Abstract
Purpose
The optimal coronal alignment is still under debate. However, in most of the studies, alignment was only assessed using radiographs, which are not accurate enough for assessment of tibial and femoral TKA position. The primary purpose of this study was to assess the relationship between coronal TKA alignment using 3D-reconstructed CTs and clinical outcome in patients with preoperative varus in comparison with patients with natural or valgus deformity. It was the hypothesis that neutral limb alignment shows a better outcome after TKA.
Methods
Prospectively collected data of 38 patients were included. The clinical and radiological follow-up was 24 months. The patients were grouped into two groups with regard to their preoperative limb alignment. Group A (varus) consisted of 21 patients with preoperative varus of 3° or more, while group B (non-varus) consisted of 17 patients with neutral (− 3 < 0 > + 3) or valgus alignment (> + 3). For assessment of TKA component position and orientation, 3D-reconstructed CT was used. The measurements of the deviation from the whole limb mechanical axis (HKA angle) and the joint line alignment in the femoral (mLDFA) and the tibial side (MPTA) were assessed in the preoperative leg as well as during follow-up after TKA. For clinical outcome assessment, the Knee Society Score (KSS) was used at 1 and 2 years postoperatively. Correlation between KSS score and each variable was done using a linear and quadratic regression model (p < 0.05).
Results
The mean postoperative HKA angle was − 1.3 (varus) in the varus group and + 1.4 (valgus) in the non-varus group. Overall, significant correlations between the preoperative and postoperative alignments were found. In the preoperatively non-varus group, a highly significant correlation was found between neutral limb alignment (HKA = 0° ± 3°) and higher KSS (r 2 = 0.74, p = 0.00). In the varus group, no correlation was found between the postoperative whole limb alignment and the components’ position in the coronal plane to KSS score.
Conclusion
A significant correlation was found between neutral limb alignment and higher KSS only in patients with preoperative non-varus alignment. The concept of constitutional varus alignment is still under debate. Moreover, it appears that one should aim for a more individualized, alignment target based on the individual knee morphotype.
Level of evidence
Diagnostic study, Level II.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Despite numerous advancements in TKA design and surgical technique a considerable number of patients are still not satisfied after TKA [3, 7, 14, 17, 35]. It is one of the most commonly accepted and well-established principles in TKA that one should aim for a neutral mechanical axis [1, 11, 36]. However, just recently, the importance of a neutral mechanical alignment for TKA implant survival and good functional outcome has been questioned [4, 18, 31, 38]. Based on several studies, it appears that a residual slight mechanical varus alignment does not come along with inferior outcomes in patients with preoperative varus alignment. Moreover, in some studies, patients with a residual varus alignment have even shown superior results [18, 29, 40]. Hence, some authors speculated that a neutral mechanical alignment might not be the most important factor for every patient undergoing TKA [31, 36]. Recently, the concept of constitutional varus has been proposed. It was found that a considerable number of osteoarthritic knees do not have a neutral mechanical alignment, but a varus of 3° or more [4]. In another landmark study, patients undergoing TKA with preoperative varus deformity had a better clinical and functional outcome when the alignment was left in mild varus [40]. However, in most of the studies discussed above, the alignment was only assessed using radiographs, which are not accurate enough for assessment of tibial and femoral TKA position [33]. Radiographs have shown a low accuracy and reliability which is due to variation in limb rotation, knee extension deficit, patient positioning, or magnification factors [15, 37]. Assessment of coronal TKA position should be done using 3D reconstructed CT as it is highly reliable. 3D-CT is considered as gold standard for assessment of TKA component position [13, 15].
The primary purpose of this study was to assess the relationship between coronal TKA alignment using 3D-reconstructed CTs and clinical outcome in patients with preoperative varus in comparison with patients with natural or valgus alignment. It was the hypothesis that neutral limb alignment shows a better outcome after TKA.
Materials and Methods
Prospectively collected data of 51 consecutive patients who underwent 3D reconstructed CT scans before and after primary TKA (Depuy, Synthes, PFC Sigma CR and PS, Warsaw, USA) was reviewed. Patients who previously underwent any ipsilateral bony knee procedure prior to TKA (n = 13) were excluded. Finally, 38 patients were included. The clinical and radiological follow-up was 24 months. The patients were grouped into two groups with regard to their preoperative limb alignment. Group A (varus) consisted of 21 patients with preoperative varus of 3° or more, while group B (non-varus) consisted of 17 patients with neutral (− 3 < 0 > + 3) or valgus alignment (> + 3) (Table 1). The patients in the preoperative varus group were younger (mean 65 ± 10 years, median 64, range 45–83 years) than in the non-varus group (mean 71 ± 7 years, median 71, range 59–85 years).
All patients underwent clinical and radiological examination including standardized radiographs (anteroposterior and lateral weight-bearing, patellar skyline view) and CT before TKA and at 1 and 2 years postoperatively.
For assessment of TKA component position and orientation, 3D reconstructed CT was used. The examination was performed using a hybrid system (Symbia T16; Siemens, Erlangen, Germany), which consists of an integrated full diagnostic CT with 16 × 0.75-mm collimation. The CT protocol was modified according to the Imperial Knee Protocol, which is a low-dose CT protocol that includes high-resolution 0.75-mm slices of the knee and 3-mm slices of the hip and ankle joints [12]. The protocol minimizes radiation exposure by scanning only the relevant regions and only the primary joint of interest is scanned in high resolution. In addition, the protocol includes an “extended scale” feature, which enables the software to extract high-quality surface information from the implant by minimizing the effect of the metal artifacts [12].
The measurements of the deviation from the whole limb mechanical axis (HKA angle) and the joint line alignment in the femoral (mLDFA) and the tibial side (MPTA) were assessed by an experienced musculoskeletal radiologist, using a customized software (Orthoexpert v1.15©, OrthoImagingSolutions Ltd., London, UK) in the native preoperative leg as well as during the follow-up after TKA [41] (Figs. 1, 2). The coronal (varus–valgus) alignment was determined with reference to the mechanical axis, according to different anatomical landmarks which have been previously proven to be available and reliable [34]. The 3D-CT scans were corrected with regard to anatomical frames of reference for the patient position in the scanner to reduce to errors caused by variation in the limb rotation. The mechanical axis of the femur was defined as the axis from the center of the femoral head to the center of the knee (the midpoint of the transepicondylar line). The mechanical axis of the tibia was defined as the axis between center of the tibial plateau (or distal to the implant) and the talus center while identifying the most posterior point on the medial and lateral condyle for a precise results in the coronal axis [41]. The femoral joint line coronal alignment (mLDFA) was measured as the angle between a line connecting the components’ distal condyles and a line perpendicular to the mechanical axis. The tibial joint line coronal alignment (MPTA) was measured as the angle between the horizontal face of tibia plateau or the TKA component and a line perpendicular to the mechanical axis.
For clinical outcome assessment, the Knee Society Score (KSS) was used at 1 and 2 years postoperatively. The KSS consists of two parts: a knee score, which rates the knee in terms of pain, range of movement, and stability, and a function score, which rates the ability of the patient to walk, the use of ambulatory aids, and the ability to climb stairs [22]. In the current study, the total score, which were recorded in close proximity to the performed CT, was included for the correlation analysis.
Ethical approval was obtained from the local ethical committee (EKNZ 2015-448). All procedures performed were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Statistical analysis
Mean, median, standard deviations (SD), and range were calculated for the patients’ age at TKA, the KSS scores, the components’ position in the coronal plane, and for the HKA angles. The correlation between the KSS score and each variable was done using a linear and quadratic regression model. The quadratic regression model is able to test the hypothesis that outlier of TKA component alignment correlate with lower KSS values. Pearson correlations were done for correlations between alignment and outcomes. A post hoc analysis using G*Power, version 3.1.9 (University of Kiel, Germany) showed a sufficient sample size. All data were analysed by an independent professional statistician using SPSS version 13.0 (SPSS, Chicago, IL, USA.) P values were two-sided and considered statistically significant if smaller than 0.05.
Results
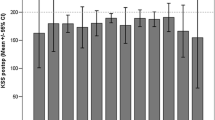
The mean postoperative HKA angle was − 1.3 ± 2.5 (varus) in the varus group and + 1.4 ± 2.9 (valgus) in the non-varus group. A complete description of pre- and postoperative alignment measurement is shown in Table 2. Overall, significant correlations between the preoperative and postoperative alignments were found (Pearson correlation coefficient 0.52, p < 0.001, Fig. 3). No significant differences were found between the groups regarding the total KSS score, as well as the knee and functional sub-scores, after 1- and 2-year follow-up. In the non-varus group, a significant correlation, using a quadratic regression model, was found between neutral limb alignment (HKA = 0° ± 3°) and higher KSS (r 2 = 0.74, p = 0.00) (Fig. 4). In the varus group, no correlation was found between the postoperative whole limb alignment or TKA components’ position in the coronal plane and KSS score.
Discussion
The most important finding of this study is that a significant correlation between neutral postoperative TKA mechanical alignment and better clinical outcomes was found only in patients with preoperative non-varus alignment. This finding corresponds well with the classical alignment target in TKA and with the dichotomous division between “inliers” and “outliers”, i.e., patients with more then 3° deviation from the neutral position had better functional results [2, 5, 8, 25]. However, there is ongoing controversy about the optimal TKA alignment for patient satisfaction and implant survivorship [6, 31, 38]. One of the main issues regarding the optimal TKA alignment is the conflict which exists between the fundamentals TKA laboratory studies and the vast clinical experience which supports natural aliment target, mainly due to the equal load distribution, and the recent literature reports regarding no correlation between neutral mechanical alignment and functional outcomes [20, 29, 30]. Moreover, although two large recent studies, by Parratte et al. [31] and Bonner et al. [6], with long-term mean follow-up (15 and 9.8 years, respectively), using long leg radiographs showed no higher survival in knees with neutral mechanical alignment (0° ± 3°) when compared to an outlier group (> 3°), no recommendation for changing the TKA neutral alignment target was proposed. However, these studies raised the hypothesis that given the complex, multidimensional forces around the knee joint, it seems reasonable to postulate that for any given patient there may be a specific target value for postoperative alignment. The numerous different morphotypes of the knee should be better characterised. Only then, an optimal alignment target for each patient could be identified.
Our findings clearly demonstrated that the influence of the postoperative alignment on the functional outcome is dependent on the preoperative alignment. The relationship between the preoperative and postoperative alignment for the success of TKA might be an important part in the understanding of the ideal, more individualized, alignment target. One explanation for this hypothesis can be found in the cadaveric study by Delport et al. [10] as the strains in the collateral ligaments closely resembled the preoperative pattern of the native knee specimens when constitutional alignment was restored. As the soft-tissue tension is important for providing neurosensory feedback, taking into consideration the preoperative alignment might influence the patients’ satisfaction [16, 23].
Second, no correlation was found between postoperative varus alignment and better clinical outcomes in patients with preoperative varus alignment. These findings contradict the previous studies which argued that patients with preoperative varus might need different alignment target and that restoring the mechanical axis to mild varus might lead to better results in this subgroup [40]. The debate on the effect of the postoperative varus on the patient satisfaction is especially important given that it is long considered to be devastating in terms of implant survival [21, 26]. Recent studies suggested that there might be a conflict of interest between patient satisfaction and implant survivorship [39, 40]. In the basic science studies, overall varus alignment or tibia varus positioning was associated with increased stress in the medial compartment and increased wear of polyethylene inlay [9, 19, 28, 32]. While most studies found no correlation of patient satisfaction with long leg alignment measured on long leg radiographs, Vanlommel et al. [40] showed superior clinical outcome when restoring the overall mechanical axis to 3°–6° varus. However, only patients with preoperative varus of more then 3° were included. The author’s explanation was that at least part of those patients had a prearthritic “constitutional varus” and undercorrection to this approximate alignment could be a more physiological option. In our work, these findings were not confirmed. Using 3D-CT scans pre- and postoperatively it was found no correlation between the postoperative overall alignment, as well as TKA component position with patients’ satisfaction during 2 years of follow-up. Based on our findings and current evidence, the concept of constitutional varus alignment is still not proven and it is not recommended to aim for varus alignment in patients with preoperative varus patients [18, 20, 27].
Finally, it was shown that although the pre- and postoperative whole limb alignments were significantly different between the groups, no difference in KSS scores was found. This finding is in agreement with previous findings [24, 40]. The preoperative alignment correlated with the postoperative alignment, i.e., more varus knees were corrected into varus and more valgus knees into valgus, although the target was neutral mechanical axis in all the cases. Hence, during TKA surgery, the surgeon tends to slightly undercorrect the knee, probably to avoid excessive alteration of soft-tissue tension.
The present study bears a number of limitations to be considered. The major limitation is the relatively small number of patients included. Moreover, as only few patients had low KSS scores, the correlation that was found in the non-varus group was based on few isolated cases. Larger case series are defiantly needed to clarify the relationship between the preoperative limb alignment and the patients’ satisfaction rate.
The clinical relevance of the current article is represented by the fact that, this is the first study, which tested the relationship between the preoperative and postoperative coronal alignment and the patients’ satisfaction using 3D-CT scan.
Conclusion
A significant correlation was found between neutral limb alignment and higher KSS only in patients with preoperative non-varus alignment. The concept of constitutional varus alignment is still under debate. Moreover, it appears that one should aim for a more individualized, alignment target based on the knee morphotype.
References
Abdel MP, Oussedik S, Parratte S, Lustig S, Haddad FS (2014) Coronal alignment in total knee replacement: historical review, contemporary analysis, and future direction. Bone Jt J 96–B:857–862
Anderl W, Pauzenberger L, Kölblinger R, Kiesselbach G, Brandl G, Laky B, Kriegleder B, Heuberer P, Schwameis E (2016) Patient-specific instrumentation improved mechanical alignment, while early clinical outcome was comparable to conventional instrumentation in TKA. Knee Surg Sports Traumatol Arthrosc 24:102–111
Becker R, Döring C, Denecke A, Brosz M (2011) Expectation, satisfaction and clinical outcome of patients after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 19:1433–1441
Bellemans J, Colyn W, Vandenneucker H, Victor J (2012) The Chitranjan Ranawat award: is neutral mechanical alignment normal for all patients? The concept of constitutional varus. Clin Orthop Relat Res 470:45–53
Blakeney WG, Khan RJK, Palmer JL (2014) Functional outcomes following total knee arthroplasty: a randomised trial comparing computer-assisted surgery with conventional techniques. Knee 21:364–368
Bonner TJ, Eardley WG, Patterson P, Gregg PJ (2011) The effect of post-operative mechanical axis alignment on the survival of primary total knee replacements after a follow-up of 15 years. J Bone Jt Surg Br 93:1217–1222
Bourne RB, Chesworth BM, Davis AM, Mahomed NN, Charron KDJ (2010) Patient Satisfaction after Total Knee Arthroplasty: Who is Satisfied and Who is Not? Clin Orthop Relat Res 468:57–63
Choong PF, Dowsey MM, Stoney JD (2016) Does accurate anatomical alignment result in better function and quality of life? Comparing conventional and computer-assisted total knee arthroplasty. J Arthroplast 24:560–569
D’Lima DD, Chen PC, Colwell CWJ (2001) Polyethylene contact stresses, articular congruity, and knee alignment. Clin Orthop Relat Res 392:232–238
Delport H, Labey L, Innocenti B, De Corte R, Vander Sloten J, Bellemans J (2014) Restoration of constitutional alignment in TKA leads to more physiological strains in the collateral ligaments. Knee Surg Sports Traumatol Arthrosc 23:2159–2169
Gromov K, Korchi M, Thomsen MG, Husted H, Troelsen A (2014) What is the optimal alignment of the tibial and femoral components in knee arthroplasty? Acta Orthop 85:480–487
Henckel J, Richards R, Lozhkin K, Harris S, Rodriguez y Baena FM, Barrett AR, Cobb JP (2006) Very low-dose computed tomography for planning and outcome measurement in knee replacement. The imperial knee protocol. J Bone Jt Surg Br 88:1513–1518
Hirschmann MT, Amsler F, Rasch H (2015) Clinical value of SPECT/CT in the painful total knee arthroplasty (TKA): a prospective study in a consecutive series of 100 TKA. Eur J Nucl Med Mol Imaging 42:1869–1882
Hirschmann MT, Iranpour F, Konala P, Kerner A, Rasch H, Cobb JP, Friederich NF (2010) A novel standardized algorithm for evaluating patients with painful total knee arthroplasty using combined single photon emission tomography and conventional computerized tomography. Knee Surg Sports Traumatol Arthrosc 18:939–944
Hirschmann MT, Konala P, Amsler F, Iranpour F, Friederich NF, Cobb JP (2011) The position and orientation of total knee replacement components: a comparison of conventional radiographs, transverse 2D-CT slices and 3D-CT reconstruction. J Bone Jt Surg Br 93:629–633
Hirschmann MT, Müller W (2015) Complex function of the knee joint: the current understanding of the knee. Knee Surg Sports Traumatol Arthrosc 23:2780–2788
Hirschmann MT, Testa E, Amsler F, Friederich NF (2013) The unhappy total knee arthroplasty (TKA) patient: Higher WOMAC and lower KSS in depressed patients prior and after TKA. Knee Surg Sports Traumatol Arthrosc 21:2405–2411
Howell SM, Howell SJ, Kuznik KT, Cohen J, Hull ML (2013) Does a kinematically aligned total knee arthroplasty restore function without failure regardless of alignment category? Clin Orthop Relat Res 471:1000–1007
Hsu HP, Garg A, Walker PS, Spector M, Ewald FC (1989) Effect of knee component alignment on tibial load distribution with clinical correlation. Clin Orthop Relat Res 248:135–144
Huijbregts HJTAM, Khan RJK, Fick DP, Jarrett OM, Haebich S (2016) Prosthetic alignment after total knee replacement is not associated with dissatisfaction or change in Oxford Knee Score. Knee 23:535–539
Insall JN, Binazzi R, Soudry M, Mestriner LA (1985) Total knee arthroplasty. Clin Orthop Relat Res 192:13–22
Insall JN, Dorr LD, Scott RD, Scott WN (1989) Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res 248:13–14
Kuster M, Bistschnau B, Votruba T (2004) Influence of collateral ligament laxity on patient satisfaction after total knee arthroplasty : a comparative bilateral study. Arch Orthop Trauma Surg 124:415–417
Lee B-S, Lee S-J, Kim J-M, Lee D-H, Cha E-J, Bin S-I (2011) No impact of severe varus deformity on clinical outcome after posterior stabilized total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 19:960–966
Longstaff LM, Sloan K, Stamp N, Scaddan M, Beaver R (2009) Good alignment after total knee arthroplasty leads to faster rehabilitation and better function. J Arthroplast 24:570–578
Lotke PA, Ecker ML (1977) Influence of positioning of prosthesis in total knee replacement. J Bone Jt Surg Am 59:77–79
Manjunath KS, Gopalakrishna KG, Vineeth G (2015) Evaluation of alignment in total knee arthroplasty: a prospective study. Eur J Orthop Surg Traumatol 25:895–903
Matsuda S, Whiteside LA, White SE (1999) The effect of varus tilt on contact stresses in total knee arthroplasty: a biomechanical study. Orthopedics 22:303–307
Matziolis G, Adam J, Perka C (2010) Varus malalignment has no influence on clinical outcome in midterm follow-up after total knee replacement. Arch Orthop Trauma Surg 130:1487–1491
Mugnai R, Zambianchi F, Digennaro V, Marcovigi A, Tarallo L, Del Giovane C, Catani F (2016) Clinical outcome is not affected by total knee arthroplasty alignment. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-016-4094-1
Parratte S, Pagnano MW, Trousdale RT, Berry DJ (2010) Effect of postoperative mechanical axis alignment on the fifteen-year survival of modern, cemented total knee replacements. J Bone Jt Surg Am 92:2143–2149
Perillo-Marcone A, Barrett DS, Taylor M (2000) The importance of tibial alignment: finite element analysis of tibial malalignment. J Arthroplasty 15:1020–1027
Radtke K, Becher C, Noll Y, Ostermeier S (2010) Effect of limb rotation on radiographic alignment in total knee arthroplasties. Arch Orthop Trauma Surg 130:451–457
Rasch H, Falkowski AL, Forrer F, Henckel J, Hirschmann MT (2013) 4D-SPECT/CT in orthopaedics: a new method of combined quantitative volumetric 3D analysis of SPECT/CT tracer uptake and component position measurements in patients after total knee arthroplasty. Skelet Radiol 42:1215–1223
Scott CEH, Howie CR, MacDonald D, Biant LC (2010) Predicting dissatisfaction following total knee replacement: a prospective study of 1217 patients. J Bone Jt Surg Br 92:1253–1258
Sikorski JM (2008) Alignment in total knee replacement. J Bone Jt Surg Br 90:1121–11277
Skytta ET, Lohman M, Tallroth K, Remes V (2009) Comparison of standard anteroposterior knee and hip-to-ankle radiographs in determining the lower limb and implant alignment after total knee arthroplasty. Scand J Surg 98:250–253
Slevin O, Amsler F, Hirschmann MT (2016) No correlation between coronal alignment of total knee arthroplasty and clinical outcomes: a prospective clinical study using 3D-CT. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-016-4400-y
Vandekerckhove P-J, Lanting B, Bellemans J, Victor J, MacDonald S (2016) The current role of coronal plane alignment in Total Knee Arthroplasty in a preoperative varus aligned population: an evidence based review. Acta Orthop Belg 82:129–142
Vanlommel L, Vanlommel J, Claes S, Bellemans J (2013) Slight undercorrection following total knee arthroplasty results in superior clinical outcomes in varus knees. Knee Surg Sports Traumatol Arthrosc 21:2325–2330
Wagner CR, Hirschmann MT, Beasley RA (2015) Specific orthopaedic imaging analysis software: clinical benefit from TKR revision surgeon. In: Hirschmann MT, Becker R (eds) The unhappy total knee replacement: a comprehensive review and management guide. Springer, Cham, pp 69–83. doi:10.1007/978-3-319-08099-4
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Funding
There was no financial conflict of interest with regards to this study.
Ethical approval
Ethical approval was obtained from the local ethical committee (EKNZ 2015-448). All procedures performed were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Slevin, O., Hirschmann, A., Schiapparelli, F.F. et al. Neutral alignment leads to higher knee society scores after total knee arthroplasty in preoperatively non-varus patients: a prospective clinical study using 3D-CT. Knee Surg Sports Traumatol Arthrosc 26, 1602–1609 (2018). https://doi.org/10.1007/s00167-017-4744-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-017-4744-y