Abstract
Purpose
Surgical repair after acute Achilles tendon rupture leads to lower re-rupture rates than non-surgical treatment. After open repair, early functional rehabilitation improves outcome, but there are risks of infection and poor wound healing. Minimal invasive surgery reduces these risks; however, there are concerns about its stability. Consequently, physicians may have reservations about adopting functional rehabilitation. There is still no consensus about the post-operative treatment after minimal invasive repair. The aim of this study was to define the most effective and safe post-operative rehabilitation protocol following minimal invasive repair.
Methods
A systematic literature search in Embase, MEDLINE and Cochrane Library for prospective trials reporting on early functional rehabilitation after minimal invasive repair was performed. Seven studies were included.
Results
One randomized controlled trail, one prospective comparative and five prospective non-comparative studies were identified. Four studies performed full weight bearing, all demonstrating good functional results, an early return to work/sports and high satisfaction. One study allowed early mobilization leading to excellent subjective and objective results. The only randomized controlled trial performed the most accelerated protocol demonstrating a superior functional outcome and fewer complications after immediate full weight bearing combined with free ankle mobilization. The non-comparative study reported high satisfaction, good functional results and an early return to work/sports following combined treatment.
Conclusion
Immediate weight bearing in a functional brace, together with early mobilization, is safe and has superior outcome following minimally invasive repair of Achilles tendon rupture. Our recommended treatment protocol provides quality assurance for the patient and reliability for the attending physician.
Level of evidence
II.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Following Achilles tendon rupture (ATR), surgical repair leads to reduced rates of re-rupture over non-operative treatment [20, 21]. The re-rupture rates in non-operative treatment can, however, be decreased with the use of accelerated rehabilitation [36]. Minimally invasive and percutaneous surgery has improved cosmesis together with reduced infection and wound complication rates and comparable re-rupture rates to open surgery [30]. This means that minimally invasive surgery is an attractive option. Rates of iatrogenic nerve injury may be slightly higher with percutaneous surgery, but this complication does not affect functional outcome [7, 11, 31].
An ATR causes long-term deficits of reduced calf muscle strength and dysfunction. Patients suffer from functional deficits after 2 years, and only approximately 60 % are able to return to their pre-injury sports level [24, 33]. Following rupture physiotherapy and rehabilitation pathways aim to minimize this dysfunction and optimize return to pre-injury activities. The key components are weight bearing and early but limited range of movement usually within an orthotic device [18, 28].
Following open repair, the benefit of early functional treatment has been consistently documented by several randomized controlled trials and meta-analyses [9, 21, 26, 37]. Specifically, combined functional treatment applying immediate full weight bearing and early but limited ankle movement was found to be superior in regard to patient satisfaction and calf muscle function after open repair [4]. In the most recent RCT, an open technique consisting of two locking Kessler sutures accompanied by a circumferential running suture was performed. Olsson et al. [34] reported no re-ruptures and good functional results followed by accelerated rehabilitation. Although this strong stable repair was performed, post-operatively an orthotic was still used to limit ankle motion for 6 weeks. Biomechanical studies of minimally invasive and percutaneous suture repair configurations show lower tensile strengths potentially encouraging caution with rehabilitation [16, 35]. Surveys of actual practice reveal that treatment algorithms show considerable variation and may be based on individual opinion only [2, 19]. Surgeons may be less confident of applying early accelerated rehabilitation following less stable minimally invasive repairs.
The aim of this study was to provide evidence-based guidance for the components of post-operative rehabilitation following minimally invasive Achilles tendon repair.
Materials and methods
Search strategy
A database search in Embase, MEDLINE and the Cochrane Collaboration Library was performed. Embase and MEDLINE were searched from inception to November 2014 using the words “Achilles”, “tendon”, “rupture” “percutaneous”, “mini-open” and “minimally invasive” using a Boolean AND operator. All English and German articles were included. The Cochrane Library was searched for the text word “Achilles tendon rupture”. Two researchers (MB, HP) independently reviewed all citations based upon title, abstract and finally full text. Again, only articles meeting the PICOS criteria were selected [10]. Additionally, the reference lists of all eligible full text articles were hand-searched to make sure that no relevant studies were missed. Differences were resolved by discussion.
Eligibility criteria
Only studies referring to acute, isolated ruptures of the Achilles tendon were included. “Acute” was defined to be less than 14 days. Minimal invasive repair (either minimally invasive or percutaneous surgery) was defined as intervention. As literature has failed to define the terms minimally invasive and percutaneous consistently, the term “minimally invasive” repair is always used when the rupture zone and apposition of tendon ends are visualized through a small incision over the rupture side. The term “percutaneous” repair is used when the rupture zone is not opened during the operation [7]. All trials using accelerated rehabilitation following minimally invasive or percutaneous repair were identified. Rehabilitation protocols were considered accelerated if they either allowed immediate full weight bearing (starting within the first 2 weeks after the operation), early ankle mobilization (initiated after the second week post-operatively at the latest) or the combination of both. Functional brace or orthotic use was noted but was not a specific inclusion or exclusion criterion. The required outcome parameters were patient satisfaction, a functional assessment, and time to return to work/sports, re-ruptures and other complications. All randomized controlled trials comparing different rehabilitation protocols and all prospective comparative or non-comparative studies were selected. The level of evidence was assessed independently by two of the authors (HP, MB) in accordance with the level-of-evidence rating system introduced by Wright et al. [40]. Disagreements were resolved by discussion.
For a structured approach, the following PICOS criteria were formulated in this review. Patients with an acute isolated ATR were included (P). Minimally invasive or percutaneous repair of the Achilles tendon was selected for intervention (I). Different post-operative treatment protocols were compared (C). Patient satisfaction, functional assessments, time to return to work/sports, re-ruptures and other complications were defined as outcome parameters (O). Only randomized controlled trials (Level I), prospective comparative studies and prospective non-comparative studies (Level II) were included in this review (S).
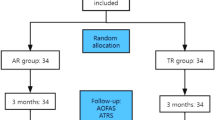
The systematic search identified 558 relevant citations. Out of these, seven trials met the defined inclusion criteria. One randomized controlled trial compared different rehabilitation protocols following percutaneous surgery. The six remaining were either prospective comparative studies (1) or prospective non-comparative studies (5). The detailed results of the literature search are presented in Fig. 1.
Quality assessment
In order to rank the included studies due to their methodological quality, a modified version of the original Coleman Methodology Score (CMS) was used [8]. The score was modified as it was originally intended to assess the outcome of different surgical procedures. By adapting the CMS, it became appropriate to evaluate and compare the methodical quality of the included studies regarding interventions (rehabilitation) other than surgery. An 8-criteria score—instead of the original 10-criteria score—was adopted with a possible maximum of 80 points, indicating a methodologically well-performed study. Two reviewers independently scored each study separately. The particular scoring of each single study is listed in Table 1.
Results
In total, seven trials were included. For a more critical appraisal, the different rehabilitation aspects were divided into full weight bearing (FWB), early mobilization (EM) or the combination of both (CFT) in the following. A detailed description of all included trials is depicted in Table 1.
Full weight bearing (FWB)
One comparative and three non-comparative studies explicitly evaluating the effect of FWB after minimal invasive repair were identified. If not stated differently, FWB means immediate FWB with the ankle immobilized in different positions.
Assal et al. [1] reported the results of 82 patients treated with partial weight bearing increased to FWB within the first two post-operative weeks after minimally invasive repair (Achillon device, non-locking sutures). The mean AOFAS score was 96 points [22]. Calf muscle strength, concentric peak torque and muscle endurance revealed no significant difference between the injured and uninjured leg. After 26 months, all patients had achieved their pre-injury activity level including five elite athletes. Three re-ruptures were reported.
Lansdaal et al. [23] documented the results of 163 patients treated by percutaneous Achilles tendon repair using a non-locking Bunnell suture with trans-calcaneal fixation followed by FWB. Subjectively, 2.5 % suffered from pain, 1.8 % reported abnormal gait and shoe problems, and 0.6 % complained a loss of strength. Fifteen patients reported a sensory loss of the sural nerve. Furthermore, four re-ruptures, three infections, one tendon necrosis and one deep vein thrombosis were reported.
Majewski et al. [27] performed a prospective comparative study using a percutaneous non-locking transverse suture followed by either FWB or NWB. Time to return to work, post-operative sports level and patient satisfaction were significantly improved by FWB. Moreover, FWB led to less pronounced calf atrophy, better heel raise endurance and improved Hannover Achilles Tendon Score [38].
Bhattacharyya and Gerber [3] prospectively compared open repair followed by NWB to minimally invasive repair followed by FWB. In order to improve the comparability of the included studies and to reduce the bias due to confounding variables, only the prospectively evaluated minimally invasive were analysed (n = 25). Patients were operated with the Achillon device. FWB led to low pain levels without wound complication. The majority returned to their pre-injury state after 3 months.
Early ankle mobilization (EM)
One non-comparative study exclusively evaluated the effect of early ankle mobilization. Early mobilization was considered to be free plantar flexion although dorsiflexion was restricted to neutral 0°.
Calder and Saxby [5] followed 46 patients treated with early ankle mobilization allowing free plantar flexion and restricting dorsiflexion at neutral. Minimally invasive repair was performed using the Achillon device. All patients reported high satisfaction levels with a mean AOFAS score of 98 and Achilles Rupture Performance Score (ARPS) of 96 points [24]. Mean time return to work was 22 days, and all patients returned to sports latest after 6 months. No re-rupture occurred.
Combined functional treatment (CFT)
CFT will be considered the combination of FWB and EM. One randomized controlled trail and one prospective non-comparative trial evaluating the effect of CFT were identified.
Guillo et al. reported 23 patients treated with CFT after performing Bunnell and Kessler sutures as described by Carmont and Maffulli [6, 15]. FWB was allowed immediately, and free plantar flexion of the ankle with restriction of dorsiflexion at 0° was allowed after 2 weeks. All patients were satisfied with their treatment resulting in an average Achilles Tendon Total Rupture Score (ATRS) of 84.3 points [32]. After 2 years, 90 % were participating in sports activities, 80 % out of these had returned to their pre-injury sports level. No re-ruptures or persistent sural nerve injuries occurred in this study.
Groetelaers et al. [14] performed the only randomized controlled trial identified comparing different rehabilitation protocols after percutaneous repair. A Bunnell suture proximally and a trans-calcaneal suture distally were used. Patients were treated either by immediate FWB and free EM or by NWB and immobilization in a cast. The median time to return to work was 4 weeks in both groups. For CFT, the time ranged from 0 to 12 weeks and for IM from 1 to 40 weeks. Ninety-six percentage of patients treated with CFT had a good or excellent Achilles Rupture Performance Score compared to 83 % in the IM group. Calf muscle strength and the SF-12 quality of life score showed better results for CFT, although not significant [39]. One re-rupture was reported in each group.
Discussion
The most important finding of this systematic review is that early active rehabilitation, consisting of immediate weight bearing and early motion, is effective and safe following minimally invasive repair of acute ATRs.
Minimally invasive repair techniques give good outcome and have minimal scar formation, infection and re-rupture rates.
Full weight bearing (FWB)
Assal et al. [1] reported no differences between the uninjured and injured leg regarding calf muscle strength and endurance after 2 years of follow-up. All showed excellent results in the AOFAS score. Outcome measurements included various objectified instrumented functional assessments.
Lansdaal et al. [23] followed 163 patients after percutaneous repair over a period of 6 years. This is extraordinary as it marks the largest patient collective and the longest follow-up of all studies included. However, mainly subjective outcome parameters were reported using a modified Leppilahti score without assessing and reporting the calf muscle function as described in the original score.
Majewski et al. [27] reported significant earlier return to work and improved patient satisfaction. Patient-reported outcome scores, the Hannover Achilles Tendon Score and heel rise endurance test were superior with FWB, however not statistically significant. A major limitation for inclusion is that no complications were reported.
Bhattacharyya and Gerber [3] originally performed a prospective comparative study with open surgery followed by NWB on one side and minimally invasive surgery followed by FWB on the other. It is considered that the differing surgical techniques and rehabilitation methods mean that it is difficult to draw a conclusion concerning the rehabilitation protocols alone. For this systematic review, all patients treated by open repair were excluded. The minimally invasive patients reported high satisfaction and a fast return to pre-injury state. Unfortunately, the outcome measurements were subjective parameters only, and re-ruptures were not stated.
In conclusion, immediate FWB leads to superior functional results, early return to pre-injury activity and high patient satisfaction. Furthermore, there was no evidence for increased re-rupture rates. Therefore, the patients should be allowed to bear full weight immediately after the operation.
Early ankle mobilization (EM)
Calder and Saxby [5] demonstrated that early ankle mobilization led to a high patient satisfaction reflected by excellent results in the AOFAS and Leppilahti score. Calder and co-workers reported an early return to work and sports without any re-rupture. Unfortunately, the results of the outcome scores are reported for a follow-up period of 6 months only and did not include a control group.
In conclusion, EM shows excellent subjective and objective outcome without increasing re-rupture risk.
Combined functional treatment (CFT)
Guillo et al. used the post-operative treatment protocol described by Maffulli et al. consisting of immediate FWB and EM after 2 weeks [15, 25]. Unfortunately, the authors then described the rehabilitation protocol differently later in their manuscript placing doubt on the exact treatment. Clinical assessments were performed using a validated and specific score for the Achilles tendon. Functional results were assessed using a dynamometer for calf muscle strength demonstrating significantly decreased values compared to the uninjured side. This study is the only trial available correlating these objective findings to the subjective results. Interestingly, 22 of 23 patients reported that they did not recognize the detected decrease in muscle strength and that this did not interfere with their daily living and sporting activity.
Groetelaers et al. [14] performed the only RCT comparing different rehabilitation protocols after percutaneous repair. This included the most accelerated protocol used in minimally invasive repairs, comparable to open repair. Patients were allowed to FWB combined with free ankle mobilization without any restriction, although a below knee splint was used for the first week following repair. Subsequently rather than an orthosis, an elastic compression sock was applied in the study group compared with a control group with cast immobilization. Moreover, it is the only study evaluating patients’ satisfaction using a well-established quality of life score (SF-12). Upon that, validated outcome measures were used such as the ATRS. CFT improved subjective and functional results, although differences did not reveal statistical significance. The complication rate was considered to be higher due to two deep venous thromboses with immobilization. Re-rupture rate was not increased in the study group.
In conclusion, CFT using immediate FWB and EM results in favourable functional results, early return to pre-injury activities and high satisfaction levels.
Groetelaers et al.’s series is one of the few in which a post-operative orthosis is discontinued early, at 1 week, following surgery. The surgical repair consists of a proximal Bunnell suture anchored distally into the calcaneus through a bone tunnel. This strong suture is comparable to the Pa-bone technique reported by Jielile and Lansdaal [17, 23]. Two other groups report outcomes without using a brace in the post-operative period. Doral used Bunnell sutures in either tendon end, with apposition confirmed by endoscopy [13]. Yotsumoto used “side locking sutures”, effectively a double Kessler suture in coronal and sagittal planes through an open incision [41]. No post-operative cast or brace was used in either study. Whilst patients moved their ankles on the same day of surgery, partial weight bearing was commenced “in the first week following surgery” in Yotsumoto’s study. No complications were reported in this series of 20 patients. Only Doral’s case series used no post-operative protection, with immediate FWB and early movement, making it difficult to draw firm conclusion about safe early mobilization.
One of the potential limitations of this systematic review is that only a small number of papers were identified for inclusion. They consisted of one randomized controlled trial, one prospective comparative and only five prospective trials. The separation due to the three different rehabilitation aspects additionally reduced the numbers of studies for comparison, limiting the conclusions that can be drawn. Furthermore, the comparability of the included trials is complicated as different operative techniques, minimally invasive and percutaneous repairs were performed. The major difference is that the apposition of the tendon ends is visualized directly in minimally invasive repair in contrast to percutaneous repair unless intra-operative endoscopy or ultrasound is used. The absence of apposition, or gaping, may result in an insufficient tendon callus or elongated tendon healing with functional deficits.
Although care must be taken when comparing the outcome of biomechanical studies to in vivo applications, the use of a locking suture resulted in a significantly stronger repair over a box suture [12]. To date there are no clinical comparison studies between the two techniques although early return to play has been reported in case series favouring mini-open repair [29].
Additionally it is worthy of note that in all comparison studies the more progressive rehabilitation protocol provided superior results without increasing the complication rate. The clinical relevance of this study is that immediate weight bearing in a functional brace, together with early mobilization, is safe and has superior outcome following minimally invasive repair of ATR. Cast immobilization to “protect” the repair is not required. More randomized controlled trials are needed to evaluate the effect of even more accelerated protocols to define the limits of progressive rehabilitation—thereby hopefully further improving post-operative results.
Conclusion
Accelerated functional rehabilitation in the early post-operative phase following minimal invasive Achilles tendon repair is superior compared to immobilization. Following repair, immediate full weight bearing in a functional brace or orthosis and early active movement are recommended (Fig. 2).
Abbreviations
- ARPS:
-
Achilles Rupture Performance Score
- ATRS:
-
Achilles Tendon Total Rupture Score
- BKC:
-
Below knee cast
- CFT:
-
Combined functional treatment
- CMS:
-
Coleman Methodology Score
- d:
-
Days
- DF:
-
Dorsiflexion
- DVT:
-
Deep vein thrombosis
- EM:
-
Early mobilization
- FWB:
-
Full weight bearing
- I:
-
Infection
- IM:
-
Immobilization
- m:
-
Months
- NWB:
-
Non-weight bearing
- PF:
-
Plantar flexion
- PWB:
-
Partial weight bearing
- RTS:
-
Return to sports
- RTW:
-
Return to work
- SND:
-
Sural nerve damage
- *:
-
p < 0.01
References
Assal M, Jung M, Stern R, Rippstein P, Delmi M, Hoffmeyer P (2002) Limited open repair of Achilles tendon ruptures: a technique with a new instrument and findings of a prospective multicenter study. J Bone Joint Surg Am 84-A:161–170
Barfod KW, Nielsen F, Helander KN, Mattila VM, Tingby O, Boesen A, Troelsen A (2013) Treatment of acute Achilles tendon rupture in Scandinavia does not adhere to evidence-based guidelines: a cross-sectional questionnaire-based study of 138 departments. J Foot Ankle Surg 52:629–633
Bhattacharyya M, Gerber B (2009) Mini-invasive surgical repair of the Achilles tendon—does it reduce post-operative morbidity? Int Orthop 33:151–156
Brumann M, Baumbach SF, Mutschler W, Polzer H (2014) Accelerated rehabilitation following Achilles tendon repair after acute rupture—development of an evidence-based treatment protocol. Injury 45(11):1782–1790
Calder JDF, Saxby TS (2005) Early, active rehabilitation following mini-open repair of Achilles tendon rupture: a prospective study. Br J Sports Med 39:857–859
Carmont MR, Maffulli N (2008) Modified percutaneous repair of ruptured Achilles tendon. Knee Surg Sports Traumatol Arthrosc 16:199–203
Carmont MR, Rossi R, Scheffler S, Mei-Dan O, Beaufils P (2011) Percutaneous & mini invasive Achilles tendon repair. Sports Med Arthrosc Rehabil Ther Technol 3:28
Coleman BD, Khan KM, Maffulli N, Cook JL, Wark JD (2000) Studies of surgical outcome after patellar tendinopathy: clinical significance of methodological deficiencies and guidelines for future studies. Victorian Institute of Sport Tendon Study Group. Scand J Med Sci Sports 10:2–11
Costa ML, MacMillan K, Halliday D, Chester R, Shepstone L, Robinson AHN, Donell ST (2006) Randomised controlled trials of immediate weight-bearing mobilisation for rupture of the tendo Achillis. J Bone Joint Surg Br 88:69–77
da Costa Santos CM, de Mattos Pimenta CA, Nobre MRC (2007) The PICO strategy for the research question construction and evidence search. Rev Lat Am Enferm 15:508–511
Del Buono A, Volpin A, Maffulli N (2014) Minimally invasive versus open surgery for acute Achilles tendon rupture: a systematic review. Br Med Bull 109:45–54
Demetracopoulos CA, Gilbert SL, Young E, Baxter JR, Deland JT (2014) Limited-open Achilles tendon repair using locking sutures versus nonlocking sutures: an in vitro model. Foot Ankle Int 35:612–618
Doral MN (2013) What is the effect of the early weight-bearing mobilisation without using any support after endoscopy-assisted Achilles tendon repair? Knee Surg Sports Traumatol Arthrosc 21:1378–1384
Groetelaers RPTGC, Janssen L, van der Velden J, Wieland AWJ, Amendt AGFM, Geelen PHJ, Janzing HMJ (2014) Functional treatment or cast immobilization after minimally invasive repair of an acute Achilles tendon rupture: prospective, randomized trial. Foot Ankle Int 35:771–778
Guillo S, Del Buono A, Dias M, Denaro V, Maffulli N (2013) Percutaneous repair of acute ruptures of the tendo Achillis. Surgeon 11:14–19
Hockenbury RT, Johns JC (1990) A biomechanical in vitro comparison of open versus percutaneous repair of tendon Achilles. Foot Ankle 11:67–72
Jielile J, Sabirhazi G, Chen J, Aldyarhan K, Zheyiken J, Zhao Q, Bai J (2012) Novel surgical technique and early kinesiotherapy for acute Achilles tendon rupture. Foot Ankle Int 33:1119–1127
Kearney RS, Costa ML (2012) Current concepts in the rehabilitation of an acute rupture of the tendo Achillis. J Bone Joint Surg Br 94:28–31
Kearney RS, Parsons N, Underwood M, Costa ML (2015) Achilles tendon rupture rehabilitation: a mixed methods investigation of current practice among orthopaedic surgeons in the United Kingdom. Bone Joint Res 4:65–69
Khan RJ, Carey Smith RL (2010) Surgical interventions for treating acute Achilles tendon ruptures. Cochrane Database Syst Rev 9(9):CD003674. doi:10.1002/14651858.CD003674.pub4
Khan RJK, Fick D, Keogh A, Crawford J, Brammar T, Parker M (2005) Treatment of acute achilles tendon ruptures. A meta-analysis of randomized, controlled trials. J Bone Joint Surg Am 87:2202–2210
Kitaoka HB, Alexander IJ, Adelaar RS, Nunley JA, Myerson MS, Sanders M (1994) Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int 15:349–353
Lansdaal JR, Goslings JC, Reichart M, Govaert GAM, van Scherpenzeel KM, Haverlag R, Ponsen KJ (2007) The results of 163 Achilles tendon ruptures treated by a minimally invasive surgical technique and functional aftertreatment. Injury 38:839–844
Leppilahti J, Forsman K, Puranen J, Orava S (1998) Outcome and prognostic factors of achilles rupture repair using a new scoring method. Clin Orthop Relat Res 346:152–161
Maffulli N, Tallon C, Wong J, Lim KP, Bleakney R (2003) Early weightbearing and ankle mobilization after open repair of acute midsubstance tears of the achilles tendon. Am J Sports Med 31:692–700
Maffulli N, Tallon C, Wong J, Peng Lim K, Bleakney R (2003) No adverse effect of early weight bearing following open repair of acute tears of the Achilles tendon. J Sports Med Phys Fitness 43:367–379
Majewski M, Schaeren S, Kohlhaas U, Ochsner PE (2008) Postoperative rehabilitation after percutaneous Achilles tendon repair: early functional therapy versus cast immobilization. Disabil Rehabil 30:1726–1732
Mark-Christensen T, Troelsen A, Kallemose T, Barfod KW (2014) Functional rehabilitation of patients with acute Achilles tendon rupture: a meta-analysis of current evidence. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-014-3180-5
McCullough KA, Shaw CM, Anderson RB (2014) Mini-open repair of achilles rupture in the national football league. J Surg Orthop Adv 23:179–183
McMahon SE, Smith TO, Hing CB (2011) A meta-analysis of randomised controlled trials comparing conventional to minimally invasive approaches for repair of an Achilles tendon rupture. Foot Ankle Surg 17:211–217
Metz R, van der Heijden GJMG, Verleisdonk E-JMM, Kolfschoten N, Verhofstad MHJ, van der Werken C (2011) Effect of complications after minimally invasive surgical repair of acute achilles tendon ruptures: report on 211 cases. Am J Sports Med 39:820–824
Nilsson-Helander K, Thomée R, Silbernagel KG, Grävare-Silbernagel K, Thomeé P, Faxén E, Eriksson BI, Karlsson J (2007) The Achilles tendon Total Rupture Score (ATRS): development and validation. Am J Sports Med 35:421–426
Olsson N, Nilsson-Helander K, Karlsson J, Eriksson BI, Thomée R, Faxén E, Silbernagel KG (2011) Major functional deficits persist 2 years after acute Achilles tendon rupture. Knee Surg Sports Traumatol Arthrosc 19:1385–1393
Olsson N, Silbernagel KG, Eriksson BI, Sansone M, Brorsson A, Nilsson-Helander K, Karlsson J (2013) Stable surgical repair with accelerated rehabilitation versus nonsurgical treatment for acute Achilles tendon ruptures: a randomized controlled study. Am J Sports Med 41:2867–2876
Ortiz C, Wagner E, Mocoçain P, Labarca G, Keller A, Del Buono A, Maffulli N (2012) Biomechanical comparison of four methods of repair of the Achilles tendon: a laboratory study with bovine tendons. J Bone Joint Surg Br 94:663–667
Soroceanu A, Sidhwa F, Aarabi S, Kaufman A, Glazebrook M (2012) Surgical versus nonsurgical treatment of acute Achilles tendon rupture: a meta-analysis of randomized trials. J Bone Joint Surg Am 94:2136–2143
Suchak AA, Bostick GP, Beaupré LA, Durand DC, Jomha NM (2008) The influence of early weight-bearing compared with non-weight-bearing after surgical repair of the Achilles tendon. J Bone Joint Surg Am 90:1876–1883
Thermann H, Zwipp H, Tscherne H (1995) Functional treatment concept of acute rupture of the Achilles tendon. 2 years results of a prospective randomized study. Unfallchirurg 98:21–32
Ware J, Kosinski M, Keller SD (1996) A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care 34:220–233
Wright JG, Swiontkowski MF, Heckman JD (2003) Introducing levels of evidence to the journal. J Bone Joint Surg Am 85-A:1–3
Yotsumoto T, Miyamoto W, Uchio Y (2010) Novel approach to repair of acute achilles tendon rupture: early recovery without postoperative fixation or orthosis. Am J Sports Med 38:287–292
Acknowledgments
We thank Mrs. Maren Hella Thun for the preparation of the figures.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Braunstein, M., Baumbach, S.F., Boecker, W. et al. Development of an accelerated functional rehabilitation protocol following minimal invasive Achilles tendon repair. Knee Surg Sports Traumatol Arthrosc 26, 846–853 (2018). https://doi.org/10.1007/s00167-015-3795-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-015-3795-1