone model was produced according to a previous study [21]. Regarding the LCS for the femur, the z-axis passes through the hip centre and the centre of the line connecting the medial sulcus and lateral condyle. The surgical epicondylar axis was projected onto the plane perpendicular to the z-axis. That projection was established as the x-axis. The line perpendicular to both the x- and z-axes was established as the y-axis. Regarding the LCS for the tibia, the z-axis passes through the centre of the medial and the lateral eminences and the ankle centre. The x-axis runs parallel to the line of the medial and lateral parts of the most posterior tibia. The line perpendicular to both the x- and z-axes was established as the y-axis. Knee rotations were described using the joint rotational convention of Grood and Suntay [10]. The flexion angle during fluoroscopy, femoral rotation angle relative to the tibia, AP translation of the medial sulcus (medial side), and lateral epicondyle (lateral side) of the femur on the plane perpendicular to the tibial mechanical axis, and kinematic pathway in each flexion angle were evaluated [21]. In patients who could not extend to 0°, external rotation was calculated at the maximum extension angle. AP translation was calculated as a percentage relative to the proximal AP dimension of the tibia [21]. Flexion was denoted as positive, and extension as negative. External rotation was denoted as positive and internal rotation as negative. Positive and negative values of AP translation were described as anterior and posterior to the axis of the tibia, respectively. All the values were expressed as mean ± standard deviation.
Statistical analyses
Results were analysed using SPSS version 25 (IBM Corp., Armonk, NY, USA). One-way analysis of variance (ANOVA) and post hoc pairwise comparison (Bonferroni test) were used to analyse the volunteer/patient characteristics and the flexion angle of the three groups. Two-way ANOVA and post hoc pairwise comparison (Bonferroni test) were used to analyse the differences in rotation angle and AP translation amongst the three groups. Mann–Whitney U test was employed to analyse the preoperative range of motion, postoperative follow-up, HKA angle, and KSS 2011 of the UKA and BCR-TKA knees. A p value < 0.05 was considered statistically significant. Moreover, a power analysis using EZR [19] indicated that 12 knees would be required for an alpha set at 0.05, power at 0.8, and effect size at 0.25.
Results
Flexion angle during fluoroscopy
Normal knees were gradually flexed from − 4.8° ± 3.5° to 148.8° ± 6.5°; UKA knees, from 4.0° ± 6.5° to 134.5° ± 12.4°; and BCR-TKA knees, from − 4.1° ± 4.4° to 117.9° ± 13.1°. The extension angle of UKA knees was significantly smaller than that of normal and BCR-TKA knees (p < 0.01), whereas the maximum flexion angle of BCR-TKA knees was significantly smaller than that of normal and UKA knees (p < 0.01). In addition, the maximum flexion angle of UKA knees was significantly smaller than that of normal knees (p < 0.01).
Rotation angle
The femurs of the three groups displayed external rotation relative to the tibia with flexion. From 0° to 10° of flexion, the femoral external rotation angle of BCR-TKA knees was significantly greater than that of normal and UKA knees (Fig. 3).
Rotation angle during squatting motion. The markers indicate the femoral external rotation relative to the tibia. *Significant differences between normal knees and bicruciate-retaining total knee arthroplasty (BCR-TKA) knees (p < 0.05). †Significant differences between unicompartmental knee arthroplasty (UKA) and BCR-TKA knees (p < 0.05)
AP translation
In normal knees, the AP translation of the medial side of the femur indicated 15.5% ± 8.3% anterior movement from 0° to 50° of flexion. Flexion > 50° indicated 15.1% ± 7.1% posterior movement. Moreover, AP translation of the medial side of the femur in UKA and BCR-TKA knees indicated mild posterior movement with flexion (UKA knees, 10.3% ± 9.0%; BCR-TKA knees, 13.5% ± 10.1%). From 0° to 10° of flexion, the medial side of BCR-TKA knees was significantly more anteriorly located than that of normal and UKA knees. From 40° to 50° of flexion, the medial side of UKA knees was significantly more posteriorly located than that of normal and BCR-TKA knees (Fig. 4).
Anteroposterior (AP) translation of the femoral medial sulcus during squatting motion. *Significant differences between normal and bicruciate-retaining total knee arthroplasty (BCR-TKA) knees (p < 0.05). †Significant differences between unicompartmental knee arthroplasty (UKA) and BCR-TKA knees (p < 0.05). §Significant differences between normal and UKA knees (p < 0.05)
In all groups, the AP translation of the lateral side of the femur indicated posterior movement with flexion (normal knees, 48.3% ± 17.8%; UKA knees, 39.4% ± 17.0%; BCR-TKA knees, 23.2% ± 11.5%). From 30° to 120° of flexion, the lateral side of BCR-TKA knees was significantly more anteriorly located than that of normal and UKA knees (Fig. 5).
Anteroposterior (AP) translation of the femoral lateral epicondyle during squatting motion. *Significant differences between normal and bicruciate-retaining total knee arthroplasty (BCR-TKA) knees (p < 0.05). †Significant differences between unicompartmental knee arthroplasty (UKA) and BCR-TKA knees (p < 0.05)
Kinematic pathway
In normal knees, the difference between the medial and lateral sides of the femur reflected a medial pivot pattern followed by a bicondylar rollback. In UKA and BCR-TKA knees, a medial pivot pattern with flexion was observed (Fig. 6).
Kinematic pathway during squatting motion. a Normal knee. b Unicompartmental knee arthroplasty (UKA) knee. c Bicruciate-retaining total knee arthroplasty (BCR-TKA) knee. Blue and orange arrows indicate the direction of the movement. In normal knees, a medial pivot pattern was observed from 0° to 50° of flexion. Beyond 50°, a bicondylar rollback was observed. In UKA and BCR-TKA knees, a medial pivot pattern with flexion was observed
Discussion
The most important finding was that BCR-TKA knees reproduce the in vivo kinematics of normal knees to a lower extent than UKA knees under the same LCS, which suggests that preservation of the lateral compartment is vital during weight-bearing activity.
This is the first study to directly evaluate the in vivo knee kinematics of normal volunteers and patients who had UKA and BCR-TKA during high-flexion activities of daily living using the CAD model of fluoroscopically captured images with the same LCS. In addition, this is the first study to compare Journey II XR BCR-TKA with another implant and with normal knees. Several studies have compared the in vivo kinematics between normal knees and knees after arthroplasty [2, 7, 9]. However, most studies compared the kinematics using different LCSs [7, 9]. Arauz et al. compared the kinematics using the same LCS; however, the operated bone model was created from a mirror image of the non-operated side [2]. Thus, the operated bone shape may not be well represented. In our study, the LCS was united by registration of preoperative and postoperative models. Hence, a comparison of the absolute values of each group was possible.
Regarding the rotation angle, all groups displayed femoral external rotation relative to the tibia with flexion. However, in BCR-TKA knees, a larger external rotation angle was observed from extension to early flexion. Moreover, the femoral external rotation angle was smaller in BCR-TKA knees than in normal and UKA knees. Generally, normal knees during squatting show steep external rotation in early flexion, which is called screw-home movement [13, 25]. Screw-home movement is facilitated by both the ACL and the articular surface of normal knees and is the rotation that occurs between the tibia and femur [8]. Several studies reported that after ACL-sacrificed TKA, knees do not show screw-home movement similar to that of normal knees [7, 9, 20]. In addition, BCR-TKA with a symmetrical articular surface showed incomplete replication of the screw-home mechanism [1]. The results of this study suggest that despite the preservation of the ACL and anatomical asymmetrical articular design, normal knee kinematics after TKA are difficult to achieve. The articular surface of this BCR-TKA implant might be insufficient to recreate that of normal knees. Additionally, the replacement of the lateral compartment might influence the stiffness of the lateral side. Moreover, the femoral external rotation angle of severe OA knees during high-flexion activities was smaller than that of normal knees due to increased collateral stiffness and other soft tissue contractures [14]. Therefore, preoperative collateral stiffness and other soft tissue contractures may also affect postoperative kinematics of knees after BCR-TKA. In addition, soft tissue release may become one of the meaningful procedures to achieve a normal kinematic pattern after TKA regarding the contracture knees. On the other hand, regarding no contracture knees, it may be important to maintain normal alignment. Although it is difficult to compare directly due to the difference of the LCS, previous studies that evaluated the in vivo kinematics of posterior-stabilised TKA (PS-TKA) knees and cruciate-retaining TKA (CR-TKA) knees reported that a total of 5° to 10° of femoral external rotation with flexion was observed [16, 32, 34]. In the current study, the amount of femoral external rotation was < 5°. These suggest that BCR-TKA knees might be more restrictive than PS-TKA and CR-TKA. No significant difference in femoral external rotation between UKA and normal knees was found. Mochizuki et al. reported that the kinematics of fixed-bearing (FB) UKA is not similar to that of normal knees [24]. These findings suggest that mobile-bearing (MB) UKA, such as Oxford partial knee, may achieve more similar rotation kinematics to that of normal knees compared with FB UKA.
Regarding the AP translation, the medial side of UKA knees was located more posterior than that of normal and BCR-TKA knees. This suggests that the medial side of UKA knees could easily slide posteriorly during weight-bearing activities. In addition, MB UKA has low conformity between the meniscal bearing and the tibial articular surface due to the flat-on-flat design, which may in turn influence the posterior slide during weight-bearing activities. On the other hand, with regard to the lateral side, that of BCR-TKA knees was significantly more anteriorly located than that of normal and UKA knees from early flexion to high flexion. Arauz et al. reported that AP translation of the lateral contact point of BCR-TKA with symmetrical articular surface is lower than that of normal knees due to the articular surface design of the tibial liner, that is, the absence of a convex lateral tibial plateau [1]. However, the result of our study suggests that AP translation of the lateral side of BCR-TKA knees with anatomical articular surface is also lower than that of normal knees. Okada et al. reported that the tibial baseplate is often placed anteriorly to preserve the ACL insertion area and that higher ACL tension results in femoral-anterior location in the full extension range [28]. These could in turn affect the AP kinematics after BCR-TKA. Moreover, no significant difference between lateral AP translation of normal knees and that of UKA knees was observed. Therefore, lateral compartment replacement, including removal of the meniscus, or preoperative OA condition, such as collateral stiffness and soft tissue contractures, may affect lateral AP translation. Previous studies have reported that PS-TKA knees showed more posterior translation with flexion than cruciate-retaining TKA CR-TKA knees during DKB activities [6, 38]. Therefore, the kinematics of PS-TKA knees may more closely resemble those of normal knees.
Kinematic pathways in this study, such as a medial pivot pattern, were observed in UKA, BCR-TKA, and normal knees. This suggests that ACL and PCL preservation may be associated with normal-like kinematics. However, some differences from normal knees were noted. In normal knees, posterior femoral rollback was observed from mid- to high-flexion, whereas in UKA and BCR-TKA knees, posterior femoral rollback was not observed. In this study, the medial side of UKA knees was located posteriorly. Therefore, it might be difficult to move posterior from mid- to high flexion. In addition, Okada et al. demonstrated that the in situ ACL forces of knees that underwent BCR-TKA are greater than those of intact knees [28]. In addition, Tsai et al. reported overstretching of the PCL in BCR-TKA knees [35]. Higher ACL tension after BCR-TKA may prevent posterior femoral rollback.
In vivo kinematics of BCR-TKA knees was less similar to that of normal knees than that of UKA knees, except the medial AP translation. However, the patient-reported outcome (PRO), such as KSS 2011, was not significantly different between BCR-TKA and UKA knees. These suggest that the in vivo kinematic pattern is not be related to the PRO. In addition, PRO after arthroplasty is influenced by preoperative conditions [4]. Hence, an evaluation of the change rate between preoperation and postoperation is needed in future investigations.
This study has some limitations. First, this study analysed knee joint kinematics only after surgery and did not take the preoperative knee kinematics into consideration. Preoperative kinematics could influence postoperative range of motion. Second, this study analysed patients whose pain and KSS 2011 symptom scores were great; this was due to the difficulty of patients with high pain and low KSS 2011 scores performing squatting. Third, the mean duration of postoperative follow-up between UKA and BCR-TKA knees was different. In addition, the follow-up duration of BCR-TKA knees was comparatively short. Therefore, the kinematics might be different during long-term follow-up. However, as the difference in the current study was < 3 months, this limitation is considered to have little clinical significance. Fourth, only knees that underwent mobile-bearing UKA and BCR-TKA with anatomical articular surface were analysed in the current study; hence, results of this study might not be generalized to other types of UKA and BCR-TKA or to other types of TKA such as PS-TKA and CR-TKA. Fifth, the characteristics, such as the sex and age, of volunteers and patients were quite different in this study; matching patients to reduce these differences would have been desirable. Sixth, the AP stability of volunteer was not evaluated using a KT2000 arthrometer. Therefore, the AP translation of volunteers might not be suitable as normal.
Using the same LCS, it was determined that BCR-TKA reproduced the in vivo kinematics of normal knees to a lower extent than UKA. Therefore, BCR-TKA knees may have lower clinical outcomes than those of UKA. However, the PRO was not significantly different between BCR-TKA and UKA. Regarding BCR-TKA with anatomical articular surface, the in vivo kinematic pattern may not be related to the clinical outcomes.
Conclusion
Although BCR-TKA knees reproduced the in vivo kinematics of normal knees to a lower extent than UKA knees, there was no difference in the reported clinical outcome scores.
Abbreviations
- KSS 2011:
-
2011 Knee Society Score
- 2D:
-
Two-dimensional
- 3D:
-
Three-dimensional
- ACL:
-
Anterior cruciate ligament
- ANOVA:
-
Analysis of variance
- AP:
-
Anteroposterior
- BCR-TKA:
-
Bicruciate-retaining total knee arthroplasty
- CAD:
-
Computer-aided design
- CR:
-
Cruciate-retaining
- CR-TKA:
-
Cruciate-retaining total knee arthroplasty
- CT:
-
Computed tomography
- DKB:
-
Deep knee bend
- FB:
-
Fixed bearing
- HKA:
-
Hip-knee-ankle
- KSS:
-
Knee Society Score
- LCS:
-
Local coordinate system
- MB:
-
Mobile-bearing
- OA:
-
Osteoarthritis
- PCL:
-
Posterior cruciate ligament
- PRO:
-
Patient-reported outcome
- PS:
-
Posterior-stabilised
- PS-TKA:
-
Posterior-stabilised total knee arthroplasty
- SD:
-
Standard deviation
- TKA:
-
Total knee arthroplasty
- UKA:
-
Unicompartmental knee arthroplasty
References
Arauz P, Klemt C, Limmahakhun S, An S, Kwon YM (2018) Stair climbing and high knee flexion activities in bi-cruciate retaining total knee arthroplasty: in vivo kinematics and articular contact analysis. J Arthroplasty 34:570–576
Arauz P, Peng Y, Kwon YM (2018) Knee motion symmetry was not restored in patients with unilateral bi-cruciate retaining total knee arthroplasty-in vivo three-dimensional kinematic analysis. Int Orthop 42:2817–2823
Audette MA, Ferrie FP, Peters TM (2000) An algorithmic overview of surface registration techniques for medical imaging. Med Image Anal 4:201–217
Bourne RB, Chesworth BM, Davis AM, Mahomed NN, Charron KD (2010) Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res 468:57–63
Cracchiolo A 3rd, Benson M, Finerman GA, Horacek K, Amstutz HC (1979) A prospective comparative clinical analysis of the first-generation knee replacements: polycentric vs. geometric knee arthroplasty. Clin Orthop Relat Res 145:37–46
Dennis DA, Komistek RD, Colwell CE Jr., Ranawat CS, Scott RD, Thornhill TS et al (1998) In vivo anteroposterior femorotibial translation of total knee arthroplasty: a multicenter analysis. Clin Orthop Relat Res 356:47–57
Dennis DA, Komistek RD, Mahfouz MR, Walker SA, Tucker A (2004) A multicenter analysis of axial femorotibial rotation after total knee arthroplasty. Clin Orthop Relat Res 428:180–189
Fuss FK (1992) Principles and mechanisms of automatic rotation during terminal extension in the human knee joint. J Anat 180(Pt 2):297–304
Grieco TF, Sharma A, Dessinger GM, Cates HE, Komistek RD (2017) In vivo kinematic comparison of a bicruciate stabilized total knee arthroplasty and the normal knee using fluoroscopy. J Arthroplasty 33:565–571
Grood ES, Suntay WJ (1983) A joint coordinate system for the clinical description of three-dimensional motions: application to the knee. J Biomech Eng 105:136–144
Gunston FH (1971) Polycentric knee arthroplasty. Prosthetic simulation of normal knee movement. J Bone Jt Surg Br 53:272–277
Halewood C, Traynor A, Bellemans J, Victor J, Amis AA (2015) Anteroposterior laxity after bicruciate-retaining total knee arthroplasty is closer to the native knee than ACL-resecting TKA: a biomechanical cadaver study. J Arthroplasty 30:2315–2319
Hallen LG, Lindahl O (1966) The “screw-home” movement in the knee-joint. Acta Orthop Scand 37:97–106
Hamai S, Moro-oka TA, Miura H, Shimoto T, Higaki H, Fregly BJ et al (2009) Knee kinematics in medial osteoarthritis during in vivo weight-bearing activities. J Orthop Res 27:1555–1561
Heyse TJ, El-Zayat BF, De Corte R, Chevalier Y, Scheys L, Innocenti B et al (2014) UKA closely preserves natural knee kinematics in vitro. Knee Surg Sports Traumatol Arthrosc 22:1902–1910
Horiuchi H, Akizuki S, Tomita T, Sugamoto K, Yamazaki T, Shimizu N (2012) In vivo kinematic analysis of cruciate-retaining total knee arthroplasty during weight-bearing and non–weight-bearing deep knee bending. J Arthroplasty 27:1196–1202
Inui H, Taketomi S, Nakamura K, Sanada T, Tanaka S, Nakagawa T (2013) An additional reference axis improves femoral rotation alignment in image-free computer navigation assisted total knee arthroplasty. J Arthroplasty 28:766–771
Inui H, Taketomi S, Nakamura K, Takei S, Takeda H, Tanaka S et al (2013) Influence of navigation system updates on total knee arthroplasty. BMC Sports Sci Med Rehabil 5:10
Kanda Y (2013) Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant 48:452–458
Kono K, Inui H, Tomita T, Yamazaki T, Taketomi S, Sugamoto K et al (2019) Bicruciate-stabilised total knee arthroplasty provides good functional stability during high-flexion weight-bearing activities. Knee Surg Sports Traumatol Arthrosc 10:1–8
Kono K, Tomita T, Futai K, Yamazaki T, Tanaka S, Yoshikawa H et al (2018) In vivo three-dimensional kinematics of normal knees during different high-flexion activities. Bone Jt J 100-b:50–55
Liddle AD, Pandit H, Judge A, Murray DW (2015) Patient-reported outcomes after total and unicompartmental knee arthroplasty: a study of 14,076 matched patients from the National Joint Registry for England and Wales. Bone Jt J 97-b:793–801
Long WJ, Bryce CD, Hollenbeak CS, Benner RW, Scott WN (2014) Total knee replacement in young, active patients: long-term follow-up and functional outcome: a concise follow-up of a previous report. J Bone Jt Surg Am 96:e159
Mochizuki T, Sato T, Blaha JD, Tanifuji O, Kobayashi K, Yamagiwa H et al (2014) Kinematics of the knee after unicompartmental arthroplasty is not the same as normal and is similar to the kinematics of the knee with osteoarthritis. Knee Surg Sports Traumatol Arthrosc 22:1911–1917
Moglo KE, Shirazi-Adl A (2005) Cruciate coupling and screw-home mechanism in passive knee joint during extension–flexion. J Biomech 38:1075–1083
Mont MA, John M, Johnson A (2012) Bicruciate retaining arthroplasty. Surg Technol Int 22:236–242
Nam D, Nunley RM, Barrack RL (2014) Patient dissatisfaction following total knee replacement: a growing concern? Bone Jt J 96-b:96–100
Okada Y, Teramoto A, Takagi T, Yamakawa S, Sakakibara Y, Shoji H et al (2018) ACL function in bicruciate-retaining total knee arthroplasty. J Bone Jt Surg Am 100:e114
Patil S, Colwell CW Jr, Ezzet KA, D'Lima DD (2005) Can normal knee kinematics be restored with unicompartmental knee replacement? J Bone Jt Surg Am 87:332–338
Pritchett JW (2015) Bicruciate-retaining total knee replacement provides satisfactory function and implant survivorship at 23 years. Clin Orthop Relat Res 473:2327–2333
Sabouret P, Lavoie F, Cloutier JM (2013) Total knee replacement with retention of both cruciate ligaments: a 22-year follow-up study. Bone Jt J 95-b:917–922
Shimizu N, Tomita T, Yamazaki T, Yoshikawa H, Sugamoto K (2011) The effect of weight-bearing condition on kinematics of a high-flexion, posterior-stabilized knee prosthesis. J Arthroplasty 26:1031–1037
Stiehl JB, Komistek RD, Cloutier JM, Dennis DA (2000) The cruciate ligaments in total knee arthroplasty: a kinematic analysis of 2 total knee arthroplasties. J Arthroplasty 15:545–550
Tamaki M, Tomita T, Yamazaki T, Hozack WJ, Yoshikawa H, Sugamoto K (2008) In vivo kinematic analysis of a high-flexion posterior stabilized fixed-bearing knee prosthesis in deep knee-bending motion. J Arthroplasty 23:879–885
Tsai TY, Liow MHL, Peng Y, Paul A, Li G, Kwon YM (2018) In-vivo elongation of anterior and posterior cruciate ligament in bi-cruciate retaining total knee arthroplasty. J Orthop Res 36:3239–3246
Von Keudell A, Sodha S, Collins J, Minas T, Fitz W, Gomoll AH (2014) Patient satisfaction after primary total and unicompartmental knee arthroplasty: an age-dependent analysis. Knee 21:180–184
Yamazaki T, Watanabe T, Nakajima Y, Sugamoto K, Tomita T, Yoshikawa H et al (2004) Improvement of depth position in 2-D/3-D registration of knee implants using single-plane fluoroscopy. IEEE Trans Med Imaging 23:602–612
Yoshiya S, Matsui N, Komistek RD, Dennis DA, Mahfouz M, Kurosaka M (2005) In vivo kinematic comparison of posterior cruciate-retaining and posterior stabilized total knee arthroplasties under passive and weight-bearing conditions. J Arthroplasty 20:777–783
Zumbrunn T, Duffy MP, Rubash HE, Malchau H, Muratoglu OK, Varadarajan KM (2008) ACL substitution may improve kinematics of PCL-retaining total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 26:1445–1454
Acknowledgements
We are grateful to Dr. Ryota Yamagami, Dr. Kohei Kawaguchi, Dr. Tomofumi Kage, Dr. Teruya Ishibashi and Dr. Shoji Konda for their cooperation in this research. We also thank our colleagues for their constructive comments. This research did not receive any specific grant from any funding agencies in the public, commercial or not-for-profit sectors.
Funding
There is no funding source.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
We declare that we have no conflict of interest.
Ethical approval
Institutional review board approval was rececived for this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Fluoroscopic analysis. Under fluoroscopy, each participant performed a squatting motion at a natural pace (WMV 5569 kb)
Two-dimensional/three-dimensional (2D/3D) registration of bicruciate-retaining total knee arthroplasty knee during squatting motion. The 2D/3D registration of the femoral and tibial implants was performed initially, followed by the 2D/3D registration of the femoral and tibial bone models (WMV 5541 kb)
Rights and permissions
About this article
Cite this article
Kono, K., Inui, H., Tomita, T. et al. Bicruciate-retaining total knee arthroplasty reproduces in vivo kinematics of normal knees to a lower extent than unicompartmental knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 28, 3007–3015 (2020). https://doi.org/10.1007/s00167-019-05754-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-019-05754-2