Abstract
Purpose
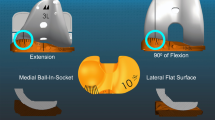
Balancing the posterior cruciate ligament (PCL) with posterior cruciate-retaining total knee replacement (PCR-TKR) aims to restore femoral rollback. In practice, paradoxical roll forward persists. The purpose of this study is to propose a technique for optimizing PCL tension. Because PCL function starts above 60° of flexion, we hypothesize that PCL balancing requires flexion gap tightening by oversizing the femoral component and increasing posterior condylar offset (PCO).
Methods
PCR-TKR was performed in 21 osteoarthritis patients with a gap-balancing technique. The femoral component was oversized if more than a 5-mm posterior drawer existed after tibial component implantation. Kinematics was recorded intra-operatively in two steps with dedicated navigation software (Praxim, La Tronche, Isère, France): antero-posterior (AP) displacements of condylo-tibial contact points were observed in native and implanted knees, with each knee serving as its own control. The absence of paradoxical displacements was verified once the final implants were inserted.
Results
Paradoxical medial condyle displacement (11 mm) persisted in a single case. On average, posterior displacement of the medial condyle decreased from 9 ± 9 to 1 ± 6 mm (p = 0.001) and that of the lateral condyle from 16 ± 14 to 6 ± 6 mm (p = 0.006). In the 0°–30° flexion interval, posterior displacement was 2 times less than before implantation for the medial condyle (p = 0.001), and 4 times less for the lateral condyle (p = 0.004). The course of the lateral condyle decreased from 2 ± 3 to 0 ± 4 mm in the 90°–120° flexion interval (p = 0.046). Six-month flexion was 124° ± 17°.
Conclusion
Femoral component oversizing allows us to control paradoxical forward displacements in 95 % of cases. When balancing PCR prostheses, AP laxity should be taken into account. Increasing PCO appears to be a reliable technique for adjusting PCL balance. Thus, it may optimize extensor mechanism action and, subsequently, the functional results of PCR-TKR.
Level of evidence
Diagnostic study, Level II.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Posterior cruciate-retaining (PCR) total knee replacement (TKR) aims at restoring posterior cruciate ligament (PCL) function. It is usually undertaken according to a conventional technique that involves balance of flexion and extension gaps, to achieve optimal frontal stability. There is growing evidence that this technique alone may not produce adequate PCL tension and appears limited to mobility ranges that are not directly involved in daily activities (normal gait, stair descent). In fact, post-operative kinematic investigations with dual fluoroscopy have revealed that posterior stabilization of the femoral condyles is ineffective in many cases, as shown by persistent paradoxical rolling and erratic axial rotation [5, 19, 20, 22]. Although the clinical consequences are not significant [20], experimental data suggest that extensor apparatus function might be impaired. Mahoney et al. [12] reported that failure to restore PCL tension results in a 15 % decrease of extensor mechanism efficiency in cadaver knees subjected to PCR-TKR. It is why we tried to develop a novel technique for optimizing PCL tension, in an attempt to control antero-posterior (AP) laxities.
PCL balancing might require a tensor to tighten the collateral ligaments at different degrees of flexion, as described by Matsumoto et al. [16] and Fujimoto et al. [6]. Heesterbeek et al. [8] proposed a technique based on the measurement of a step-off distance at 90° of flexion and proposed increased thickness of the tibial spacer in case of loose PCL. We recommend continuous vision with precise measurements of AP displacements of the femoral condyle by dedicated navigation software (Praxim, La Tronche, Isère, France) at some steps of the operation [13, 14]. Flexion gap balancing was previously suggested in deep-dished implants with this software [14], by eventually oversizing the femoral component and subsequently increasing posterior condylar offset (PCO). Although kinematics recorded by the software disclosed that paradoxical displacements still persisted in some patients, this navigation-aided protocol provided new insights into TKR balancing, by taking into account AP laxities as adjunct to the conventional gap-balancing technique. Thus, it was decided to apply the technique to PCR implants, in an attempt at PCL balancing. It was hypothesized that adapting PCL tension would control paradoxical displacements and axial rotation while preserving flexion range. Here, femoral component oversizing was elected because of a persistent posterior drawer after implantation of the trial tibial component. The purpose of this study was to verify a posteriori that paradoxical displacements and/or rotation does not persist after the TKR of definitive trial implants.
Question 1 attempted to validate the PCL-tightening technique in terms of kinematics. Question 2 investigated if a tight PCL restrains motion. That is why we compared test patients with tightened PCL to patients without PCL who had been operated on with deep-dished implants according to the same technique of flexion gap tightening.
Materials and methods
The test population consisted of 21 consecutive patients (February 2011–July 2013), who were scheduled for PCR-TKR, because of painful and disabling primary osteoarthritis (OA), and prospectively selected for operation with a dedicated navigation system displaying, in real time, AP displacements of the condyles on their corresponding tibial plateau (Praxim, La Tronche, Isère, France). Only knees with intact anterior cruciate ligament (ACL) and <10° of varus deformity with no previous surgery were eligible. In fact, pre-implantation kinematics served as personalized references because previous investigations showed that degenerative changes did not significantly alter native kinematics if the ACL was intact [13]. Patients gave informed consent to participate in this special protocol.
The control population consisted of 21 patients who had their PCL excised and their knee stabilized with a deep-dished design of the same prosthesis (September 2010–February 2011). Because the kinematics of deep-dished implants has already been reported in a previous publication [14], the control group served solely to compare flexion ranges. They were selected retrospectively from our database, according to the same inclusion criteria. They were operated on with the same navigation technique that consisted of flexion gap tightening by oversizing the femoral component. Demographic data on the test and control groups were comparable (Table 1).
Operative technique
The same senior surgeon operated on all patients belonging to the test and control groups. The former were implanted with semi-congruent PCR NK2 prosthesis (Hyperflex Natural Knee II, Zimmer, Warsaw, IN, USA) available in a large set of sizes, including narrow configurations (female gender). The latter received the ultracongruent posterior sacrificing (PS) version of the same implant.
Implants were fixed without cement, and the patella was not resurfaced. In the first step of tibial preparation, a posterior slope of 3° was navigated with care taken to superimpose the largest transverse axis with adequate size baseplate (best tibial surface coverage) on the largest transverse axis of the native tibia. Gaps were then balanced in an intermediate step with patella reduction, after inserting provisional tibial implants before the femoral bone cuts. More than 5 mm of posterior drawer at 90° of flexion led to an oversized femoral component compared to the AP dimensions of native condyles, which induced a 3-mm increase in femoral offset. In doubtful cases, marks were made with sterile pencil on the trial insert in front of the medial condyle, before and after applying the posterior drawer, to estimate drawer magnitude by the distance between the 2 marks. In all cases, the femoral component was rotated externally by 3° from the posterior bicondylar line. After insertion of the provisional femoral implant, excessive PCL tension was ruled out by checking that the insert remained spontaneously in place on its tibial baseplate.
Evaluation
Follow-up consisted of annual evaluations based on International Knee Society (IKS) scores [10] and a series of radiographs, including AP, lateral and skyline views.
Kinematics was recorded in the 0°–130° flexion range in two steps of the operation in the PCR group only. Pre-implantation kinematics was considered as reference and recorded after removal of all osteophytes and deep aspect release of the medial collateral ligament but before excising the ACL and before starting the bone cuts. Post-operative kinematics was recorded at the end of the operation with provisional implants in place and the patella reduced as retrospective control (extensive data analysis was conducted after the operation).
The navigation system displayed AP displacements of femoro-tibial contact points, as described previously [13]. Three-dimensional coordinates of these medial and lateral contact points were recorded in a tibial reference frame over the entire range of the passive tibio-femoral path. Bone morphing, which consisted of digitizing bone surfaces and adjusting a statistically deformable model based on the data collected, provided a working knee paradigm. The system delivered measurements with tenth-of-a-millimetre precision. After acquiring the anatomic points, the model obtained on the screen was tested by palpating the real articular surface and was accepted only if discrepancies between real and virtual points were <1 mm. Measurement reproducibility was tested by recording 10 flexion–extension cycles for each acquisition, producing superimposed displacement curves that were finally averaged by logistic regression with high significance (p < 0.01) (meaning that the majority of points were grouped around the regression line). Knees were flexed manually by maintaining the feet in a neutral position while leaving the femur free to rotate. Tibio-femoral contact points were defined as the most distal femoral points relative to the tibial reference frame. We defined the AP displacement of these contact points as the horizontal distance between two extreme positions: full extension and 130° of knee flexion. At the same time, axial rotation of the femur on the tibia was calculated.
Paradoxical displacements were deduced from measurement of AP displacements of femoro-tibial contact points within 30° intervals of flexion and then summarized on flexion extension cycle totality. Secondary criteria were axial rotation, measured in the same manner, and 6-month active flexion range, gauged manually by goniometer.
Institutional Review Board approval (No. IRB00006477) was obtained from our institution (Paris North Hospitals, Paris 7 University, Assistance Publique-Hôpitaux de Paris).
Statistical analysis
Because the primary goal of the presented technique was to restore AP kinematics, the difference between original and final AP displacements of the femoro-tibial contact points was tested. Measuring 5-mm difference between pre- and post-operative AP displacements of contact points with 5-mm standard deviation required at least 17 patients for 90 % power analysis. A 5-mm difference appeared consistently because it was substantially superior to measurement precision and clinically relevant. IKS scores and flexion ranges of the test and control groups were compared by Student’s t test. Pre- and post-operative AP displacements (mm) and axial rotation (in degree) were compared by matched-pair Student’s t test. The threshold for significance was set at p < 0.05.
Results
The femoral component was oversized in 16 cases in the test group (PCR-TKR). Average posterior bone resection was 8 ± 2 mm on the medial side and 6 ± 2 mm on the lateral side, smaller than the 12-mm thickness of prosthetic condyles. The femoral component was oversized in 14 cases from the control group (deep dished). Average posterior resection was 9 ± 3 mm on the medial side and 7 ± 3 mm on the lateral side.
No paradoxical displacement persisted after implantation in the test group, except in one case, in whom it was already present in the original knee. In this particular patient, residual paradoxical forward displacement of the medial condyle was 11 mm, which increased by 5 mm compared to pre-implantation values.
Overall, the magnitude of posterior displacements between 0° and 130° was significantly decreased for both medial and lateral condyles. On average, medial condyle backward displacement declined from 9 ± 9 to 1 ± 5 mm at the end of the operation (p < 0.001) (Fig. 1). Lateral condyle backward displacement decreased from 16 ± 14 to 6 ± 6 mm (p = 0.006) (Fig. 2).
More detailed analysis showed that the medial condyle rolled backward in 0°–30°, 30°–60° and 120°–140° intervals, although these mean displacements were lower than pre-operatively (p values of 0.01, 0.01 and 0.3, respectively). In contrast, paradoxical roll forward was observed in 60°–90° and 90°–120° intervals (Fig. 3).
The lateral condyle rolled backward in every 30° interval, but the distance was significantly lower than before implantation in 0°–30°, 60°–90° and 90°–120° intervals (p values of 0.004, 0.03 and 0.04, respectively) (Fig. 4).
In full extension, both condyles lay 5 and 6 mm, respectively, backward of their native position (p < 0.001) (Figs. 5, 6).
Overall, mean external axial rotation of the femur on the tibia decreased from 18° ± 10° to 8° ± 5° (p = 0.03) (Figs. 7, 8).
Finally, flexion gain was 5° ± 22° in the test group with final flexion of 124° ± 17°, which was not significantly different from control group values. Final IKS scores were also not significantly different (Table 2).
Discussion
The most important finding of the present study was that increased posterior femoral offset allowed optimization of PCL tension without compromising flexion range. In fact, there was no residual paradoxical kinematics in 20 of 21 patients, none of whom had stiff knee. Intra-operative monitoring of AP displacements appears to be an original and precise way of checking PCL tension. This technique for optimizing flexion gap balance seemed to be more beneficial when the PCL was retained. We reported more frequent residual paradoxical displacements (4 out of 10 cases) with deep-dished PS implants and the same technique. These results plead for PCL preservation.
In contrast, conventional gap balancing was found to leave persistent paradoxical forward displacements at squatting in about 70 % of cases, as reported by Dennis et al. [4], who scrutinized the kinematics of 72 patients with PCR implants. These authors investigated active knee kinematics by dual fluoroscopy and observed abnormal displacements that would not have been possible without some persistent laxity at the end of the procedure. Other studies confirmed these findings [3–5, 18–20, 22–24].
We are aware that control of laxity at the end of the operation will not guarantee the absence of paradoxical displacements under load and during daily activities. However, the non-existence of residual laxity remains the best intra-operative indication of adequate ligamentous tension to date. Similarly, consistent intra-operative kinematics (absence of roll forward at knee flexion) might be the only available predictive factor for sound post-operative kinematics, because it takes additional parameters into account, such as insert design, collateral ligament tension and patellar tracking. However, load amount and type as well as active extensor apparatus contraction may ultimately amplify AP displacements, as suggested by Yoshiya et al. [23].
Although AP displacement directions and axial rotation were maintained, the present study showed that their magnitude was reduced significantly. This can result from ACL resection, which occurs in the normal course of almost all TKRs and modifies the position of femoro-tibial contact points in extension. In fact, the condyles appear more posterior in extension than in the native knee, thereby inducing a decrease in rollback magnitude. Stiehl et al. [20] determined that this posterior translation of femoro-tibial contact points in full extension was 16 mm. Their results were confirmed by anatomical observations in cadaver knees by Yue et al. [24] who noted that mean posterior translation was 4 mm after ACL sectioning. It is likely that extensor apparatus contraction at footstep substantially amplifies this translation that Dejour et al. [2] described as an active anterior drawer. Miller et al. [17] demonstrated experimentally that posterior femur translation weakens extensor apparatus action by decreasing patello-tibial angle, thereby inducing instability or giving way eventually.
Because PCL action appears to be effective above 60° of flexion, as reported by Li et al. [11], it is surprising that some forward rolling of the medial condyle occurs in higher flexion intervals. This phenomenon can be explained by the effect of the insert’s posterior rim that could induce re-centering of the medial condyle above the central part of its corresponding glenoid, thus preventing posterior dislocation. Dennis et al. [3] observed anterior translation of the medial condyle in a series of patients with postero-substituting implants investigated by dual fluoroscopy. However, in the present study, it was verified that the condyles did not ultimately trespass their initial position in full extension.
Decreased axial rotation after TKR has been seen in cadaveric studies as well as in active patients [1, 24]. Argenson et al. [1], investigating the kinematics of prostheses designed for hyperflexion, observed mean axial rotation of 4.9°, which was substantially inferior to its reportedly physiological value of about 20° [13]. In the present work, reduction of axial rotation resulted from the decreased asymmetry of condylar displacements, since the lateral condyle course was reduced significantly.
Oversizing the femoral component with an anterior reference produced tighter flexion gaps, which did not provoke flexion stiffness. It is possible that subsequently increased PCO played a role by delaying posterior impingement between the femoral cortex and the posterior margin of the tibial plateau. In a theoretical model, we noted that a 2-mm increment in posterior femoral offset augmented flexion range by 10° [15]. Geijsen et al. [7] also showed that an increase in PCO did not induce a reduction of the flexion range in PCR-TKR. Thus, in daily practice, augmenting posterior femoral offset if AP laxity persists after the tibial bone cut appears safe because it allows PCL tightening and does not compromise flexion.
The present work has some limitations. First, it deals with passive kinematics, so that its relationship with active kinematics under load remains unknown. In vivo investigations suggest that extensor apparatus contraction under load increases posterior displacement. Horiuchi et al. [9] found that posterior displacements in the first degrees of flexion were amplified under load. Fujimoto et al. [6] reported amplified posterior rolling in the loaded knee. However, although they are absent at the end of the operation, paradoxical displacements could appear secondarily. That is why, in the future, intra-operative kinematics should be compared to late post-operative active kinematics of the same patients explored by fluoroscopy. Second, the absence of long-term follow-up prevents us from drawing definitive conclusions about the strength of fixation and the resistance to wear of prostheses implanted by this particular technique. Third, clinical relevance is uncertain because the relationship between paradoxical displacements and functional results remains controversial. A meta-analysis, comparing the results with PCR and PS prostheses, failed to reveal differences between functional data and mobility ranges [21]. In contrast, Fantozzi et al. [5] determined that increased posterior rolling improves the functional results and mobility range under load.
Conclusion
Keeping these limitations in mind, we proposed an original technique to achieve effective PCL tension, without compromising flexion and short-term outcomes. Definitive validation requires further investigation of active kinematics in participating patients as well as long-term follow-up.
References
Argenson JN, Komistek RD, Mahfouz M, Walker SA, Aubaniac JM, Dennis DA (2004) A high flexion total knee arthroplasty design replicates healthy knee motion. Clin Orthop Relat Res 428:174–179
Dejour H, Walch G, Deschamps G, Chambat P (2014) Arthrosis of the knee in chronic anterior laxity. Orthop Traumatol Surg Res 100:49–58
Dennis DA, Komistek RD, Colwell CE Jr, Ranawat CS, Scott RD, Thornhill TS, Lapp MA (1998) In vivo anteroposterior femorotibial translation of total knee arthroplasty: a multicenter analysis. Clin Orthop Relat Res 356:47–57
Dennis DA, Komistek RD, Mahfouz MR, Haas BD, Stiehl JB (2003) Multicenter determination of in vivo kinematics after total knee arthroplasty. Clin Orthop Relat Res 416:37–57
Fantozzi S, Catani F, Ensini A, Leardini A, Giannini S (2006) Femoral rollback of cruciate-retaining and posterior-stabilized total knee replacements: in vivo fluoroscopic analysis during activities of daily living. J Orthop Res 24:2222–2229
Fujimoto E, Sasashige Y, Masuda Y, Hisatome T, Eguchi A, Masuda T, Sawa M, Nagata Y (2013) Significant effect of the posterior tibial slope and medial/lateral ligament balance on knee flexion in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 21:2704–2712
Geijsen GJ, Heesterbeek PJ, van Stralen G, Anderson PG, Wymenga AB (2014) Do tibiofemoral contact point and posterior condylar offset influence outcome and range of motion in a mobile-bearing total knee arthroplasty? Knee Surg Sports Traumatol Arthrosc 22:550–555
Heesterbeek PJ, Labey L, Wong P, Innocenti B, Wymenga AB (2014) A new spacer-guided, PCL balancing technique for cruciate-retaining total knee replacement. Knee Surg Sports Traumatol Arthrosc 22:650–659
Horiuchi H, Akizuki S, Tomita T, Sugamoto K, Yamazaki T, Shimizu N (2012) In vivo kinematic analysis of cruciate-retaining total knee arthroplasty during weight-bearing and non-weight-bearing deep knee bending. J Arthroplasty 27:1196–1202
Insall JN, Dorr LD, Scott RD, Scott WN (1989) Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res 248:13–14
Li G, Zayontz S, Most E, Otterberg E, Sabbag K, Rubash HE (2001) Cruciate-retaining and cruciate-substituting total knee arthroplasty: an in vitro comparison of the kinematics under muscle loads. J Arthroplasty 16:150–156
Mahoney OM, Noble PC, Rhoads DD, Alexander JW, Tullos HS (1994) Posterior cruciate function following total knee arthroplasty. A biomechanical study. J Arthroplasty 9:569–578
Massin P, Boyer P, Hajage D, Kilian P, Tubach F (2011) Intra-operative navigation of knee kinematics and the influence of osteoarthritis. Knee 18:259–264
Massin P, Boyer P, Sabourin M (2012) Less femorotibial rotation and AP translation in deep-dished total knee arthroplasty. An intraoperative kinematic study using navigation. Knee Surg Sports Traumatol Arthrosc 20:1714–1719
Massin P, Gournay A (2006) Optimization of the posterior condylar offset, tibial slope, and condylar roll-back in total knee arthroplasty. J Arthroplasty 21:889–896
Matsumoto T, Kubo S, Muratsu H, Matsushita T, Ishida K, Kawakami Y, Oka S, Matsuzaki T, Kuroda Y, Nishida K, Akisue T, Kuroda R, Kurosaka M (2013) Different pattern in gap balancing between the cruciate-retaining and posterior-stabilized total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 21:2338–2345
Miller RK, Goodfellow JW, Murray DW, O’Connor JJ (1998) In vitro measurement of patellofemoral force after three types of knee replacement. J Bone Joint Surg Br 80:900–906
Nilsson KG, Karrholm J, Gadegaard P (1991) Abnormal kinematics of the artificial knee. Roentgen stereophotogrammetric analysis of 10 Miller–Galante and five New Jersey LCS knees. Acta Orthop Scand 62:440–446
Ploegmakers MJ, Ginsel B, Meijerink HJ, de Rooy JW, de Waal Malefijt MC, Verdonschot N, Banks SA (2010) Physical examination and in vivo kinematics in two posterior cruciate ligament retaining total knee arthroplasty designs. Knee 17:204–209
Stiehl JB, Komistek RD, Dennis DA, Paxson RD, Hoff WA (1995) Fluoroscopic analysis of kinematics after posterior-cruciate-retaining knee arthroplasty. J Bone Joint Surg Br 77:884–889
Verra WC, van den Boom LG, Jacobs W, Clement DJ, Wymenga AA, Nelissen RG (2013) Retention versus sacrifice of the posterior cruciate ligament in total knee arthroplasty for treating osteoarthritis. Cochrane Database Syst Rev 10:CD004803
Victor J, Banks S, Bellemans J (2005) Kinematics of posterior cruciate ligament-retaining and -substituting total knee arthroplasty: a prospective randomised outcome study. J Bone Joint Surg Br 87:646–655
Yoshiya S, Matsui N, Komistek RD, Dennis DA, Mahfouz M, Kurosaka M (2005) In vivo kinematic comparison of posterior cruciate-retaining and posterior stabilized total knee arthroplasties under passive and weight-bearing conditions. J Arthroplasty 20:777–783
Yue B, Varadarajan KM, Moynihan AL, Liu F, Rubash HE, Li G (2011) Kinematics of medial osteoarthritic knees before and after posterior cruciate ligament retaining total knee arthroplasty. J Orthop Res 29:40–46
Acknowledgments
We thank Ovid Da Silva for editing this manuscript.
Conflict of interest
PM has received royalties from Zimmer in relation to materials not included in the present study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Donadio, J., Pelissier, A., Boyer, P. et al. Control of paradoxical kinematics in posterior cruciate-retaining total knee arthroplasty by increasing posterior femoral offset. Knee Surg Sports Traumatol Arthrosc 23, 1631–1637 (2015). https://doi.org/10.1007/s00167-015-3561-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-015-3561-4