Abstract
Purpose
This study was set up to identify the native trochlear geometry and define its relationship with the rotational landmarks of the distal femur.
Methods
The rotational landmarks of the distal femur were analysed on CT-scans of 281 patients with end-stage knee osteoarthritis.
Results
The anterior trochlear line (ATL) was on average 4.3° (SD 3.3°) internally rotated relative to the surgical transepicondylar axis (sTEA). The ATL was on average 2.1° (SD 3.0°) internally rotated relative to the posterior condylar line (PCL). The relationship between the ATL and the sTEA was statistically different in the different coronal alignment groups (p = 0.004): 3.9° (SD 3.0°) in varus knees, 4.0° (SD 2.9°) in neutral knees and 5.4° (SD 3.8°) in valgus knees. The lateralisation of the trochlea, represented by the distance between the perpendicular to PCL and the perpendicular to the posterior parallel line to the sTEA, was on average 2.2 mm (SD 1.8 mm).
Conclusion
The ATL was on average 4.3° (SD 3.3°) internally rotated relative to the sTEA and 2.1° (SD 3.0°) internally rotated relative to the PCL. The ATL is more externally orientated in varus knees and more internally rotated in valgus knees. The trochlear groove is lateralised by only 2.2 mm when the femoral component is externally rotated.
Level of evidence
III.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The correct alignment of the femoral component in total knee arthroplasty (TKA) is according to most authors parallel to the surgical transepicondylar axis (sTEA) [4, 10, 15, 20, 24]. First of all, its relative external rotation compared to the posterior condylar line (PCL) stabilises the flexion gap and favours patellar tracking [15, 20, 24]. Secondly, the sTEA is considered the functional flexion axis of the knee [4, 10]. Although the sTEA is considered a reliable and reproducible reference axis, the practical use of this axis is limited because it is difficult to localise the sulcus of the medial epicondyle precisely during surgery [14, 28, 30]. Therefore, anatomical references located on the anterior femur were recently introduced. Won et al. proposed the anterior trochlear line (ATL) as an additional reference axis with an internal rotation of 8.0° of the ATL with respect to the sTEA in normal knees of Korean subjects. Ji et al. [14] found an internal rotation of the ATL of 6.1° with respect to the sTEA in female varus knees. Morizane et al. [22] developed a new radiograph with an axial view of the femur to determine the angle between the ATL and the sTEA.
Although TKA has proven to be successful treatment of end-stage knee osteoarthritis, patellofemoral complications remain common after primary TKA [26]. One of the leading causes for these patellofemoral complications is malpositioning of the femoral component [1, 2, 6, 11, 19, 21, 25, 31]. Internal rotation and excessive external rotation of the femoral component are directly related to patellofemoral malfunctioning [6, 20].
The aim of this study was to define the relationship of the ATL to the PCL and sTEA in osteoarthritic knees in males and females with respect to coronal alignment.
The secondary goal was to identify the native trochlear geometry and assess the effect of external rotation on the mediolateral position of the trochlear groove.
It was hypothesised that (1) a relationship exists between the ATL and the sTEA where the ATL is internally rotated relative to the sTEA and that (2) the mediolateral position of the trochlear groove is not altered when applying external rotation of the femoral component.
Materials and methods
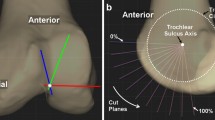
Three hundred and fifty CT-scans (taken on 350 consecutive patients) were performed at the orthopaedic department of UZ Leuven Hospital, Pellenberg, Belgium, from 2009 till 2011. These CT-scans were taken as part of a standard pre-operative protocol in patients with osteoarthritis scheduled for TKA. The CT-scan used was a GE Brightspeed 16 slice CT. The patient was placed in the supine position on the scanning table with the affected leg in full extension. A scout view was obtained. To take scans perpendicular to the long axis of the leg, the scanner’s gantry was tilted based on the lateral scout view. All CT-scans of the knee were performed with a slice thickness of 1 mm. Reconstructions of the axial plane were made in the bone window with a 1:1 ratio without overlap. Thirty-three patients with rheumatoid arthritis and seventeen patients with post-traumatic arthritis were excluded. Nineteen patients where full extention of the knee was not possible were excluded. Two hundred and eighty-one were eventually withheld for further studying as presented in Fig. 1. The average age of the patients was 67.5 years (SD 11.5). One hundred and nineteen patients were males (42.3%), one hundred and sixty-two were females (57.7%). The left knee was involved in 138 cases, the right knee in the remaining 143 cases. On the full limb standing radiograph, the mechanical tibiofemoral angle (mTFA) (angle between the femoral mechanical axis and the tibial mechanical axis) was measured and ranged from 22° of valgus to 23° of varus. The standing long anteroposterior films were obtained under fluoroscopic control with the patella facing the radiographic source. The patients were subdivided into three categories, based on the mTFA. One hundred and fifty-four patients had varus knees with mTFA ≤ 177°, fifty-three patients had neutrally aligned knees with 177° < mTFA < 183° and seventy-four had valgus knees with mTFA ≥ 183°. Each subclass was subdivided according to gender in order to evaluate the variability of the femoral rotational anatomy in relation to gender of the patient. The rotational reference axes were defined as follows: surgical transepicondylar axis (sTEA): the line connecting the tip of the lateral epicondyle with the lowest point of the medial sulcus (more proximal and posterior to the medial epicondyle [16]); posterior condylar line (PCL): the tangent passing through the most posterior part of the medial and lateral femoral condyles; and anterior trochlear line (ATL): the line between the most anterior projections of the lateral and medial femoral condyles [24]. The trochlear anteroposterior axis (TRAx) connects the deepest point of the trochlear groove to the top of the femoral notch with the femur viewed along its mechanical axis. The adequate slice thickness of the CT-scan measurements allowed us to visualise the medial sulcus in all cases. The following angles were defined: posterior condylar angle (PCA) = PCL versus sTEA (Fig. 2a); trochlear angle (TA) = ATL versus sTEA (Fig. 2b); ATL versus PCL (Fig. 2c); and the perpendicular to TRAx versus sTEA (Fig. 2d). The height of the anterior medial and lateral femoral condyles was measured by connecting the most anterior point of the medial and lateral femoral condyles with the line through the deepest point of the trochlear groove, parallel to the sTEA (Fig. 2e). The distance was measured between the line perpendicular to the PCL through the deepest point of the trochlea and the line perpendicular to the posterior parallel line to the sTEA (Fig. 2f). A positive value indicated a more lateral position of the second line in comparison to the line perpendicular to the PCL. Lastly the PCA was measured after TKA using scatter reduction software. The angle between the sTEA and the tangent passing through the most posterior part of the medial and lateral condyles of the femoral component was measured. Internal rotation of the first reference axis relative to the second one was denoted as a positive value. All measurements on the full limb standing radiograph and CT-scan were performed up to one decimal precision (0.1°) three times by the same observer (CV). The intra-observer variability of measuring the mTFA on the full limb standing radiograph was studied on ten samples and gave a SD of 0.7°. The rotational measurements were made on the 2D axial plane images of the CT-scan. The intra-observer variability of finding the anatomical landmarks on 2D axial plane images of the CT-scan was studied on ten samples and was SD 0.4°. IRB approval was attained from the Ethics Committee of the University Hospitals Leuven, ID approval S57326, Contact Ethics Committee via 003216348600 or ec@uzleuven.be.
Measurements performed on the axial images of the CT-scan. a PCL versus sTEA, b ATL versus sTEA, c ATL versus PCL, d perpendicular to TRAx versus sTEA, e height anterior medial and lateral condyles and f lateralisation of trochlea. PCL posterior condylar line, sTEA surgical transepicondylar axis, ATL anterior trochlear line and TRAx trochlear anteroposterior axis
Statistical analysis
A multivariate analysis (ANOVA) was performed to compare the average values of the angles, in relation to the coronal deformity of the knee (varus, neutral and valgus) and the gender of the patient. For every measured value, the β value (slope of the line representing the correlation), the p coefficient and the R 2 were reported. All analyses were performed using StatPlus® 5.8.0.0 (2009 AnalystSoft Inc.).
Results
The mean mTFA was 176.9° (SD 8.2°). The PCL was on average 2.2° (SD 1.8°) internally rotated relative to the sTEA. The ATL was on average 4.3° (SD 3.3°) internally rotated relative to the sTEA. The ATL was on average 2.1° (SD 3.0°) internally rotated relative to the PCL. The lateral condylar height measured on average 8.4 mm (SD 2.0 mm) while the medial condylar height was 5.4 mm (SD 2.0 mm) on average. The lateralisation of the trochlea, represented by the distance between the perpendicular to PCL and the perpendicular to the posterior parallel line to the sTEA, was on average 2.2 mm (SD 1.8 mm). The ┴TRAx was on average 5.5° (SD 2.2°) externally rotated relative to the sTEA. The post-operative PCL was on average 0.5° (SD 2.6°) internally rotated relative to the sTEA.
As presented in Table 1, the relationship between the PCL and the sTEA was statistically different in the different coronal alignment groups (p = 0.015): 1.9° (SD 1.6°) in varus knees, 2.3° (SD 1.9°) in neutral knees and 2.7° (SD 2.3°) in valgus knees. The relationship between the ATL and the sTEA was statistically different in the different coronal alignment groups (p = 0.004): 3.9° (SD 3.0°) in varus knees, 4.0° (SD 2.9°) in neutral knees and 5.4° (SD 3.9°) in valgus knees. The same was true for the lateral condyle height (p = 0.05), the lateralisation of the trochlea (p = 0.001) and the post-operative PCA (p = 0.011).
In order to evaluate the correlation of the measured values with the coronal alignment of the knee, a linear regression test was performed. For every measured value, the β value (slope of the line representing the correlation), the p coefficient and the R 2 were obtained. P values were two sided and considered significant if smaller than 0.05. Statistical analysis revealed a significant relationship between the coronal alignment and the ATL versus sTEA (p < 0.001) (R = 0.23) (Fig. 3).
The same was true for the PCL versus sTEA (p < 0.001) (R = 0.2), ATL versus PCL (p = 0.044) (R = 0.12), lateral condyle height (p = 0.036) (R = 0.13), lateralisation of the trochlea (p < 0.001) (R = 0.23) and PCA after TKA (p = 0.006) (R = 0.17). There was no correlation between the different coronal alignment groups for the height of the medial condyl and the perpendicular to TRAx versus sTEA.
Statistical difference of measured values and angles between varus, valgus and neutral male knees, between males and female knees and between varus, valgus and neutral female knees is presented in Table 2. There was a statistical difference between males and females for the lateral condyle height: females had a significant smaller lateral condyle height in varus knees (p < 0.001), in neutral knees (p < 0.001) and valgus knees (p = 0.013).
There was a statistical difference between males with varus and valgus deformity: varus knees had less internally rotated PCL versus sTEA (p = 0.005), less internally rotated ATL versus sTEA (p = 0.001) and less internally rotated post-operative PCA (p = 0.003).
There was a statistical difference between the three coronal alignment groups in female knees: varus knees had significant smaller lateral condyle height than valgus knees (p = 0.046), varus knees had significant higher lateral condyle height than neutral knees (p = 0.046) and neutral knees had significant smaller lateral condyle height than valgus knees (p = 0.003).
Discussion
The most important finding of this study was that the native trochlear geometry resembled the orientation of the posterior condyles in osteoarthritic knees. This was proven by two measured values. First of all, the ATL was found to be internally rotated compared to the sTEA. The mean ATL in this series was 4.3° (SD 3.3°) internally rotated relative to the sTEA. Secondly, the relationship between the ATL and the sTEA was statistically different in the different coronal alignment groups. In varus knees, the trochlea is more externally rotated, in valgus knees the trochlea is more internally rotated. Luyckx et al. [18] found a similar relationship between the PCL and sTEA in osteoarthritic knees according to coronal alignment. Aside from the ATL, previous studies proposed the trochlear groove as an additional rotational landmark by stating that the native femoral sulcus could be used as a guide for the femoral component position in TKA surgery [8, 9, 27, 28]. Recently, Huang et al. [13] confirmed this role of the native femoral sulcus in patients with severe osteoarthritis. In addition, Talbot et al. [28] reported that the sulcus line of the trochlear groove is more accurate than Whiteside’s line in determining femoral component rotation. More recently, Talbot et al. [27] described an intraoperative trochlear alignment guide to remove intraoperative parallax errors and improve femoral component rotation in total knee arthroplasty. The secondary goal of this study was to analyse the effect on the mediolateral position of the trochlear groove, when the femoral component is externally rotated. In the past, the importance of this external rotation to obtain a rectangular flexion gap has been frequently emphasised. Bellemans et al. reported that a relevant proportion of the physiologically normal human population has a natural limb alignment of 3° varus or more. The greatest contributor of this constitutional varus is the natural varus orientation of the tibia [5]. Therefore, when the tibial cut is done perpendicularly on the mechanical axis of the tibia, an external rotation of 3° is applied to obtain a rectangular flexion gap. Moreover, this external rotation was said to lateralise the trochlear groove and improve patellar tracking [1, 2]. However, in this series an average lateralisation of the trochlear groove of only 2.2 mm (SD 1.8 mm) was found when the implant was externally rotated parallel to the sTEA. These two findings have implications on TKA surgery. First of all, the native trochlear orientation can help the surgeon to assess the femoral component alignment in concordance with the PCL. Secondly, the mediolateral position of the trochlea is not disturbed by applying external rotation of the femoral component during TKA surgery. There are several studies that discuss the different rotational anatomy between males and females. For instance, Berger et al. [7] found a PCA of 3.5° in males and 0.3° in females. In our series, there was a no statistical difference between males and females for the PCA. However, the females had a significant smaller lateral condyle height in varus knees (p < 0.001), in neutral knees (p < 0.001) and valgus knees (p = 0.013) compared to the males. This was also true for the medial condyle height for varus knees (p = 0.001) and neutral knees (p = 0.003). Li et al. [17] described similar findings with a smaller anterior lateral and medial condyle height as well a smaller anterior condyle width of females compared to males. No other statistical different values were observed between males and females. Aside from the PCL and sTEA, the TRAx is also a known and popular reference axis [3, 29]. A mean perpendicular to TRAx versus sTEA of 5.5° (SD 2.2°) was found which is comparable to findings by Luyckx et al. [18] in osteoarthritic knees with a value of 4.8°. The post-operative PCA in our series was on average 0.5° (SD 2.6°) in external rotation relative to the sTEA. This can be attributed to the fact that in our institution the femoral component is aligned with the pre-operative sTEA measured on axial CT-scans. This study has several limitations. First of all, the measurements were performed on CT-scans of osteoarthritic (OA) knees. The degree of OA or the cartilage and bone loss on the posterior condyles was not taken into account. However, Nam et al. [23] showed that the cartilage loss on the posterior condyles in the OA knee is minimal in most cases. Secondly, the rotational measurements were made on 2D axial images of the CT-scan, whereas the sTEA and the trochlea are 3D structures [12]. The bias introduced by this dimensional reduction was minimised by making the CT-scans perpendicular to the long axis of the limb. Nevertheless, 2D images remain inferior to 3D reconstructions in measuring rotational alignment.
Conclusion
The ATL was on average 4.3° (SD 3.3°) internally rotated relative to the sTEA. The ATL was on average 2.1° (SD 3.0°) internally rotated relative to the PCL. The orientation of the anterior trochlea follows the orientation of the posterior condyles in osteoarthritic knees. The ATL is more externally orientated in varus knees and more internally rotated in valgus knees. The trochlear groove is lateralised by only 2.2 mm when the femoral component is externally rotated.
References
Akagi M, Matsusue Y, Mata T, Asada Y, Horiguchi M, Iida H, Nakamura T (1999) Effect of rotational alignment on patellar tracking in total knee arthroplasty. Clin Orthop Relat Res 360:155–163
Anouchi YS, Whiteside LA, Kaiser AD, Millian MT (1993) The effects of axial rotational alignment of the femoral component on knee stability and patellar tracking in total knee arthroplasty demonstrated on autopsy specimens. Clin Orthop Relat Res 287:170–177
Arima J, Whiteside LA, McCarthy DS, White SE (1995) Femoral rotational alignment, based on the anteroposterior axis, in total knee arthroplasty in a valgus knee. A technical note. J Bone Joint Surg Am 77:1331–1334
Asano T, Akagi M, Nakamura T (2005) The functional flexion-extension axis of the knee corresponds to the surgical epicondylar axis. J Arthroplast 20:1060–1067
Bellemans J, Colyn W, Vandenneucker H, Victor J (2012) Is neutral mechanical alignment normal for all patients? The concept of constitutional varus. Clin Orthop Relat Res 470:45–53
Berger RA, Crossett LS, Jacobs JJ, Rubash HE (1998) Malrotation causing patellofemoral complications after total knee arthroplasty. Clin Orthop Relat Res 356:144–153
Berger RA, Rubash HE, Seel MJ, Thompson WH, Crossett LS (1993) Determining the rotational alignment of the femoral component in total knee arthroplasty using the epicondylar axis. Clin Orthop Relat Res 286:40–47
Chiu FY (2006) The native femoral sulcus as the guide for the medial/lateral position of the femoral component in knee arthroplasty: normal patellar tracking in 690/700 knees—a prospective evaluation. Acta Orthop 77:501–504
Chiu FY (2006) Native femoral sulcus as a guide for the position of the femoral component in primary total knee arthroplasty: a prospective comparative study of 420 knees. Knee Surg Sports Traumatol Arthrosc 14:437–442
Churchill DL, Incavo SJ, Johnson CC, Beynnon BD (1998) The transepicondylar axis approximates the optimal flexion axis of the knee. Clin Orthop Relat Res 356:111–118
Fehring TK (2000) Rotational malalignment of the femoral component in total knee arthroplasty. Clin Orthop Relat Res 380:72–79
Hirschmann MT, Konala P, Amsler F, Iranpour F, Friederich NF, Cobb JP (2011) The position and orientation of total knee replacement components: a comparison of conventional radiographs, transverse 2D-CT slices and 3D-CT reconstruction. J Bone Joint Surg Br 93:629–633
Huang G, Xia J, Wang S, Wei Y, Wu J, Chen F, Chen J, Shi J (2016) Total knee arthroplasty using trochlear groove as guide for position of femoral component in severe knee osteoarthritis. BMC Surg 16:33
Ji H-M, Jin DS, Han J, Choo H-S, Won Y-Y (2015) Comparison of alternate references for femoral rotation in female patients undergoing total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 24:2402–2406
Kobayashi H, Akamatsu Y, Kumagai K, Kusayama Y, Ishigatsubo R, Muramatsu S, Saito T (2014) The surgical epicondylar axis is a consistent reference of the distal femur in the coronal and axial planes. Knee Surg Sports Traumatol Arthrosc 22:2947–2953
LaPrade RF, Engebretsen AH, Ly TV, Johansen S, Wentorf FA, Engebretsen L (2007) The anatomy of the medial part of the knee. J Bone Joint Surg Am 89:2000–2010
Li P, Tsai T-Y, Li J-S, Wang S, Zhang Y, Kwon Y-M, Rubash HE, Li G (2014) Gender analysis of the anterior femoral condyle geometry of the knee. Knee 21:529–533
Luyckx T, Zambianchi F, Catani F, Bellemans J, Victor J (2013) Coronal alignment is a predictor of the rotational geometry of the distal femur in the osteo-arthritic knee. Knee Surg Sports Traumatol Arthrosc 21:2331–2337
Matsuda S, Miura H, Nagamine R, Urabe K, Hirata G, Iwamoto Y (2001) Effect of femoral and tibial component position on patellar tracking following total knee arthroplasty: 10-year follow-up of Miller-Galante I knees. Am J Knee Surg U S 14:152–156
Miller MC, Berger RA, Petrella AJ, Karmas A, Rubash HE (2001) Optimizing femoral component rotation in total knee arthroplasty. Clin Orthop Relat Res 392:38–45
Mochizuki RM, Schurman DJ (1979) Patellar complications following total knee arthroplasty. J Bone Joint Surg Am 61:879–883
Morizane K, Takahashi T, Konishi F, Yamamoto H (2011) The anterior trochlear line as a reference for femoral component positioning in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 19:2009–2015
Nam D, Lin KM, Howell SM, Hull ML (2014) Femoral bone and cartilage wear is predictable at 0 degrees and 90 degrees in the osteoarthritic knee treated with total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 22:2975–2981
Poilvache PL, Insall JN, Scuderi GR, Font-Rodriguez DE (1996) Rotational landmarks and sizing of the distal femur in total knee arthroplasty. Clin Orthop Relat Res 331:35–46
Rhoads DD, Noble PC, Reuben JD, Mahoney OM, Tullos HS (1990) The effect of femoral component position on patellar tracking after total knee arthroplasty. Clin Orthop Relat Res 260:43–51
Shervin D, Pratt K, Healey T, Nguyen S, Mihalko W, El-Othmani M, Saleh K (2015) Anterior knee pain following primary total knee arthroplasty. World J Orthop 6:795
Talbot S, Dimitriou P, Mullen M, Bartlett J (2015) Referencing the sulcus line of the trochlear groove and removing intraoperative parallax errors improve femoral component rotation in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-015-3668-7
Talbot S, Dimitriou P, Radic R, Zordan R, Bartlett J (2014) The sulcus line of the trochlear groove is more accurate than Whiteside’s Line in determining femoral component rotation. Knee Surg Sports Traumatol Arthrosc 23:3306–3316
Whiteside LA, Arima J (1995) The anteroposterior axis for femoral rotational alignment in valgus total knee arthroplasty. Clin Orthop Relat Res 321:168–172
Won YY, Cui WQ, Baek MH, Yun TB, Han SH (2007) An additional reference axis for determining rotational alignment of the femoral component in total knee arthroplasty. J Arthroplast 22:1049–1053
Yoshii I, Whiteside LA, White SE, Milliano MT (1991) Influence of prosthetic joint line position on knee kinematics and patellar position. J Arthroplasty 6:169–177
Acknowledgements
Creation of the data was supported in part by Smith and Nephew.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Funding
There was no funding for this study.
Ethical standards
The Ethics Committee of the University Hospitals Leuven acknowledges that this study is carried out according to the prevailing ethical standard. Contact Ethics Committee via 003216348600 or ec@uzleuven.be.
Rights and permissions
About this article
Cite this article
Vercruysse, C., Vandenneucker, H., Bellemans, J. et al. The shape and orientation of the trochlea run more parallel to the posterior condylar line than generally believed. Knee Surg Sports Traumatol Arthrosc 26, 2685–2691 (2018). https://doi.org/10.1007/s00167-017-4685-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-017-4685-5