Abstract
Purpose
The benefits of simultaneous bilateral total knee arthroplasty (SBTKR) include reduced hospital costs, single anaesthetic exposure and in many cases is also the patient’s preference. Despite these potential benefits, risk-adversity with respect to assumed complications and mortality make it difficult for the orthopaedic surgeon and patient to make an informed decision. This study aimed to address the inconsistencies and lack of consensus in previous literature regarding the short-term complications and clinical safety of SBTKR in patients with end-stage knee osteoarthritis (OA).
Methods
A cohort of 950 knees (475 patients) undergoing surgery between 2008 and 2013 was extracted from a prospectively collected clinical database and retrospectively linked to the Australian Joint Replacement Registry and hospital records. Patients underwent sequential SBTKR by their treating surgeon under one anaesthetic. Basic demographic data and outcome data including complications and mortality were collected. All data were analyzed using descriptive statistics only.
Results
A total of 413 patients and 826 knees were included. The average age of the cohort was 70 years with range between 46 and 88 years. 50% of patients were female. The overall mortality rate during the study follow-up period was 1.9%, with an average time to death postoperatively of 23.8 months. There were no cases of acute postoperative mortality (< 6 weeks). Medical complication rates were low.
Conclusions
In contrast to the higher mortality and complication rates suggested in previous literature, this study has demonstrated that SBTKR is safe, with low mortality and complication rates under the current surgical protocol.
Level of Evidence
IV.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
End-stage knee osteoarthritis (OA) is a common clinical presentation, particularly in older patients, and once nonsurgical measures have become ineffective and surgery is indicated, the option is usually a total knee replacement (TKR). For patients requiring bilateral TKR the options are to either do this as a staged procedure (StBTKR), or to do both TKR under the same anaesthetic as a simultaneous procedure (SBTKR). SBTKR involves one surgical event under one anaesthetic, while staged procedures require two operations under two separate anesthetics, separated by a variable time interval depending on the preference of the patient and treating surgeon. The potential benefits of SBTKR include reduced hospital stay and costs, a single anaesthetic exposure, decreased overall rehabilitation time, and in some cases patient preference [6, 18, 23, 24, 28, 35, 41, 47].
There have traditionally been concerns amongst orthopaedic surgeons regarding the safety of SBTKR, usually leading to a reluctance to offer this procedure to patients. The literature examining the safety of SBTKR contains conflicting findings, making it difficult to obtain clear guidelines. Some studies have demonstrated that staged procedures are safer and produce better outcomes than SBTKR [21, 52], while others have described an increased risk of mortality [19, 34, 55] and serious complications including deep vein thrombosis, pulmonary embolism, and cardiovascular events associated with SBTKR [9, 26, 29, 36]. Other studies, however, have failed to detect any significant difference in mortality or the above complications between the two approaches [12, 16, 19, 29, 31, 32, 38, 42, 48], while in other studies, SBTKR demonstrated fewer complications than staged procedures [17, 46]. Despite the potential benefits of SBTKR, risk aversion with respect to associated mortality and morbidity has restricted its clinical application in some centres. However, the variable results for mortality and morbidity in these studies may be outweighed by the benefits of reduced costs and convalescent time, with equivalent functional outcomes [13, 27, 53].
The lack of consensus in the relevant literature may be explained by methodological flaws in previous studies. Several reports of complications in bilateral total knee arthroplasty may have selection bias, as patients with more comorbidities are often deemed inappropriate candidates for SBTKR and are excluded, an issue that may also be present in this study [5, 39, 40, 42, 54]. Also, comparisons between SBTKR and StBTKR should involve doubling of complication rates in unilateral total knee arthroplasty but this is often not clearly described [29, 39, 50]. What is exactly meant by “SBTKR”is also often not clearly defined, and there may be significant differences in the outcomes of surgery in which two TKR are done by two surgeons at the same time under tourniquet, when compared to procedures in which one surgeon does the procedures consecutively without tourniquet. Conflicting findings within the contemporary literature limit the ability of the orthopaedic surgeon or patient to develop an informed decision regarding surgical treatment. There are no evidence-based guidelines regarding the optimal choice between SBTKR or StBTKR that have been developed from consistent high quality, comparable data.
To help address this gap in the knowledge and to better inform clinical practice, the purpose of this study was to carefully assess the safety of SBTKR in a large cohort of patients to either confirm the safety of this surgical option, or alternatively to reaffirm and better define the concerns regarding the inherent risks of this procedure. Unlike previous studies in the literature which took place in the 1980s, this more recent study examines outcomes following significant advancements in anaesthesiology, surgical technique and postoperative care such as hypotensive anaesthesia, computer navigation and tranexamic acid.
Materials and methods
This study is a retrospective analysis of prospectively collected data on a cohort of 475 patients (950 knees) operated on by three orthopaedic surgeons in two private hospitals in Sydney, Australia. The data was extracted from the clinical database (Socrates, v3.5, Orthosoft, AUS) and retrospectively linked to the Australian Joint Replacement Registry and hospital records over a five year period, from 2008 until 2013. The study was approved by the Northern Sydney Local Health District Human Research Ethics Committee (NSLHD HREC Reference Number NSPHEC 2014-LNR-006).
Inclusion criteria
The database recorded all TKAs performed by three consultant Orthopaedic Surgeons at two private hospitals in Sydney, Australia. Patients identified as having undergone SBTKR had two primary total knee arthroplasty procedure codes entered on the same day, as required by discharge coding rules.
Indications for SBTKR were bilateral end stage osteoarthritis with each knee independently meeting criteria for TKR as assessed by the treating orthopaedic surgeon and patient preference for simultaneous bilateral surgery. Preoperative anaesthesiologist review of each patient, which included assessment of medical co-morbidities to evaluate fitness for anaesthesia and surgery. When deemed necessary by the anaesthesiologist, further physician review for these comorbidities, such as that of a cardiologist or respiratory physician, was attained. Those deemed to be unsafe for anaesthesia were excluded from surgery. Patients with severe lower limb vascular insufficiency or active infection in the knee joint or elsewhere in the body were also excluded.
Postoperative high dependency unit (HDU) admission was not routine but was planned if deemed necessary by the anaesthesiologist or surgeon.
Demographic data
Demographic data collected on the patients included age, gender, past medical history. Body-mass index (BMI) was also reported using a single tape measure and scales at the preoperative appointment, recorded to one decimal point. Particular note regarding previous cardiac comorbidity history was also taken. Significant cardiac comorbidity was defined as a patient who had at least one of the following: confirmed diagnosis of congestive cardiac failure, ischaemic heart disease, myocardial infarction, presence of in situ cardiac stent or previous cardiac valve repair or replacement.
The American Society of Anaesthesiologists classification of physical health (ASA) score for each patient, assessed preoperatively, was also retrieved from operative notes.
Surgery protocol
In all cases a computer navigation system was used. Tourniquets were used from 2008 until mid-2011, after which tourniquet was not used in any patient. Routine use of intravenous and intraarticular tranexamic acid commenced in late 2011. Patients underwent sequential SBTKR by the treating orthopaedic surgeon under one anaesthetic commencing with the most symptomatic knee. Prior to commencement of the second total knee arthroplasty, the first knee replacement was completed and the wound closed, and permission to proceed was confirmed with the anaesthetist. Preference was for spinal anaesthetic combined with sedation, which was employed in 80% of patients, with the remainder undergoing general anaesthetic.
Outcome evaluation
Mortality and all complications were recorded from analysis of clinical records up to October 2015. Acute medical complications evaluated included death, deep vein thrombosis, pulmonary embolism, cerebral vascular accident, myocardial infarction, other perioperative cardiac complications, respiratory complications, gastrointestinal complications, urinary complications, and confusion.
Minor surgical complications recorded included intraoperative skin tear and superficial wound infections requiring debridement but not implant removal. Major orthopaedic complications included deep wound infections requiring take back to theatre or implant revision.
Statistical analysis
The cohort was analyzed using descriptive statistics of patient characteristics and surgical outcomes. The data was checked for normality by observing the histogram and q–q plot. All statistical analyses were conducted with Stata 14.0 software (StataCorp).
Results
Patient demographics
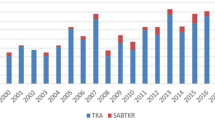
Sixty-two patients were excluded from the analysis due to incomplete hospital records. Confirmation that none of these patients died by the conclusion of the data collection period (September 2016) was based on data provided by the national Australian joint registry. This left a cohort of 413 patients (826 knees) who underwent SBTKR between January 2008 and January 2014.
The mean age of the patients at the time of undergoing SBTKR was 69.5 (46–88 years). Mean patient body mass index (BMI) was 30. The majority of patients had an ASA score of 2 (45.8%), followed by 1 (27.4%), 3 (22.8%) and 4 (4.1%.)37 patients (8.9%) had cardiac comorbidity preoperatively, and 27 patients (6.5%) had a previous thromboembolism.
Mean operative time for each patient was 228.3 ± 27.4 min from skin incision to closure. Mean tourniquet time for patients underwent tourniquet was 47.2 ± 25.9 min. 64.5% of patients underwent cemented femur fixation. All patients underwent patella resurfacing.
Mortality and complications
There were no cases of perioperative mortality, and no cases recorded in the acute postoperative period (6 weeks).The overall mortality rate during the study follow-up period was 1.9% (8 patients), with an average time to death of 23.8 months. Medical complication rates ranged from 31.7% (blood transfusion) to 1.9% (confusion). The transfusion rate reduced between 2009 (64.3%) and 2010 (49%), followed by a steady decline to a final rate of 8% in 2013. Deep vein thrombosis occurred in 2.7% (11 patients), pulmonary embolism occurred in 1.9% (8 patients), cerebral vascular accident occurred in 0.5% (2 patients), and myocardial infarct occurred in 0.2% (1 patient). Minor surgical complication rates were less common, but included superficial wound infection in 0.97% (4 patients) and intraoperative skin tear in 0.24% (1 patient). Deep periprosthetic wound infection occurred in 0.7% (3 patients) of patients of which only one knee required further surgery. Twelve patients (2.9%) experienced an unexpected HDU admission.
Age
Stratification of the cohort into four distinct groups based on age was performed to identify if mortality rates or complications were increased in older patients compared to those younger undergoing SBTKR [33]. To do this, the cohort was separated into arbitrary cut-offs of patients under 60 (7.7% of patients), those between 60 and 70 (43.8%), those between 70 and 80 (37.7%) years of age and those older than 80 (10.7%).
A total of 8 patients over the age of 70 years experienced mortality compared to 0 patients under the age of 70. Of these 8 patients, 4 were above the age of 80 and the other 4 were between 70 and 80 years. As there was no mortality in patients under 70, statistical analysis was unable to be performed for significance comparing these groups. Interestingly, the mortality rate reported for the time frame of the present study is lower than the reported 2.9% yearly mortality rate in the Australian general population among patients aged 70–74, as reported by the Australian Institute of Health and Welfare (AIHW) [56].
Complication rates were also assessed, defined as a diagnosis of DVT, PE, MI, CVA, surgical site infection or confusion in the immediate postoperative period. 2 patients under the age of 60 (6.3%), 12 patients between 60 and 70 (6.6%), 9 patients between 70 and 80 (5.7%) and 7 patients over 80 (15.9%) were identified to have postoperative complications. This overall pooled complication rate was noted to be statistically significant on univariate analysis (p < 0.05) but not after adjusting for sex and operating surgeon (n.s.)
Cardiac history
Six (1.6%) of 376 patients without a cardiac history experienced mortality during the follow-up period compared to two out of 37 (5.4%) patients who did have a cardiac history. Although we did identify a positive association between cardiac comorbidity and mortality, this was not statistically significant on either univariate [OR = 2.27, (n.s), 95% CI 0.69–18.1.] or after adjusting for age, sex or operating surgeon [OR = 1.23, (n.s), 95% CI 0.46–17.2.]
Comparison was also made of the rate of postoperative complications, defined as at least one of postoperative DVT, PE, MI, CVA, wound infection requiring antibiotics or confusion, between patients with a significant cardiac history compared to those who did not. We found that 6.9% (26) of patients without a cardiac history had at least one complication postoperatively compared to 10.8% (4) of patients with a cardiac history. Again, although there was a positive association between cardiac history and postoperative complication, there was no statistically significant difference on either univariate [OR = 1.63, (n.s), 95% CI 0.54–4.96] or multivariate analysis [OR = 1.47, (n.s), 95%CI 0.47–4.56.]
Discussion
The most important finding of the present study was the low mortality and complication rates of one-anaesthetic SBTKR. In this study of 413 patients who underwent SBTKR, there were no cases of perioperative or acute post-operative morbidity. Overall morbidity during the entire follow-up period was found to be actually less than that reported for age matched population norms in Australia [3]. Although direct comparison to a cohort with unilateral or staged procedures was not performed, major and minor surgical complication rates are comparable to those reported in the literature for these types of procedures.
Complication rates and clinical safety of SBTKR remains a controversial topic with lack of consensus present in the literature. Previous studies have reported inhospital mortality rates ranging from 0% up to 4.3%. In addition to increased incidence of HDU admission due to cardiac or respiratory complications, other serious complications such as deep venous thrombosis, pulmonary embolism, and myocardial infarction differ in incidence in SBTKR compared to StBTKR throughout the literature [1, 2, 5, 11, 15, 20, 32, 45].
Nevertheless a common perception persists amongst orthopaedic surgeons that SBTKR carries a significantly higher risk profile. As a result, patients are often inappropriately denied the benefits of SBTKR. These benefits include a faster overall recovery, improved patient satisfaction, and reduced costs for the patient and the health care system. In addition, for patients with severe deformities, unilateral deformity correction creates an asymmetric lower limb profile that may impact on rehabilitation. It should also be noted that when patients are intended to undergo staged procedures, there will be a certain percentage who may ultimately not return for the second procedure, and as a result may receive limited benefit from the single TKR.
The risks of serious medical complications such as deep vein thrombosis (DVT), pulmonary embolism (PE) and myocardial infarction (MI) have been used to justify not performing SBTKR. Our study suggests that this risk-aversion may be misplaced. Only 2.7% of patients in our study suffered deep vein thrombosis, a finding in keeping with Restrespo et al.’s (2007) meta-analysis of 27,807 patients (44,684 knees) from 18 studies over 39 years, where there was no statistically significant difference in the risk of deep vein thrombosis between SBTKR and UTKR. Our study also had a lower incidence of pulmonary embolism and myocardial infarction.
This study also demonstrated low rates of blood transfusions, with blood transfusions occurring in only 31.7% of patients, with transfusion rate steadily declining over the study period. Increased significant blood loss may increase the need for blood transfusions, increasing the possibility for blood transfusion reactions or transmission of blood-borne diseases. In the literature, increased intraoperative blood loss associated with SBTKR is a consistent issue [32, 43, 47]. Patients in the final year of this study had a transfusion rate of 8%, and since study completion this has reduced even further. The combination of preoperative screening and iron transfusions as necessary, hypotensive anaesthesia, and tranexamic acid, both intravenously and topically, have seen this rate reduce to less than 5% with current practices.
Surgical complications experienced were uncommon in this study, and ranged from superficial wound infection (0.97%) to intraoperative skin tear (0.24%). Such rates are low when compared to prior studies in the literature [30.44.51.] Furthermore, we found that our rates for revision procedures secondary to complications were also comparatively low. A summary of the outcomes of the cohort and comparison with the current literature is presented in Table 1.
The authors postulate several explanations as to why outcomes in this study differ from previous, more pessimistic studies in the literature. First, a significant proportion of the literature that investigates perioperative complications after SBTKR took place in the 1980s [4, 10, 53]. Since then, advances in the surgical technique, anaesthesiology, and measures to prevent perioperative complications have been implemented, and almost certainly these improvements have made this procedure much safer. For example, use of computer navigation avoids intramedullary alignment rods and associated fat emboli and avoidance of the tourniquet avoids the metabolic insult that occurs with each tourniquet release. Hypotensive anaesthesia in conjunction with tranexamic acid minimizes blood loss and the need for postoperative transfusion. Completing the first knee prior to commencement of the second maintains a carefully controlled procedure, and improvements in pain management reduce the need for postoperative narcotics and the associated complications.
Second, there is potential selection bias, as the entire cohort of patients were private. As a result, the majority of patients were categorized as either ASA score 1 or 2, and thus may be healthier with fewer comorbidities than cohorts in previous studies. This is also a limitation of our study, as these results may not be generalized to other populations, particularly those of a lower socioeconomic class. However, we still feel that given SBTKR is an elective procedure, our cohort of patients would not be significantly different to any other cohort deemed suitable to undergo the surgery. In addition, whilst we acknowledge that less healthy patients may have a higher risk profile, the current study would suggest that this risk profile would not be higher with SBTKR, compared to staged BTKR, when careful surgical technique is used.
Third, it should be noted that the three surgeons in this study are all experienced high-volume sub-specialist knee surgeons who are comfortable in performing SBTKR, and as such the outcomes may not be representative of all orthopaedic surgeons or those performing the procedure in previous studies.
One of the major limitations of this study is its retrospective design. This could be one of the reasons why there were 62 patients who did not have any hospital medical records. Information on these patients was obtained by searching through the joint replacement and death registries of Australia, and it was found that none of these patients underwent a revision procedure or died within the 1 year postoperative period, confirming that this exclusion had no impact on the perioperative mortality results of this study. The ability to obtain relevant data on these patients from valid secondary sources means that this 13% of the original cohort is not “lost to follow up” for the purposes of this study, but rather has an incomplete dataset such that they cannot be included in all of the relevant analyses of rates of lesser complications.
Considering these findings, the authors suggest that SBTKR should be given greater consideration for patients who have bilateral, end-stage knee osteoarthritis and require bilateral arthroplasty. SBTKR offers the advantages of improved patient satisfaction and cost-effectiveness while maintaining a minimal morbidity and complication rate following the introduction of improved patient selection, anaesthetic and surgical technique and post-operative care.
Conclusions
The safety of SBTKR is a topic that has generated much discussion for many years amongst arthroplasty surgeons. Recent literature has demonstrated significant potential benefits for patients receiving SBTKR, including improved patient satisfaction, cost-effectiveness at an individual and a national level, and at least equivalent clinical outcomes to those of StBTKR. Our study demonstrates that sequential SBTKR performed under the same anaesthetic, with careful preoperative patient selection, can be safe with low mortality and complication rates.
Abbreviations
- OA:
-
Osteoarthritis
- TKR:
-
Total knee replacement
- SBTKR:
-
Simultaneous bilateral total knee replacement
- NSLHD:
-
Northern Sydney Local Health District
- HREC:
-
Human research ethics committee
- HDU:
-
High-dependency unit
- AIHW:
-
Australian institute of Health and Welfare
- DVT:
-
Deep vein thrombosis
- PE:
-
Pulmonary embolism
- MI:
-
Myocardial infarction
- CVA:
-
Cerebrovascular accident
- CI:
-
Confidence intervals
- OR:
-
Odds ratio
- UTKR:
-
Unilateral total knee replacement
- StBTKR:
-
Staged bilateral total knee replacement.
References
Adili A, Bhandari M, Petruccelli D, De Beer J (2001) Sequential bilateral total knee arthroplasty under 1 anesthetic in patients> or = 75 years old: complications and functional outcomes. J Arthroplasty 16(3):271–278
Alemparte J, Johnson GV, Worland RL, Jessup DE, Keenan J (2002) Results of simultaneous bilateral total knee replacement: a study of 1208 knees in 604 patients. J South Orthop Assoc 11(3):153–156
Australian Institute of Health and Welfare (2013) General Record of Incidence of Mortality (GRIM) books. http://www.aihw.gov.au/deaths/grim-books/
Barrett J, Baron JA, Losina E, Wright J, Mahomed NN, Katz JN (2006) Bilateral total knee replacement: staging and pulmonary embolism. J Bone Joint Surg Am 88(10):2146–2151
Benjamin J, Tucker T, Ballesteros P (2001) Is obesity a contraindication to bilateral total knee arthroplasties under one anesthetic? Clin Orthop Relat Res 392:190–195
Besser MI (1983) Bilateral Attenborough total knee replacement as a single procedure. Arch Orthop Trauma Surg 101(4):271–272
Bini SA, Khatod M, Inacio MC, Paxton EW (2014) Same-day versus staged bilateral total knee arthroplasty poses no increase in complications in 6,672 primary procedures. J Arthroplasty 29(4):694–697
Bolognesi MP, Watters TS, Attarian DE, Wellman SS, Setoguchi S (2013) Simultaneous vs staged bilateral total knee arthroplasty among medicare beneficiaries, 2000–2009. J Arthroplasty 28:87–91
Bould M, Freeman BJ, Pullyblank A, Newman JH (1998) Blood loss in sequential bilateral total knee arthroplasty. J Arthroplasty 13:77–79
Brotherton SL, Roberson JR, de Andrade JR, Fleming LL (1986) Staged versus simultaneous bilateral total knee replacement. J Arthroplasty 1(4):221–228
Bullock DP, Sporer SM, Shirreffs TG Jr (2003) Comparison of simultaneous bilateral with unilateral total knee arthroplasty in terms of perioperative complications. J Bone Joint Surg Am 85(10):1981–1986
Cohen RG, Forrest CJ, Benjamin JB (1997) Safety and efficacy of bilateral total knee arthroplasty. J Arthroplasty 12:497–502
Dorr LD, Merkel C, Mellman MF, Klein I (1989) Fat emboli in bilateral total knee arthroplasty: predictive factors for neurologic manifestations. Clin Orthop Relat Res. (248):112–119
Forster MC, Bauze AJ, Bailie AG, Falworth MS, Oakeshott RD (2006) A retrospective comparative study of bilateral total knee replacement staged at a one-week interval. J Bone Joint Surg Br 88(8):1006–1010
Gill GS, Mills D, Joshi AB (2003) Mortality following primary total knee arthroplasty. J Bone Joint Surg Am 85:432–435
Gradillas EL, Volz RG (1979) Bilateral total knee replacement under one anesthetic. Clin Orthop Relat Res 140:153–158
Hardaker WT Jr, Ogden WS, Musgrave RE, Goldner JL (1978) Simultaneous and staged bilateral total knee arthroplasty. J Bone Joint Surg Am 60:247–250
Hooper GJ, Hooper NM, Rothwell AG, Hobbs T (2009) Bilateral total joint arthroplasty: the early results from the New Zealand National Joint Registry. J Arthroplasty 24:1174–1177
Hu J, Liu Y, Lv Z, Li X, Qin X, Fan W (2011) Mortality and morbidity associated with simultaneous bilateral or staged bilateral total knee arthroplasty: a meta-analysis. Arch Orthop Trauma Surg 131(9):1291–1298
Hussain N, Chien T, Hussain F, Bookwala A, Simunovic N, Shetty V, Bhandari M (2013) Simultaneous versus staged bilateral total knee arthroplasty a meta-analysis evaluating mortality, peri-operative complications and infection rates. HSSJ 9:50–59
Husted H, Troelsen A, Otte KS, Kristensen BB, Holm G, Kehlet H (2011) Fast-track surgery for bilateral total knee replacement. J Bone Joint Surg Br 93(3):351–356
Hutchinson JR, Parish EN, Cross MJ (2006) A comparison of bilateral uncemented total knee arthroplasty: simultaneous or staged? J Bone Joint Surg Br 88(1):40–43
Ivory JP, Simpson AH, Toogood GJ, McLardy-Smith PD, Goodfellow JW (1993) Bilateral knee replacements: simultaneous or staged? J R Coll Surg Edinb 38(2):105–107
Jankiewicz JJ, Sculco TP, Ranawat CS, Behr C, Tarrentino S (2004) One-stage versus 2-stage bilateral total knee arthroplasty. Clin Orthop Relat Res. (309):94–101
Kim YH, Choi YW, Kim JS (2009) Simultaneous bilateral sequential total knee replacement is as safe as unilateral total knee replacement. J Bone Joint Surg Br 91:64–68
Kim YH (2001) Incidence of fat embolism syndrome after cemented or cementless bilateral simultaneous and unilateral total knee arthroplasty. J Arthroplasty 16:730–739
Kolettis GT, Wixson RL, Peruzzi WT, Blake MJ, Wardell S, Stulberg SD (1994) Safety of 1-stage bilateral total knee arthroplasty. Clin Orthop Relat Res. (309):102–109
Kovacik MW, Singri P, Khanna S, Gradisar IA (1997) Medical and financial aspects of same-day bilateral total knee arthroplasties. Biomed Sci Instrum 33:429–434
Lane GJ, Hozack WJ, Shah S et al (1997) Simultaneous bilateral versus unilateral total knee arthroplasty: outcomes analysis. Clin Orthop Relat Res 345:106–112
Leonard L, Williamson DM, Ivory JP, Jennison C (2003) An evaluation of the safety and efficacy of simultaneous bilateral total knee arthroplasty. J Arthroplasty 18(8):972–978
Liu TK, Chen SH (1998) Simultaneous bilateral total knee arthroplasty in a single procedure. Int Orthop 22(6):390–393
Lombardi AV, Mallory TH, Fada RA et al (2001) Simultaneous bilateral total knee arthroplasties: who decides? Clin Orthop Relat Res 392:319–329
Lynch NM, Trousdale RT, Ilstrup DM (1997) Complications after concomitant bilateral total knee arthroplasty in elderly patients. Mayo Clin Proc. 72:799–805
Mangaleshkar SR, Prasad PS, Chugh S, Thomas AP (2001) Staged bilateral total knee replacement: a safer approach in older patients. Knee 8(3):207–211
McLaughlin TP, Fisher RL (1985) Bilateral total knee arthroplasties: comparison of simultaneous (two-team), sequential, and staged knee replacements. Clin Orthop Relat Res. (199):220–225
Meehan JP, Danielsen B, Tancredi DJ, Kim S, Jamali AA, White RH (2011) A population-based comparison of the incidence of adverse outcomes after simultaneous-bilateral and staged-bilateral total knee arthroplasty. J Bone Joint Surg Am 93:2203–2213
Memtsoudis SG, Ma Y, Della Valle AG, Mazumdar M, GAber-Baylis LK, MacKenzie CR, Sculco TP (2009) Perioperative outcomes after unilateral and bilateral total knee arthroplasty. Anesthesiology 111(6):1206–1216
Morrey BF, Adams RA, Ilstrup DM, Bryan RS (1987) Complications and mortality associated with bilateral or unilateral total knee arthroplasty. J Bone Joint Surg Am 69(4):484–488
Noble J, Goodall JR, Noble DJ (2009) Simultaneous Bilateral Total Knee Replacement: A persistent controversy. The Knee 16:420–426
Oakes DA, Hanssen AD (2004) Bilateral total knee replacement using the same anesthetic is not justified by assessment of the risks. Clin Orthop Relat Res 428:87–91
Odum SM, Troyer JL, Kelly MP, Dedini RD, Bozic KJ (2013) A cost-utility Analysis comparing the cost-effectiveness of simultaneous and staged bilateral total knee arthroplasty. J Bone Joint Surg Am 95(16):1441
Parvizi J, Sullivan TA, Trousdale RT, Lewallen DG (2001) Thirty-day mortality after total knee arthroplasty. J Bone Joint Surg Am 83(8):1157–1161
Pavone V, Johnson T, Saulog PS, Sculco TP, Bottner F (2004) Perioperative morbidity in bilateral one-stage total knee replacements. Clin Orthop Relat Res 421:155–161
Peskun C, Mayne I, Malempati H, Kosashvili Y, Gross A, Backstein D (2012) Cardiovascular disease predicts complications following bilateral total knee arthroplasty under a single anaesthetic. Knee 19:580–584
Restrepo C, Parvizi J, Dietrich T, Einhorn TA (2007) Safety of simultaneous bilateral total knee arthroplasty: a meta-analysis. J Bone Joint Surg Am 89(6):1220–1226
Reuben JD, Meyers SJ, Cox DD, Elliott M, Watson M, Shim SD (1998) Cost comparison between bilateral simultaneous, staged, and unilateral total joint arthroplasty. J Arthroplasty 13(2):172–179
Ritter M, Mamlin LA, Melfi CA, Katz BP, Freund DA, Arthur DS (1997) Outcome implications for the timing of bilateral total knee arthroplasties. Clin Orthop Relat Res 345:99–105
Ritter MA, Harty LD, Davis KE, Meding JB, Berend M (2003) Simultaneous bilateral, staged bilateral, and unilateral total knee arthroplasty: a survival analysis. J Bone Joint Surg Am 85(8):1532–1537
Ritter MA, Harty LD (2004) Debate: simultaneous bilateral knee replacements: the outcomes justify its use. Clin Orthop Relat Res 428:84–86
Ritter MA, Meding JB (1987) Bilateral simultaneous total knee arthroplasty. J Arthroplasty 2(3):185–189
Shin YH, Kim MH, Ko JS, Park JA (2010) The safety of simultaneous bilateral versus unilateral total knee arthroplasty: the experience in a Korean hospital. Singap Med J 51:44–49
Sliva CD, Callaghan JJ, Goetz DD, Taylor SG (2005) Staggered bilateral total knee arthroplasty performed four to seven days apart during a single hospitalization. J Bone Joint Surg Am 87(3):508–513
Soudry M, Binazzi R, Insall JN, Nordstrom TJ, Pellicci PM, Goulet JA (1985) Successive bilateral total knee replacement. J Bone Joint Surg Am 67(4):573–576
Stanley D, Stockley I, Getty CJ (1990) Simultaneous or staged bilateral total knee replacements in rheumatoid arthritis: a prospective study. J Bone Joint Surg Br 72(5):772–774
Stefansdottir A, Lidgren L, Robertsson O (2008) Higher early mortality with simultaneous rather than staged bilateral TKAs: results from the Swedish Knee Arthroplasty Register. Clin Orthop Relat Res 466:3066–3070
Yoon HS, Han CD, Yang IH (2010) Comparison of simultaneous bilateral and staged bilateral total knee arthroplasty in terms of perioperative complications. J Arthroplasty 25:179–184
Funding
The study was financed by acquired independent research funds, and was not financed by a specific grant.
Author information
Authors and Affiliations
Contributions
All authors (EW, CN, SP, DP) were involved in study design, collection of data, data analysis and manuscript preparation. All authors have read and approved the final manuscript for submission.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare no conflicts of interest.
Ethical approval
Ethics approval for this retrospective study was granted following review by the Northern Sydney Local Health District Human Research Ethics Committee (NSLHD HREC Reference Number NSPHEC 2014-LNR-006).
Informed consent
For this type of study formal consent is not required.
Additional information
Investigation performed at the Sydney Orthopaedic Research Institute, Sydney, Australia.
Rights and permissions
About this article
Cite this article
Wong, E., Nguyen, C.L., Park, S. et al. Simultaneous, same-anaesthetic bilateral total knee arthroplasty has low mortality and complication rates. Knee Surg Sports Traumatol Arthrosc 26, 3395–3402 (2018). https://doi.org/10.1007/s00167-018-4908-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-018-4908-4