Abstract
Purpose
To examine the role of the posterior fan-like extension of the ACL’s femoral footprint on the ACL failure load.
Methods
Sixteen (n = 16) fresh frozen, mature porcine knees were used in this study and randomized into two groups (n = 8): intact femoral ACL insertion (ACL intact group) and cut posterior fan-like extension of the ACL (ACL cut group). In the ACL cut group, flexing the knees to 90°, created a folded border between the posterior fan-like extension and the midsubstance insertion of the femoral ACL footprint and the posterior fan-like extension was dissected and both areas were measured. Specimens were placed in a testing machine at 30° of flexion and subjected to anterior tibial loading (60 mm/min) until ACL failure.
Results
The intact ACL group had a femoral insertion area of 182.1 ± 17.1 mm2. In the ACL cut group, the midsubstance insertion area was 113.3 ± 16.6 mm2, and the cut posterior fan-like extension portion area was 67.1 ± 8.3 mm2. The failure load of the ACL intact group was 3599 ± 457 N and was significantly higher (p < 0.001) than the failure load of the ACL cut group 392 ± 83 N.
Conclusion
Transection of the posterior fan-like extension of the ACL femoral footprint has a significant effect on the failure load of the ligament during anterior loading at full extension. Regarding clinical relevance, this study suggests the importance of the posterior fan-like extension of the ACL footprint which potentially may be retained with remnant preservation during ACL reconstruction. Femoral insertion remnant preservation may allow incorporation of the fan-like structure into the graft increasing graft strength.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The goal of anterior cruciate ligament (ACL) reconstruction is to restore the intact tissue’s function. Towards this aim, anatomic ACL reconstruction attempts to recreate the native ACL’s dimensions, collagen orientation and insertion sites [13, 16] and anatomical studies have been done to assess these factors and also to gain an understanding of the ligament’s form and function.
For these reasons, the ACL has been the subject of many anatomical studies, and recent studies have used advances in technology to better control knee loading during measurement and more accurately characterize the complex tissue morphology. Most studies have described the native ACL as having an hourglass shape with direct midsubstance attachments and thin, membranous, peripheral attachments, at both the femoral and tibial insertion sites [1, 3, 5, 6, 8, 10]. Harner et al., used a digital measurement system to quantify the ACL dimensions and found that the cross-sectional areas at the femoral and tibial insertion areas were over three times larger that of the midsubstance cross-sectional area [6]. A recent study employing a laser measurement system and controlled knee loading has also found enlargement of the tissue at the insertion sites with the cross-sectional area of the midsection being less than half the area of the insertion sites [3]. The tissue at the femoral attachment was described as dense midsubstance fibers attach to a narrow oval area on the lateral condyle and there is a fan-like extension of fibers spreading out towards the posterolateral condyle which increase the area of the insertion site [14]. There is, however, still some debate on the ligament morphology with one study characterizing the ACL as being flat and ribbon-like near the femoral insertion [15]. With most studies finding an hourglass like shape of the ligament and the reconstruction goal of restoring the native ACL anatomy, this has led to interest in the functional basis for the morphology.
Recent studies have attempted to determine the function of the flared morphology by trying to assess the load transmission through different regions of the insertion site by testing the knee with the tissue intact, then cutting a portion of the insertion site and retesting the knee. Using this approach, Kawaguchi et al. and Nawabi et al. both concluded that the posterior fan-like extension of the ACL femoral insertion carries only a small portion of the load and contributes little to the anterior–posterior and rotatory stability of the knee [7, 12]. From these results they suggested that placement of the ACL graft should be at the midsubstance or high (anterior) portion of the insertion site.
While previous studies have concluded that the fan-like extension of the ligament bears little load, the purpose of this study is to examine the role of the ACL’s femoral insertion site morphology on the failure of the ligament using a porcine model. It was hypothesized that the posterior fan-like extension of the ACL’s femoral insertion plays a significant role in increasing the ligament failure load. This would indicate the structural importance of the posterior fan-like extension of the ACL footprint which potentially may be retained with remnant preservation during ACL reconstruction and if incorporated could increase graft strength.
Materials and methods
Sixteen (n = 16) fresh frozen, mature porcine knees were used in this study [2]. The porcine analog allows for better control of specimen size, weight and age, where age is a known factor in the human ACL strength [17]. Moreover, the goal of this study was not to determine specific values of ACL failure loads, but to assess the relative effect of cutting of a ligament’s fan-like extension on the failure load.
After disarticulation at the hip joint, skin and subcutaneous layers were removed, and the knee joint capsule was left intact. The specimens were stored at – 20 °C and thawed at room temperature the night before testing [11, 18]. Before testing, the femur and the tibia were sectioned approximately 10 cm from the joint line and potted in epoxy for mounting in aluminum grips.
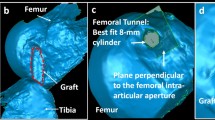
For testing, the knees were fixed in aluminum grips, placed in a custom-made testing fixture, and then mounted to a material testing machine at 30° of flexion (full extension in the porcine knee) (Fig. 2b). The knees were removed, the soft tissue structures other than the ACL were dissected, the condyles removed, and for the ACL cut group the posterior fan-like extension of the ACL was cut. The knees were placed back in the testing machine and subjected to anterior tibial loading with other motions being constrained. A small preload of 2.5 N was applied to the knee, after which it was cyclically preconditioned between 0 and 2 mm of deformation at a rate of 20 mm/min for 10 cycles [17]. The laser measurement system has an accuracy of 0.05 mm (Faro, Inc.). Thereafter, the knee was loaded to failure at a rate of 60 mm/min [4]. The load and elongation were recorded continuously during the test. The failure load that was defined by the maximum load, the displacement at failure that was defined by the displacement of the maximum load, and the forces at 5 mm, 10 mm, 15 mm, and 20 mm of displacement were reported. The failure mode of each specimen was recorded.
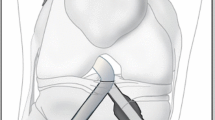
Sixteen knees used for this study and were randomly divided into two groups (n = 8): an intact femoral ACL insertion (ACL intact group) and a cut posterior fan-like extension of the ACL (ACL cut group). Each knee was dissected free of all soft tissue structures, except for the ACL. The medial femoral condyle was removed using a reciprocating saw along with femoral intercondylar notch in order to better visualize the ACL footprint. The border between the midsubstance area and the posterior fan-like extension was apparent with the knee in extension (Fig. 1a), but a folded border becoming more prominent with the knee at 90° of flexion (Fig. 1b) [7]. The area posterior to the folded border was identified as the posterior fan-like extension of the ACL and was dissected from the femur using a surgical no. 11 blade (Fig. 1c) in the cut group.
No border was apparent between the midsubstance area and the posterior fan-like extension with the knee in extension (a). With the knee at 90° of flexion a folded border becoming more prominent (b). The area posterior to the folded border was identified as the posterior fan-like extension of the ACL and was dissected from the femur using a surgical no. 11 blade (c)
To quantify the area of the ACL footprint that was cut, the posterior fan-like extension and the midsubstance insertion of the footprint were outlined and coordinates measured using a digitizing probe (Faro, Inc.) for the ACL cut group. A plane was fitted to the points and the coordinates were exported to computer program (MATLAB, Math Works Inc.) to compute the areas of the posterior fan-like extension and the midsubstance insertion of the ACL footprint (Fig. 2a).
For this study, a review request was presented to the Institutional Review Board and the Institutional Animal Care and Use Committee (IACUC) at the University of Pittsburgh and was determined not to require oversight. Procurement of the porcine knee specimens were from a local meat market.
Statistical analysis
Statistical analysis of the differences in the failure load, the displacement at failure, and the loads at 5 mm, 10 mm, 15 mm and 20 mm of displacement were analyzed using a two-tailed independent t test (SPSS Inc., Chicago, Illinois, USA) with statistical significance was set at p < 0.05. To estimate the number of samples, an a-priori power analysis, based on a 2-tailed paired t test, was performed (v. 3.1.9.2; G*power) using the significance level of 0.05, a power of 0.80, with a hypothesized effect size of d = 1.5, which resulted in n = 14 samples.
Results
For the ACL cut group, the intact ACL had an area of 182.1 ± 17.1 mm2, with a midsubstance insertion area of 113.3 ± 16.6 mm2 and a posterior fan-like extension area of 67.1 ± 8.3 mm2. Thus, the cut area of the posterior fan-like extension insertion site represented 37% of the total ACL insertion site. The failure load of the ACL intact group was 3599 ± 457 N and was significantly higher (p < 0.001) than the 392 ± 83 N failure load of the ACL cut group (Fig. 3).
The displacement at failure of the ACL intact group was 45.6 ± 5.8 mm which was significantly higher (p < 0.001) than the 27.7 ± 7.7 mm failure load displacement of the ACL cut group (Fig. 4). The load required for a given displacement was also significantly higher for the ACL intact group than the ACL cut group for 5 mm, 10 mm, 15 mm, and 20 mm of displacement (Fig. 5).
Evaluation of the failure mode in the ACL intact group revealed a fracture of the tibia in one specimen, and fracture of the femur in seven specimens. In the ACL cut group, all the specimens failed at the ACL femoral insertion.
Discussion
The most important finding of this study is that the posterior fan-like extension of the ACL femoral insertion site (the lower part of the ACL footprint when viewed arthroscopically) significantly contributes to the ACL’s strength. While it comprises less than 50% of the femoral insertion site area, it greatly increases to the ACL’s ability to resist anterior tibial displacement and to ultimate failure load. To the best of our knowledge, this is the first study to evaluate the effects of the posterior fan-like extension of the ACL femoral insertion site on failure load.
Earlier cadaveric studies concluded that the posterior fan-like extension contributes little to knee stability but did not examine the ACL under large loads. Kawaguchi et al. sequentially transected the femoral ACL insertion from posterior to anterior, dividing the footprint into twelve parts [7]. The group examined the anterior load required for 6 mm of anterior tibial displacement and the torque required for 10° of internal and 15° external rotation. The force required to produce the anterior translation ranged from 61 ± 9 N to 123 ± 27 N. Under these conditions, they stated the central-proximal area of the femoral insertion was primarily responsible for providing AP and rotatory stability. Though they did note the low magnitude load as a limitation, they concluded that the entire femoral footprint does not need be covered in ACL reconstruction.
Subsequently, a study by Nawabi et al. examined load transmission across the ACL’s femoral footprint, bisecting the insertion into an anterior band and a posterior extension [12]. Randomly cutting each section, they simulated Lachman, anterior drawer, and pivot shift tests. For all knees, the anterior displacement was evaluated at 134 N. Under their experimental conditions, they found that the anterior fibers bore more force during stability testing and were more isometric during flexion when compared to the posterior extension fibers. Like the Kawaguchi et al. study, they concluded that since the central, anterior portion of the femoral footprint is most important to resisting displacement, suggesting tunnel placement in the “high AM location” in reconstruction.
These studies used sequential cutting of the ligament footprint to assess the force distribution at the ACL insertion and apply this information to reconstruction in terms of how much of the insertion site must be reconstructed and tunnel placement. Since the Kawaguchi et al. study [7] considered the force required for the knee to reach a given displacement, this evaluated changes in tissue stiffness with the cutting of different portions of the insertion proceeding in a fixed sequence from posterior to central area to anterior. The cutting of the central area led to the largest decrease in stiffness.
No ACL reconstruction technique restores the native tissue attachment, fiber orientation or morphology at the insertion site which are the factors governing the force distribution, so there are limitations in assuming that a reconstruction will restore the intact ligament force distribution. With regard to ACL footprint restoration, the aspect of tunnel placement has been evaluated through the study of knee biomechanics with ACL reconstruction techniques that consider this factor in which knee kinematics and graft force are compared to that of the intact ACL for actual reconstruction [2].
By stressing the porcine ACL to failure, this high load test revealed that in the ACL cut group, the ACL failed at 392.0 ± 83.1 N, compared to a significantly higher 3598.9 ± 456.5 N failure load in the ACL intact group. Similarly, in the ACL cut group, the ACL had 27.7 ± 7.7 mm of displacement before failure, significantly less than the 45.6 ± 5.8 mm displacement experienced by the intact ACL. Finally, the forces required to reach given levels of displacement (5 mm, 10 mm, 15 mm, and 20 mm) were significantly lower for the ACL cut group.
The significant findings suggest that under large loads, the posterior fan-like extension plays a substantial role in the strength of the ACL. Though further analysis in human cadavers is necessary, these findings reveal that the femoral footprint morphology is important to resisting ACL failure and should be considered during ACLR. The effect of the fan-like shape of the ligament may serve to reduce stress at the insertion site under loading.
This study has some limitations. Porcine knees were used that have different bone and ACL morphology than humans, however, the porcine model is the preferred animal model for studies of in situ forces in the ACL [9, 19]. Additionally, the porcine model benefits from consistency of specimen size and age. Human cadavers tend to be older and more variable in age and aging significantly decreases linear stiffness, ultimate load, and energy absorbed of the ACL [17]. Future studies could compare age-matched models on failure testing in human specimens.
With regard to clinical relevance, this study sheds light on the contribution of the posterior fan-like extension to resisting ACL failure. In the present study, the posterior fan-like morphology plays a significant role in increasing anterior failure load. This may suggest remnant preservation in ACL reconstruction, which may potentially retain the insertion site morphology. Femoral insertion remnant preservation may allow incorporation of the fan-like structure into the graft increasing graft strength.
Conclusion
Transection of the posterior fan-like extension of the ACL femoral insertion site has a significant effect on the failure load of the ligament during AP translation at full extension. Clinically, consideration should be given remnant preservation in ACL reconstruction.
References
Araki D, Thorhauer E, Tashman S (2018) Three-dimensional isotropic magnetic resonance imaging can provide a reliable estimate of the native anterior cruciate ligament insertion site anatomy. Knee Surg Sports Traumatol Arthrosc 26:1311–1318
Araujo PH, Asai S, Pinto M, Protta T, Middleton K, Linde-Rosen M, Irrgang J, Smolinski P, Fu FH (2015) ACL graft position affects in situ graft force following ACL reconstruction. J Bone Jt Surg Am 97:1767–1773
Fujimaki Y, Thorhauer E, Sasaki Y, Smolinski P, Tashman S, Fu FH (2016) Quantitative in situ analysis of the anterior cruciate ligament: length, midsubstance cross-sectional area, and insertion site areas. Am J Sports Med 44:118–125
Gan Y, Xu D, Ding J, Xu Y (2012) Tension band wire fixation for anterior cruciate ligament avulsion fracture: biomechanical comparison of four fixation techniques. Knee Surg Sports Traumatol Arthrosc 20:909–915
Hara K, Mochizuki T, Sekiya I, Yamaguchi K, Akita K, Muneta T (2009) Anatomy of normal human anterior cruciate ligament attachments evaluated by divided small bundles. Am J Sports Med 37:2386–2391
Harner CD, Livesay GA, Kashiwaguchi S, Fujie H, Choi NY, Woo SL (1995) Comparative study of the size and shape of human anterior and posterior cruciate ligaments. J Orthop Res 13:429–434
Kawaguchi Y, Kondo E, Takeda R, Akita K, Yasuda K, Amis AA (2015) The role of fibers in the femoral attachment of the anterior cruciate ligament in resisting tibial displacement. Arthroscopy 31:435–444
Li F, Qin L, Gong X, Huang Z, Wang T, Liu Z, Sandiford S, Yang J, Zhu S, Liang X, Huang W, Hu N (2019) The Chinese ACL injury population has a higher proportion of small ACL tibial insertion sizes than Western patients. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-019-05541-z
Markolf KL, Hame S, Hunter DM, Oakes DA, Zoric B, Gause P, Finerman GA (2002) Effects of femoral tunnel placement on knee laxity and forces in an anterior cruciate ligament graft. J Orthop Res 20:1016–1024
Mochizuki T, Fujishiro H, Nimura A, Mahakkanukrauh P, Yasuda K, Muneta T, Akita K (2014) Anatomic and histologic analysis of the mid-substance and fan-like extension fibres of the anterior cruciate ligament during knee motion, with special reference to the femoral attachment. Knee Surg Sports Traumatol Arthrosc 22:336–344
Moon DK, Woo SL, Takakura Y, Gabriel MT, Abramowitch SD (2006) The effects of refreezing on the viscoelastic and tensile properties of ligaments. J Biomech 39:1153–1157
Nawabi DH, Tucker S, Schafer KA, Zuiderbaan HA, Nguyen JT, Wickiewicz TL, Imhauser CW, Pearle AD (2016) ACL fibers near the lateral intercondylar ridge are the most load bearing during stability examinations and isometric through passive flexion. Am J Sports Med 44:2563–2571
Rahnemai-Azar AA, Sabzevari S, Irarrázaval S, Chao T, Fu F (2016) Anatomical individualized ACL reconstruction. ABJS 4:291–297
Sasaki N, Ishibashi Y, Tsuda E, Yamamoto Y, Maeda S, Mizukami H, Toh S, Yagihashi S, Tonosaki Y (2012) The femoral insertion of the anterior cruciate ligament: discrepancy between macroscopic and histological observations. Arthroscopy 28:1135–1146
Smigielski R, Zdanowicz U, Drwiega M, Ciszek B, Ciszkowska-Lyson B, Siebold R (2015) Ribbon like appearance of the midsubstance fibres of the anterior cruciate ligament close to its femoral insertion site: a cadaveric study including 111 knees. Knee Surg Sports Traumatol Arthrosc 23:3143–3150
van Eck CF, Lesniak BP, Schreiber VM, Fu FH (2010) Anatomic single- and double-bundle anterior cruciate ligament reconstruction flowchart. Arthroscopy 26:258–268
Woo SL, Hollis JM, Adams DJ, Lyon RM, Takai S (1991) Tensile properties of the human femur-anterior cruciate ligament-tibia complex. The effects of specimen age and orientation. Am J Sports Med 19:217–225
Woo SL, Orlando CA, Camp JF, Akeson WH (1986) Effects of postmortem storage by freezing on ligament tensile behavior. J Biomech 19:399–404
Xerogeanes JW, Fox RJ, Takeda Y, Kim HS, Ishibashi Y, Carlin GJ, Woo SL (1998) A functional comparison of animal anterior cruciate ligament models to the human anterior cruciate ligament. Ann Biomed Eng 26:345–352
Funding
This study was funded by the Department of Orthopaedic Surgery at the University of Pittsburgh.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Authors have no conflicts to disclose.
Ethical approval
No ethical approval was required from IACUC.
Informed consent
Not applicable to this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sabzevari, S., Shaikh, H., Marshall, B. et al. The femoral posterior fan-like extension of the ACL insertion increases the failure load. Knee Surg Sports Traumatol Arthrosc 28, 1113–1118 (2020). https://doi.org/10.1007/s00167-019-05753-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-019-05753-3