Abstract
Purpose
The purpose was to characterize the independent effect of procedure length on the rates of 30-day perioperative complications, hospital readmissions, and overnight hospital stay in patients undergoing arthroscopic anterior cruciate ligament reconstruction (ACLR). We hypothesized that longer procedure length in primary ACLR increases the risk for post-operative complications.
Methods
Primary ACLR cases from 2005 to 2015 were identified in the American College of Surgeons National Surgical Quality Improvement Program registry. Patients were categorized into two cohorts based on procedure length, either less than or greater than 90 min. Two equal-sized propensity-matched cohorts were generated to account for differences in baseline and operative characteristics. Thirty-day clinical outcomes were compared using bivariate analyses between propensity-matched groups that controlled for patient-specific factors and concurrent meniscal repair. Multivariate logistic regression models were used to identify independent predictors of hospital readmission and overnight hospital stay.
Results
In total, 12,077 ACLR cases were identified. The rate of any 30-day complication was increased in longer procedures relative to shorter procedures (1.6% vs 0.9%, p = 0.006), as were the rates of returning to the operating room (0.6% vs 0.3%, p = 0.03), hospital readmission (1.0% vs 0.3%, p = 0.001), and overnight hospital stay (16.2% vs 6.0%, p < 0.001). Obesity was a risk factor for both hospital readmission and overnight hospital stay, while hypertension, diabetes, chronic obstructive pulmonary disease, and a smoking history were associated with increased rates of overnight hospital stay. The most common reasons for hospital readmission were deep vein thrombosis or pulmonary embolism (25.0% of all readmitted patients), surgical site infection (25.0%), and post-operative pain (14.1%).
Conclusions
In this propensity-matched analysis adjusting for baseline patient characteristics and operative factors, procedure length of greater than or equal to 90 min in ACLR was independently associated with an increased risk of hospital readmission and overnight hospital stay. As a surrogate measure of surgical complexity, operative time may be a useful perioperative variable for post-operative risk stratification and patient counseling.
Level of evidence
III
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Anterior cruciate ligament reconstruction (ACLR) is one of the most commonly performed orthopaedic procedures [14, 22]. Both short- and long-term clinical outcomes after ACLR have been well characterized [3, 7, 11, 15, 17, 23, 24, 27, 30, 31]. Perioperative complications occur infrequently, with the rate of symptomatic thromboembolic events reported at between 0.53 and 4.0% [11, 15, 30], septic arthritis between 0.14 and 0.48% [17, 23, 31], urinary tract infection at 0.74% [27], and an inpatient mortality rate under 0.01–0.02% [11, 27]. Risk factors found to be associated with perioperative complications after ACLR include age greater than 20 years and diabetes mellitus, whereas decreased risk has been observed when procedures are performed in hospitals with a high volume of reconstructions [7, 22, 27].
While perioperative complication rates are low with arthroscopic procedures, there are various operative factors which have been associated with an increased incidence of complications. In knee arthroscopy, patient-related risk factors such as corticosteroid injection at the time of arthroscopy have been associated with significantly increased post-operative infection rates [8]. Other known risk factors for infection following knee arthroscopy include: age, obesity, tobacco use, and a number of medical comorbidities [9]. Furthermore, differences in arthroscopic irrigation fluid temperature and osmolarity may also have a variable impact on core body temperature and articular cartilage viability [10, 25, 26]. However, studies assessing the impact of procedure time on short-term clinical outcomes after arthroscopic ACLR are lacking.
The association between operative time and post-operative complications in ACLR is presently unclear. Accordingly, the primary aim of this study was to use a large national registry to assess for independent associations between procedure time in ACLR, and 30-day post-operative complications and readmissions rates. Secondary aims were to identify patient-specific factors associated with hospital readmission and overnight hospital stay and to determine the most common reasons for readmission after ACLR. We hypothesized that longer procedure length in primary ACLR increases the risk for post-operative complications. Procedure length may be a surrogate for surgical complexity, and is also useful as a perioperative variable for risk stratification and patient counseling.
Materials and methods
Following approval of the institutional review board, the American College of Surgeons National Surgical Quality Improvement Program (NSQIP) database was accessed. This national registry was established in 2005 and is updated annually, with data available for over 4 million unique surgical encounters as of 2015 [1]. The NSQIP contains patient demographical information, intraoperative variables including operative time, and post-operative complications and readmissions up to 30 days after surgery. Post-operative events for 30 days are reported irrespective of length of hospital stay. Data collection is performed by trained surgical clinical reviewers, and audited by the American College of Surgeons to ensure accuracy and reliability of the data. As a result, there is high interrater reliability, with a disagreement rate of only 1.56% as of 2015 [29]. Perhaps due to this frequent auditing, the NSQIP database is more accurate compared to other large registries, such as insurance administrative claims databases [12, 19].
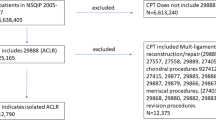
Baseline patient characteristics and perioperative complications
This study used NSQIP data over a 10-year period, from 2005 to 2015. Patients who underwent ACLR were identified with a primary Current Procedural Terminology (CPT) 29888. Patients with dirty wound classifications, surgical procedures considered emergent, multi-ligament reconstructions, and those with missing baseline patient and operative characteristics were excluded from this study. Baseline patient and operative characteristics that were assessed in this study included: age, sex, body mass index (BMI), American Society of Anesthesiologists (ASA) class, operation length, whether or not a patient underwent a concurrent meniscus repair, and medical comorbidities including hypertension, chronic obstructive pulmonary disease (COPD), smoking history, and diabetes mellitus. Concurrent meniscus repair was identified using secondary CPT codes 29882 (medial or lateral repair) and 29883 (medial and lateral repair).
Clinical outcomes assessed in this study included 30-day readmissions, whether or not a patient needed overnight hospital stay, and perioperative complications including surgical site infections, wound dehiscence, urinary tract infection, return to the operating room, deep vein thrombosis or pulmonary embolism (DVT/PE), and respiratory complications. For patients that were readmitted, the reason for readmission was recorded. The NSQIP began collecting readmission information in 2011, and these data were available for 79.1% of patients who underwent arthroscopic ACLR between 2005 and 2015 in this current study. Institutional review board approval for this current study was obtained from the Hospital for Special Surgery (#2017-0463).
Statistical analysis
A propensity score-matched analysis was performed to account for differences in baseline patient and operative characteristics between the two cohorts, patients with an operative time less than 90 min or greater than or equal to 90 min. This methodology has been established in large data set outcomes research in orthopaedic surgery [5, 6, 13]. In the current study, the propensity score is defined as the conditional probability that a patient has an operative time greater than or equal to 90 min, while controlling for patient age, sex, body mass index, medical comorbidities, ASA class, and concurrent meniscus repair. Two equal-sized, propensity-matched cohorts undergoing arthroscopic ACLR less than and greater than or equal to 90 min were generated using 1:1 matching with tight calipers (0.001) and nearest-neighbor matching [21]. Nearest-neighbor matching selects for patients in both groups with the smallest difference in propensity score. Once these two patients are matched by this method, they are removed from the eligible pool of patients available to be matched. The next two patients in each group with the closest propensity scores are selected for, and this process is continued until no more eligible patients are available. Two operative time cohorts were used in this study to allow for rapid stratification of a patient into the appropriate cohort. Next, clinical outcome variables between both groups, including complications and readmissions, were compared using Pearson’s Chi-squared test. A multivariate binary logistic regression with readmission and overnight hospital stay as outcome variables and baseline patient and operative characteristics as covariates was performed to identify preoperative risk factors for these two complications. Statistical significance was defined as a p value less than 0.05. SPSS version 23 (IBM Corporation, Armonk, NY) was used for all statistical analyses.
Results
Baseline patient and operative characteristics
In total, 12,077 ACLR cases were identified (Table 1). 5584 (46.2%) of these patients had a procedure lasting less than 90 min, and 6493 (53.8%) had a procedure lasting greater than or equal to 90 min. The mean procedure length in the shorter procedure cohort was 67 (± standard deviation 15) min, and was 132 (± 50) min in the longer procedure cohort. A bivariate comparison of the non-propensity-matched groups found that patients who had a longer procedure were more likely to be younger (p < 0.001), male (p < 0.001), and have a lower ASA class (p < 0.001). After generating propensity-matched cohorts, the differences seen in the unadjusted groups were no longer observed upon bivariate analysis.
Bivariate analysis for perioperative complications
With bivariate analysis of the propensity-matched cohorts, the rate of any complication was found to be significantly increased in ACLR with operative times greater than or equal to 90 min (1.6%), compared to those under 90 min (0.9%, p = 0.006) (Table 2). There was also a significantly increased rate of returning to the operating room in the longer procedure length group (0.6%) relative to the shorter procedure length group (0.3%, p = 0.03). Furthermore, patients with a longer procedure had a significantly higher rate of 30-day readmission (1.0%, p = 0.001) and overnight hospital stay (16.2%, p < 0.001) compared to those with a shorter procedure (0.3% and 6.0%, respectively).
Multivariable analysis for risk factors for complications
Operative time greater than or equal to 90 min was an independent predictor of 30-day hospital readmission (OR 2.53, p = 0.001), any peri- or post-operative complication (OR 1.61, p = 0.007), and overnight hospital stay (OR 2.97, p < 0.001) (Table 3). BMI greater than 40 kg/m2 was also an independent predictor of hospital readmission (OR 5.01, p < 0.001) and any peri- or post-operative complication (OR 2.10, p = 0.025). Risk factors for overnight hospital stay were male sex (OR 0.86, p = 0.018), medical comorbidities such as diabetes mellitus (OR 1.83, p = 0.004), COPD (OR 2.56, p = 0.029), and a smoking history (OR 1.18, p = 0.029), as well as BMI between 30 and 34.9 kg/m2 (OR 1.25, p = 0.003), BMI of 35.0 and 39.9 (OR 14.2, p = 0.002), and BMI greater than 40 (OR 1.50, p = 0.004).
Reasons for hospital readmission
In total, 64 patients (0.7% of all patients in this study) were identified with a 30-day readmission in the unadjusted cohorts. 17 of these (26.6%) had a procedure lasting under 90 min, while 47 (73.4%) had a procedure lasting greater than or equal to 90 min (Table 4). Of all readmitted patients in each group, 11.8% of the patients in the shorter operative time group were readmitted for a deep vein thrombosis or pulmonary embolism, compared to 29.8% in the longer operative time group.
Discussion
The most important finding of the present study was that there are increases in adverse post-operative outcomes as the duration of ACLR increases. Previous studies have incompletely assessed the effect of operative time on clinical outcome and complication risk after ACLR. Using a national, prospectively collected registry, the impact of operative time on 30-day complication and readmission rates was identified. When controlling for baseline patient and operative characterizes using a propensity-adjusted model, we found that there were increased rates of any complication, overnight hospital stay, hospital readmission, and return to the operating room in ACLR requiring greater than or equal to 90 min of operative time, relative to those requiring less than 90 min.
Previous studies assessing procedure time-dependent effects on short-term clinical outcomes in ACLR are lacking. However, procedure length has been associated with poorer outcomes in other arthroscopic procedures. A 2011 study of 418,323 patients undergoing any arthroscopic procedure of the knee found a nearly threefold increase in the odds of symptomatic pulmonary embolisms in procedures lasting greater than 90 min, relative to those lasting under 30 min [16]. Similarly, a study assessing the risk factors for complications in all arthroscopic shoulder procedures identified a nearly twofold increase in any complication when procedures lasted longer than 90 min [28]. However, these studies looked at all knee or shoulder arthroscopic procedures in aggregate, without isolating any particular procedure. Furthermore, they did not control for the number of concurrent arthroscopic procedures performed in each patient in their multivariate analyses. One of the most common reasons for readmission was identified as DVT/PE in the longer operative time cohort relative to the shorter operative time cohort in this current study. Procedure length has also been implicated a negative prognostic factor in longer term and functional outcomes, for instance when assessing rotator cuff repair a longer procedure length was identified as an independent predictor of rotator cuff re-tears following arthroscopic rotator cuff repair [20]. Similar studies assessing long-term outcomes, such as the rate of re-tears as a function of procedure length in ACLR have not been described.
In this present study of ACLR, operative time greater than or equal to 90 min was found to be an independent predictor of adverse outcomes, including total 30-day complications, hospital readmission, and overnight hospital stay. The reasons for these associations may not be entirely due to adverse effects of prolonged arthroscopy duration, but is perhaps more likely related to surgical complexity. Our propensity-matching model accounted for concurrent meniscus repair to account for one potential source of increased ACLR procedure complexity. There are, however, additional factors that may prolong the operative time. These can include varying operative techniques, surgeon experience, or the availability of intraoperative support staff who can assist with portions of the procedure such as graft preparation. Therefore, the procedure length may be an overly simplified measure of surgical complexity, but can perhaps act as one helpful tool in post-operative risk stratification. Specifically, patients undergoing ACLR with operative time greater than or equal to 90 min should be monitored more closely for the incidence of unintended perioperative complications. As a simple surrogate measure of surgical complexity, operative time is a useful perioperative variable for post-operative risk stratification and patient counseling.
In addition to increased procedure duration, BMI greater than 40 kg/m2 was identified as an independent predictor of hospital readmission, any complication, and overnight hospital stay. Furthermore, in this current study, we identified the most common reason for 30-day hospital readmission after ACLR as DVT/PE in all patients. In procedures lasting greater than or equal to 90 min, the reason for readmission in nearly 30% of these patients was DVT/PE. Increased immobility in longer procedures may increase the risk of subsequent DVT/PE as venous stasis is a risk factor for thromboembolic events. In addition to procedure length, patients with a BMI greater than 40 kg/m2 had more than five times higher odds of hospital readmission. Obesity has been identified previously as a risk factor for DVT, perhaps due to the pro-thrombotic forces of chronic inflammation and impaired fibrinolysis seen in this patient population [4]. Prophylactic agents such as aspirin or low-molecular-weight heparin are not routinely used after arthroscopic knee procedures [2, 18], but may be warranted in those with significant risk factors such as increased procedure duration and extreme obesity. Further studies are needed to assess the benefit-to-risk ratio of this approach in these higher risk patients. Whether or not anti-thrombotic agents are utilized, these high-risk patients should be educated on the symptoms of DVT and encouraged to employ non-pharmacological strategies to prevent DVT such as periodic leg elevation, compressive stockings, as well as early ambulation.
This study has several limitations. First, due to limitations in the database, we lack specific clinical variables that are relevant to arthroscopic ACLR. Specifically, information regarding physical examination findings, functional outcomes, graft type, and the rate of graft failure or re-tears was not collected in the NSQIP. In particular, graft selection may have an important impact on procedure length, particularly when comparing allograft with autograft. Furthermore, the NSQIP only contains post-operative outcomes data until 30 days after the index procedure. Therefore, we were unable to identify the time-dependent association impact of procedure length on medium- and long-term clinical outcomes. Finally, the NSQIP only obtains information on surgical procedures at participating institutions, and therefore, the patients included in this study may not be representative of all patients undergoing arthroscopic ACLR. However, as of 2015, there were over 600 separate institutions participating in this registry, ranging from large academic centers to smaller community hospitals [1].
Conclusions
In this propensity-matched analysis adjusting for baseline patient characteristics and operative factors, and procedure length of greater than or equal to 90 min in ACLR was independently associated with an increased risk of hospital readmission and overnight hospital stay. As a surrogate measure of surgical complexity, operative time is a useful perioperative variable for post-operative risk stratification and patient counseling.
References
ACS NSQIP Participant Use Data Files. https://www.facs.org/quality-programs/acs-nsqip/program-specifics/participant-use. Accessed May 1, 2017
Adala R, Anand A, Kodikal G (2011) Deep vein thrombosis and thromboprophylaxis in arthroscopic anterior cruciate ligament reconstruction. Indian J Orthop 45:450–453
Ardern CL, Taylor NF, Feller JA, Webster KE (2014) Fifty-five per cent return to competitive sport following anterior cruciate ligament reconstruction surgery: an updated systematic review and meta-analysis including aspects of physical functioning and contextual factors. Br J Sports Med 48:1543–1552
Blokhin IO, Lentz SR (2015) Mechanisms of thrombosis in obesity. Curr Opin Hematol 20:437–444
Boddapati V, Fu MC, Mayman DJ, Su EP, Sculco PK, McLawhorn AS (2018) Revision total knee arthroplasty for periprosthetic joint infection is associated with increased postoperative morbidity and mortality relative to noninfectious revisions. J Arthroplasty 33:521–526
Boddapati V, Fu MC, Schairer WW, Ranawat AS, Dines DM, Dines JS (2017) Increased shoulder arthroscopy time is associated with overnight hospital stay and surgical site infection. Arthroscopy 34:363–368
Brophy RH, Huston LJ, Wright RW, Nwosu SK, Kaeding CC, Parker RD et al (2016) Outcomes of ACL reconstruction in patients with diabetes. Med Sci Sports Exerc 48:969–973
Cancienne JM, Gwathmey FW, Werner BC (2016) Intraoperative corticosteroid injection at the time of knee arthroscopy is associated with increased postoperative infection rates in a large medicare population. Arthroscopy 32:90–95
Cancienne JM, Mahon HS, Dempsey IJ, Miller MD, Werner BC (2017) Patient-related risk factors for infection following knee arthroscopy: an analysis of over 700,000 patients from two large databases. Knee 24:594–600
Capito NM, Smith MJ, Stoker AM, Werner N, Cook JL (2015) Hyperosmolar irrigation compared with a standard solution in a canine shoulder arthroscopy model. J Shoulder Elbow Surg 24:1243–1248
Cvetanovich GL, Chalmers PN, Verma NN, Cole BJ, Bach BR Jr (2016) Risk factors for short-term complications of anterior cruciate ligament reconstruction in the United States. Am J Sports Med 44:618–624
Davenport DL, Holsapple CW, Conigliaro J (2009) Assessing surgical quality using administrative and clinical data sets: a direct comparison of the university health system consortium clinical database and the national surgical quality improvement program data set. Am J Med Qual 24:395–402
Fu MC, Boddapati V, Gausden EB, Samuel AM, Russell LA, Lane JM (2017) Surgery for a fracture of the hip within 24 hours of admission is independently associated with reduced short-term post-operative complications. Bone Joint J 99b:1216–1222
Garrett WE Jr, Swiontkowski MF, Weinstein JN, Callaghan J, Rosier RN, Berry DJ et al (2006) American Board of Orthopaedic Surgery Practice of the Orthopaedic Surgeon: Part-II, certification examination case mix. J Bone Joint Surg Am 88:660–667
Gaskill T, Pullen M, Bryant B, Sicignano N, Evans AM, DeMaio M (2015) The prevalence of symptomatic deep venous thrombosis and pulmonary embolism after anterior cruciate ligament reconstruction. Am J Sports Med 43:2714–2719
Hetsroni I, Lyman S, Do H, Mann G, Marx RG (2011) Symptomatic pulmonary embolism after outpatient arthroscopic procedures of the knee: the incidence and risk factors in 418,323 arthroscopies. J Bone Joint Surg Br 93:47–51
Indelli PF, Dillingham M, Fanton G, Schurman DJ (2002) Septic arthritis in postoperative anterior cruciate ligament reconstruction. Clin Orthop Relat Res 398:182–188
Kaye ID, Patel DN, Strauss EJ, Alaia MJ, Garofolo G, Martinez A et al (2015) Prevention of venous thromboembolism after arthroscopic knee surgery in a low-risk population with the use of aspirin a randomized trial. Bull Hosp Jt Dis 73:243–248
Lawson EH, Louie R, Zingmond DS, Brook RH, Hall BL, Han L et al (2012) A comparison of clinical registry versus administrative claims data for reporting of 30-day surgical complications. Ann Surg 256:973–981
Le BT, Wu XL, Lam PH, Murrell GA (2014) Factors predicting rotator cuff retears: an analysis of 1000 consecutive rotator cuff repairs. Am J Sports Med 42:1134–1142
Lunt M (2014) Selecting an appropriate caliper can be essential for achieving good balance with propensity score matching. Am J Epidemiol 179:226–235
Lyman S, Koulouvaris P, Sherman S, Do H, Mandl LA, Marx RG (2009) Epidemiology of anterior cruciate ligament reconstruction: trends, readmissions, and subsequent knee surgery. J Bone Joint Surg Am 91:2321–2328
McAllister DR, Parker RD, Cooper AE, Recht MP, Abate J (1999) Outcomes of postoperative septic arthritis after anterior cruciate ligament reconstruction. Am J Sports Med 27:562–570
Nwachukwu BU, Voleti PB, Berkanish P, Chang B, Cohn MR, Williams RJ 3rd et al (2017) Return to play and patient satisfaction after acl reconstruction: study with minimum 2-year follow-up. J Bone Joint Surg Am 99:720–725
Pan X, Ye L, Liu Z, Wen H, Hu Y, Xu X (2015) Effect of irrigation fluid temperature on core body temperature and inflammatory response during arthroscopic shoulder surgery. Arch Orthop Trauma Surg 135:1131–1139
Parodi D, Valderrama J, Tobar C, Besomi J, Lopez J, Lara J et al (2014) Effect of warmed irrigation solution on core body temperature during hip arthroscopy for femoroacetabular impingement. Arthroscopy 30:36–41
Scillia AJ, Issa K, Boylan MR, McDermott JD, McInerney VK, Patel DV et al (2016) Inpatient cruciate ligament reconstruction in the United States: a nationwide database study from 1998 to 2010. Orthopedics 39:e196–202
Shields E, Thirukumaran C, Thorsness R, Noyes K, Voloshin I (2015) An analysis of adult patient risk factors and complications within 30 days after arthroscopic shoulder surgery. Arthroscopy 31:807–815
Shiloach M, Frencher SK Jr, Steeger JE, Rowell KS, Bartzokis K, Tomeh MG et al (2010) Toward robust information: data quality and inter-rater reliability in the American College of Surgeons National Surgical Quality Improvement Program. J Am Coll Surg 210:6–16
Struijk-Mulder MC, Ettema HB, Verheyen CC, Buller HR (2013) Deep vein thrombosis after arthroscopic anterior cruciate ligament reconstruction: a prospective cohort study of 100 patients. Arthroscopy 29:1211–1216
Williams RJ 3rd, Laurencin CT, Warren RF, Speciale AC, Brause BD, O’Brien S (1997) Septic arthritis after arthroscopic anterior cruciate ligament reconstruction. Diagnosis and management. Am J Sports Med 25:261–267
Funding
No sources of funding for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Ranawat reports royalties from Conformis, consulting fees from Stryker, and Arthrex, outside the submitted work. No other authors have financial disclosures.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
This study utilized de-identified publicly available data and therefore formal consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Boddapati, V., Fu, M.C., Nwachukwu, B.U. et al. Procedure length is independently associated with overnight hospital stay and 30-day readmission following anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 28, 432–438 (2020). https://doi.org/10.1007/s00167-019-05622-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-019-05622-z