Abstract
Purpose
The hypothesis of this study is that all-polyethylene (APE) tibial implants offer a biomechanical profile similar to metal-backed tray (MBT). There are significant financial implications, in selected patient groups, if APE can be deemed to perform as well as MBT.
Methods
Using a finite element analysis of CAD models provided by DePuy (Leeds), stress distributions were investigated for both an APE and MBT tibial implant. The performance was assessed for cancellous bone at 700 MPa (normal) and at 350 MPa (less stiff). Plots were recorded along the length of the tibia, showing the loads carried by the bone (cortical and cancellous), the implant interface, cement interface and the stem. von Mises stress distributions and percentage volumes were used to assess bone resorption and hence potential for failure (fracture).
Results
Higher stress shielding (resorption) occurred around the keel and stem of the MBT revealing greater potential for bone loss in these areas. APE had no areas of bone resorption (being more flexible resulting in less stress shielding). The stiffer MBT carries a higher proportion of the load down the stem. MBT stress in cancellous bone is lower than APE, as load is distributed to the cortical rim. APE has a marginally favourable strain state in cancellous bone and spreads loads more at the cement interface than MBT.
Conclusion
Modern-day APE bearings may be superior to previously designed implants due to improvements in manufacturing. In the correct patient group, this could offer substantial cost savings.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
First-generation TKA tibial trays were uniformly APE, but experienced poor results due to aseptic loosening, mostly due to implantation technique [2, 10, 12, 16, 26]. The APE TKA tibial implant was then succeeded by MBT implants to address the loosening issues, with excellent results, offering modularity and intraoperative flexibility [13, 19, 24, 25, 28, 33]. There were, however, issues with MBT locking mechanisms, backside wear and subsequent osteolysis [6, 7, 11, 20, 22].
Significant stress and strain distributions at the implant–bone interface, which vary with quality of the bone and the biomechanical properties of the implant, may lead to loosening, pain, subsidence and subsequent failure of the TKA. Finite element analysis (FEA) studies have assessed the impact of APE and MBT on cancellous bone [9, 17, 21, 31], with higher cancellous bone stresses correlated with increased migration and subsequent poorest survival rates at 5 years [3–5, 31].
Clinical results of APE and MBT have been described in the literature, and studies have shown that MBT can reduce the compressive stress in tibial cancellous bone and dissipate load more uniformly across the proximal tibia, protecting against loosening [3, 17, 31]. However, the manufacturing process of polyethylene has improved considerably. Implant survival has increased, and as such we wish to study the effect on a currently available modern arthroplasty system [1, 8, 18, 19, 23, 27, 32]. The hypothesis of this study is that APE can offer a biomechanical profile similar to MBT and therefore APE can be used in certain patients groups, offering substantial cost savings.
Materials and methods
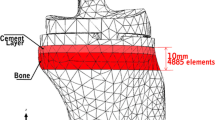
A 3D-cortical shell was created from a single CT scan in multiple planes spaced 0.7 mm apart using Simpleware™, facilitating model creation by using various techniques to retain the pixels covering the relevant part of a left tibia from a healthy 48-year-old male, weighing 105 kg. The cortical shell was then imported as an IGES file into the Finite Element (FE) package ABAQUS (Dassault Systems, Paris, France) for further processing. ABAQUS is a commercial FEA code that can solve complex 3D problems. The model was meshed with a total of 452,761 tetrahedral elements. A mesh convergence study was undertaken to ensure a sufficient number of elements were used.
The proximal tibial condylar surface of the knee joint was then sectioned in ABAQUS leaving an open space in the tibia. The cancellous bone volume was then defined using the inner surface of the imported cortical shell and enclosing the space, forming the cancellous bone volume.
A cement mantle of about 2 mm was then created using the outer surface of the implant stem. This cement part was then used to create the cavity in the cancellous bone for the insertion of the tibial tray. This was done by a Boolean subtraction of the volume of the cement from the cancellous bone stock.
The CAD models of the implant parts, PFC Sigma Posterior Stabilised implant DePuy (Warsaw, Indiana), were provided in IGES formats. The cement mantle, tibial tray and tibial bearing were assembled in their correct positions. The final assemblies of the implanted tibiae (APE and MBT) are shown in Fig. 1.
Two different properties were assessed for the cancellous bone: 700 MPa representing stiff normal bone, whilst 350 MPa representing less stiff bone (such as seen in metabolic bone disorders). A complete summary of the material properties of the bone and implant components is shown in Table 1.
The material properties of the APE (homogenous linear elastic isotropic) were assigned by changing the material properties of the tibial tray part of the model from metal to polyethylene. The two parts (tray and bearing) were tied together in ABAQUS, creating a single polyethylene part. Interfaces between the bone and the cement and between the cement and the implant were also tied in the models.
The tibia was evenly resected, with a tibiofemoral angle of 90° to the long axis of the tibia. The load was applied to the bearing with 50:50 load distributions medially and laterally. The total load applied on the model was chosen to replicate the maximum joint loads experienced during the gait cycle, at contra-lateral toe-off. The gastrocnemius muscle is the only active muscle at this late stance phase of gait. As the gastrocnemius muscle does not attach to any region of the proximal tibia, it was not necessary to include any ligaments or muscles in the models. The effect of the gastrocnemius, however, is represented in the applied joint reaction force. The total load was 2.1 kN which has been used in previous studies in the literature, aiming to represent 2–3 times normal body weight [17, 31].
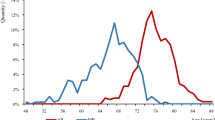
Load plots were generated through the proximal and distal sections of the cancellous bone, cortical bone and tibial tray stem for all models. Von Mises stress distributions for each model (both APE and MBT in both 350 and 700 MPa scenarios) were used to determine areas of bone that may undergo resorption or failure (fracture). A value of 200 με was taken to represent the minimum strain required to maintain bone with <200 με resulting in bone resorption; 10,000 με will lead to bone failure (fracture) and 4000 με was taken to represent an acceptably high strain. Table 2 shows the corresponding stress thresholds set for cancellous bone.
Results
Load transfer
At the implant interface, the underlying cancellous bone in the APE model carried a higher proportion of the load 48 % (700 MPa) and 32 % (350 MPa) than the MBT 26 % (700 MPa) and 17 % (350 MPa).
Implanting the APE and MBT in the less stiff cancellous bone caused the load transfer in the cancellous bone region to be reduced, redistributing load to the cortical rim as shown in Fig. 2.
The gradient of the load transfer plots seen in Fig. 3 reveals a rapid load transfer with the APE, in contrast to the slower load transfer with the MBT. The APE stem carries a significantly lower proportion of the load, as Fig. 4 shows early, rapid load transfer.
The stem of the MBT carries a higher percentage of load than that of the APE. Load transfers in the MBT stem are as high as 28 % (700 MPa) and 25 % (350 MPa) cancellous bone compared to the APE stem, 8 % (350 MPa) and 7 % (700 MPa), respectively.
Von Mises stress
Cancellous bone stress contour plots exhibit differences between MBT and APE in both the 700 and 350 MPa model (Figs. 5, 6). MBT exhibits reduced stresses in the underlying proximal region of cancellous bone resulting in stress shielding, manifested as black areas of resorption (<200 με). APE demonstrates increased stress peripherally (grey areas), and the percentage volume bone above 4000 με was 0.02 % (700 MPa) and 0.21 % (350 MPa). The MBT did not demonstrate values above 4000 με.
As cancellous bone stiffness increases, the stresses in APE encountered were 3.3 MPa (700 MPa) compared to 2.4 MPa (350 MPa). In the MBT the equivalent values were 2.8 MPa (700 MPa) and 2.0 MPa (350 MPa). Figure 2 shows higher loads carried by the cancellous bone by the APE than by the MBT.
The overall percentage bone loss volume (shown black in Figs. 5, 6) was 1.4 % (700 MPa) and 0.4 % (350 MPa) for the MBT. The APE percentage volume bone loss was 0.24 % (700 MPa) and 0 % (350 MPa). Resorption occurred around the MBT keel region, stiffer cancellous bone revealing greater potential for bone loss.
Shear stresses were concentrated in the periphery of the proximal cement layer (facing the tray), in the MBT, load transferred from the (stiff) metal tray to the cortical bone (Fig. 7). APE exhibits a more uniform distribution of shear stresses due to the more flexible tray spreading the load over the resected surface. Two inward shear stress peaks (of opposing signs) can be seen on both the lateral and medial sides on the APE upper cement layer, due to axial compressive stress (not seen on the MBT). Shear stresses on the distal side of the cement layer (facing the resected bone surface) show that the shear stress peaks are found peripherally, adjacent to the cortical bone.
The maximum shear stresses in the cement are marginally higher on the distal side and are marginally higher for the MBT (2.6 and 3.2 MPa) than for the APE (2.3 and 3.0 MPa) for 700 and 350 MPa cancellous bone, respectively. The stresses in all components are considerably lower than the cement shear fatigue endurance limit of 5 MPa.
Maximum compressive cement stresses were located peripherally on the distal cement face (facing the resected bone); unlike the shear stresses, the maximum compressive stresses were marginally higher for the APE (7.5 and 8.5 MPa) than for the MBT (6.5 and 5.5 MPa) for 700 and 350 MPa cancellous bone, respectively. The maximum compressive stresses in both the APE and MBT cement were lower than the compressive fatigue endurance limits of 17 MPa.
Discussion
The most important finding of this study was increase in potential bone loss due to resorption around the MBT stem and keel, when compared to APE in the cancellous region of the proximal tibia.
It has been the hypothesis of previous studies that APE suffers with excessive stresses in the proximal tibia and that this may cause prosthesis migration and subsequent cancellous bone failure. Historically, early failures were also due to mal-alignment. Previous studies using FEA, unsurprisingly, showed that the location and magnitude of loading are significantly altered by component alignment—combined effects of >3° varus of the tibial component and higher body mass indexes are associated with increased medial component loading and failure [30]. Implant failures could also be linked to component design and geometry, with better coronal conformity being an issue addressed [14, 15].
It has been shown here that implanting an all-polyethylene implant into the proximal tibia caused increased load transfer and increased stresses on the underlying cancellous bone, evidenced by the generated load plots. Load transfers of 48 % (700 MPa) and 32 % (350 MPa) were encountered in APE, whilst only 26 % (700 MPa) and 17 % (350 MPa) in MBT. Increased APE cancellous stresses were not so high as to overload the bone, but would have the effect of reducing the stress shielding that might occur in the MBT.
APE causes the load to be transferred to the stiffer cancellous regions surrounding the polyethylene stem, the stem not carrying much of the load, with less stiff bone directing more load through the stem. The stiffer MBT will not allow the load to be dissipated through the surrounding cancellous bone, and it will carry a higher proportion of the load in the stem. The stiffer cancellous bone also causes less load to be transferred into the cortical bone, Fig. 4, the additional load being carried by the stem.
Von Mises stresses of 2.46 MPa were present in the cancellous bone for the all-polyethylene implant, whilst stresses of up 2.0 MPa were present for the metal tray for the 350 MPa cancellous bone. This has been reflected in other similar studies, reporting peak cancellous bone stresses of 7.95 MPa for APE compared to 2.59 MPa for the MBT [9, 14, 15, 17, 18, 21, 29–31]. These stresses are insufficient to overload the bone.
Cement stresses in other studies also reported increased compressive stresses at the cement–cancellous bone interface for the all-polyethylene implant. Compressive stresses of 3.5 MPa were found for the all-polyethylene implant and 1.3 MPa for the metal-backed implant [17]. We found that the stresses were significantly below the fatigue endurance limit for the cement.
The main limitation of a study such as this is the material model used for the cancellous bone. It is known that the properties of cancellous bone vary spatially, and this is a level of complexity that has not yet been included in this study. We analyse results using a uniform material, investigating values based on what would be considered a high cancellous modulus and a low cancellous modulus. Further work should explore the use of spatially varying cancellous material properties. Another limitation is bone resorption thresholds used. There are a range of bone resorption models and a range of thresholds within these models. The approach adopted has been to use representative thresholds of the common strain-based resorption model. Changing the model or the threshold might change the predicted quantity of bone resorbed, but the relative effects of MBT and APE are likely to remain the same. A final limitation is the degree of load alignment. In this preliminary study, the load has been assumed to be perfectly aligned. Further studies could be undertaken to assess the degree of loading mal-alignment.
APE and MBT have advantages and disadvantages. Most surgeons will cite a lack of intraoperative flexibility with APE, but when adequate pre-operative planning is carried out identifying cases unsuitable for APE, there may be a significant financial saving to the healthcare economy.
Conclusion
FEA modelling reveals APE transfers more load to the cancellous bone than the MBT and produces higher stresses in the cancellous bone.
MBT exhibits more potential bone loss due to resorption than APE in the cancellous region of the proximal tibia, particularly around the implant stem and keel.
APE produces marginally more favourable strain state in cancellous bone than the MBT and spreads the stresses at the cement interface more than MBT.
References
Adalberth G, Nilsson KG, Byström S, Kolstad K, Milbrink J (2001) All-polyethylene versus metal-backed and stemmed tibial components in cemented total knee arthroplasty. A prospective, randomised RSA study. J Bone Joint Surg Br 83(6):825–831
Apel DM, Tozzi JM, Dorr LD (1991) Clinical comparison of all-polyethylene and metal-backed tibial components in total knee arthroplasty. Clin Orthop Relat Res 273:243–252
Bartel DL, Burstein AH, Santavicca EA et al (1982) Performance of the tibial component in total knee replacement. J Bone Joint Surg Am 64(7):1026–1033
Bourne RB, Finlay JB (1986) The influence of tibial component intramedullary stems and implant-cortex contact on the strain distribution of the proximal tibia following total knee arthroplasty. An in vitro study. Clin Orthop Relat Res 208:95–99
Brihault J, Navacchia A, Pianigiani S, Labey L, De Corte R, Pascale V, Innocenti B (2015) All-polyethylene tibial components generate higher stress and micromotions than metal-backed tibial components in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-015-3630-8
Conditt MA, Stein JA, Noble PC (2004) Factors affecting the severity of backside wear of modular tibial inserts. J Bone Joint Surg Am 86-A(2):305–311
Conditt MA, Thompson MT, Usrey MM, Ismaily SK, Noble PC (2005) Backside wear of polyethylene tibial inserts: mechanism and magnitude of material loss. J Bone Joint Surg Am 87(2):326–331
Cheng T, Pan X, Liu T, Zhang X (2012) Tibial component designs in primary total knee arthroplasty: should we reconsider all-polyethylene component? Knee Surg Sports Traumatol Arthrosc 20(8):1438–1449
Completo A, Fonseca F, Simões JA (2007) Experimental validation of intact and implanted distal femur finite element models. J Biomech 40(11):2467–2476
Ducheyne P, Kagan A 2nd, Lacey JA (1978) Failure of total knee arthroplasty due to loosening and deformation of the tibial component. J Bone Joint Surg Am 60(3):384–391
Engh GA, Dwyer KA, Hanes CK (1992) Polyethylene wear of metal-backed tibial components in total and unicompartmental knee prostheses. J Bone Joint Surg Br 74(1):9–17
Faris PM, Ritter MA, Keating EM, Meding JB, Harty LD (2003) The AGC all-polyethylene tibial component: a ten-year clinical evaluation. J Bone Joint Surg Am 85-A(3):489–493
Font-Rodriguez DE, Scuderi GR, Insall JN (1997) Survivorship of cemented total knee arthroplasty. Clin Orthop Relat Res 345:79–86
Gioe TJ, Sinner P, Mehle S, Ma W, Kileen KK (2007) Excellent survival of all-polyethylene tibial components in a community joint registry. Clin Orthop Relat Res 46:88–92
Gioe TJ, Stroemer ES, Santos ER (2007) All-polyethylene and metal-backed tibias have similar outcomes at 10 years: a randomized level I [corrected] evidence study. Clin Orthop Relat Res 455:212–218 (Erratum in: Clin Orthop Relat Res. 458:249)
Hyldahl H, Regnér L, Carlsson L, Kärrholm J, Weidenhielm L (2005) All-polyethylene vs. metal-backed tibial component in total knee arthroplasty-a randomized RSA study comparing early fixation of horizontally and completely cemented tibial components: part 2. Completely cemented components: MB not superior to AP components. Acta Orthop 76(6):778–784
Lewis JL, Askew MJ, Jaycox DP (1982) A comparative evaluation of tibial component designs of total knee prostheses. J Bone Joint Surg Am 64(1):129–135
Najibi S, Iorio R, Surdam JW, Whang W, Appleby D, Healy WL (2003) All-polyethylene and metal-backed tibial components in total knee arthroplasty: a matched pair analysis of functional outcome. J Arthroplasty 18(7 Suppl 1):9–15
Nouta KA, Verra WC, Pijls BG, Schoones JW, Nelissen RG (2012) All-polyethylene tibial components are equal to metal-backed components: systematic review and meta-regression. Clin Orthop Relat Res 470(12):3549–3559
Parks NL, Engh GA, Topoleski LD, Emperado J (1998) The Coventry Award. Modular tibial insert micromotion. A concern with contemporary knee implants. Clin Orthop Relat Res 356:10–15
Perillo-Marcone A, Ryd L, Johnsson K, Taylor M (2004) A combined RSA and FE study of the implanted proximal tibia: correlation of the post-operative mechanical environment with implant migration. J Biomech 37(8):1205–1213
Rao AR, Engh GA, Collier MB, Lounici S (2002) Tibial interface wear in retrieved total knee components and correlations with modular insert motion. J Bone Joint Surg Am 84-A(10):1849–1855
Ranawat AS, Mohanty SS, Goldsmith SE, Rasquinha VJ, Rodriguez JA, Ranawat CS (2005) Experience with an all-polyethylene total knee arthroplasty in younger, active patients with follow-up from 2 to 11 years. J Arthroplasty 20(7 Suppl 3):7–11
Rand JA, Ilstrup DM (1991) Survivorship analysis of total knee arthroplasty. Cumulative rates of survival of 9200 total knee arthroplasties. J Bone Joint Surg Am 73(3):397–409
Rasquinha VJ, Ranawat CS, Cervieri CL, Rodriguez JA (2006) The press-fit condylar modular total knee system with a posterior cruciate-substituting design. A concise follow-up of a previous report. J Bone Joint Surg Am 88(5):1006–1010
Ritter MA (1994) The cemented all-poly tibia. Orthopaedics 17(9):841
Rodriguez JA, Baez N, Rasquinha V, Ranawat CS (2001) Metal-backed and all-polyethylene tibial components in total knee replacement. Clin Orthop Relat Res 392:174–183
Scuderi GR, Insall JN, Windsor RE, Moran MC (1989) Survivorship of cemented knee replacements. J Bone Joint Surg Br 71(5):798–803
Small SR, Berend ME, Ritter MA, Buckley CA (2010) A comparison in proximal tibial strain between metal-backed and all-polyethylene anatomic graduated component total knee arthroplasty tibial components. J Arthroplasty 25(5):820–825
Taylor M, Tanner KE (1997) Fatigue failure of cancellous bone: a possible cause of implant migration and loosening. J Bone Joint Surg Br 79:181
Taylor M, Tanner KE, Freeman MA (1998) Finite element analysis of the implanted proximal tibia: a relationship between the initial cancellous bone stresses and implant migration. J Biomech 31(4):303–310
Wasielewski RC, Parks N, Williams I, Surprenant H, Collier JP, Engh G (1997) Tibial insert undersurface as a contributing source of polyethylene wear debris. Clin Orthop Relat Res 345:53–59
Windsor RE, Scuderi GR, Moran MC, Insall JN (1989) Mechanisms of failure of the femoral and tibial components in total knee arthroplasty. Clin Orthop Relat Res 248:15–19 (discussion 19–20)
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Thompson, S.M., Yohuno, D., Bradley, W.N. et al. Finite element analysis: a comparison of an all-polyethylene tibial implant and its metal-backed equivalent. Knee Surg Sports Traumatol Arthrosc 24, 2560–2566 (2016). https://doi.org/10.1007/s00167-015-3923-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-015-3923-y