Abstract
Purposes
This study analyzed morphological differences in the resected proximal tibial surfaces of Chinese males and females undergoing total knee arthroplasty (TKA) and compared the measurements with the dimensions of five currently used tibial implants.
Methods
The mediolateral (ML), middle anteroposterior (AP), medial anteroposterior (MAP), and lateral anteroposterior (LAP) dimensions of the resected tibial surfaces of 976 Chinese TKA knees (177 male, 799 female) were measured. The ML/AP ratio of every knee was calculated. These morphological data were compared with the dimensions of five currently used tibial implants.
Results
The ML, AP, MAP, and LAP dimensions of the resected proximal tibias showed significant differences according to gender. Compared with currently used tibial implants, the smaller implants showed tibial ML undersizing and the larger implants showed tibial ML overhang. The ML/AP aspect ratio progressively decreased with increasing AP dimension in the resected proximal tibias, which contrasts with the relatively constant or increased (NexGen) aspect ratio in currently used tibial implants. Males showed a higher ML/AP aspect ratio than females for a given AP dimension. This indicates that for an implant with a given AP dimension, the tibial ML dimension tends to be undersized in males and to overhang in females.
Conclusion
The results of this study may provide fundamental data for designing suitable tibial implants for use in the Chinese population, especially for design of gender-specific prostheses.
Level of evidence
II.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In addition to patient characteristics and surgical technique, matching the shape of the prosthesis to the resected bone surface is important for better clinical outcome and long-term component survival rate [2, 10, 20]. Therefore, it is critical to determine the anthropometric data of the knee at the resection level to design appropriate components for TKA candidates. Most knees that undergo TKA are deformed and are shaped quite differently from healthy knees. This suggests that the design of prostheses should be based on data from diseased knees [3]. In addition, since implants are placed directly on the resected bone surface, the morphometric data of the resected bone surface should be more useful for implant design than data obtained using radiology.
Several studies have reported that the anatomical morphology of knees is different in Asian populations compared a Caucasian population, with Asian populations having smaller dimension [5, 18, 19, 26]. Other studies have compared the anatomical profiles of Asian knees to those of currently used TKA implants, most of which were designed based on anthropometric data from Caucasian populations, and found that these implants are not suitable for use in Asian populations [4, 15, 17]. It is critical to design implants that are appropriate for use in such populations. However, few studies have investigated morphometric parameters of the resected tibial surface in a Chinese population. Here, we analyzed morphological differences in 976 resected proximal tibial surfaces in a large group of Chinese males and females undergoing TKA and compared these data with the dimensions of five currently used tibial implants. We hypothesize that within the Chinese population, there is a distinct gender difference in the intraoperative resected tibial surface and the currently used tibial implants mismatch the Chinese TKA patients.
Materials and methods
Morphological data of 976 resected proximal tibial surfaces obtained from February 2010 to August 2013. These included 177 (18 %) knees from males and 799 (82 %) knees from females who were undergoing primary TKA for Kellgreen and Lawrence IV. The average patient age was 67.4 ± 7.2 years for males and 65.9 ± 6.9 years for females. The average height was 168.9 ± 6.3 cm for males and 158.2 ± 5.6 cm for females. The average leg alignment was 9.2 ± 4.3 for males and 8.4 ± 4.5° for females. Patients were excluded if they had substantial bone loss and/or degradation requiring augmentation, or if they had a history of high tibial fracture or a congenital anomaly, or if they had a high tibial osteotomy.
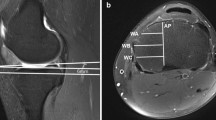
All surgeries were performed by the senior surgeon (JK Yu) using minimally invasive TKA. The knees were exposed through a medial parapatellar approach. Bone cut of the tibia was made with the extramedullary alignment guide perpendicular to the long axis of the tibia with a 7° posterior slope angle and 10-mm thickness below the surface of the less affected tibial plateau or 2 mm below the seriously damaged tibial plateau. The average thickness of the resection was 10.5 ± 1.7 mm in lateral and 4.4 ± 2.5 mm in medial plateau. Osteophytes were removed after the bone cuts. Four dimensions of the resected tibial surface were measured during surgery: the mediolateral (ML), middle anteroposterior (AP), medial anteroposterior (MAP), and lateral anteroposterior (LAP) dimensions (Fig. 1). All were measured in millimeters using a sterile slide caliper. The tibial ML dimension was taken as the longest ML length of the resected tibial surface, which perpendicular to a line connecting the center of the insertion of the posterior cruciate ligament and the medial 1/3 of the tibial tuberosity. The middle AP dimension was taken as the length of a line drawn perpendicular and passing through the midpoint of the ML line. The MAP and LAP dimensions were taken as the longest line drawn parallel to the middle AP and passing through the most posterior medial and lateral tibial condyle point, respectively. The ML/AP aspect ratio calculates as the ML dimension divided by the AP dimension ×100 and acts as a guide to predict the shape of the proximal tibia. The intraoperatively measured ML and AP dimensions and the ML/AP ratio were compared with five kinds of imported tibial implants that are commonly used in China: Duracon and Scorpio (Stryker Howmedica Osteonics), NexGen (Zimmer, Warsaw, Indiana), PFC Sigma (Depuy-Johnson and Johnson, Warsaw, Indiana), and UKnee (United Ortho Co, Taiwan). Patients provided informed written consent, and the study was approved by the institutional review board of Peking University Third Hospital.
Statistical analysis
The SPSS software 20.0 (SPSS, Chicago, IL) was used for statistical analysis. The dimensions were summarized as the mean and standard deviation. The independent sample t test was used to determine the significance of differences in males versus females. Linear regression analysis was used to determine the correlations of tibial ML, ML/AP, and AP dimension. All differences were considered significant when p < 0.05.
Results
Morphology of resected proximal tibias in males and females
Males had significantly larger ML, AP, MAP, and LAP dimensions than females (p < 0.05). The mean MAP dimension was larger than the mean LAP dimension in both males and females (p < 0.05), and there was no significant difference between males and females with regard to the MAP–LAP difference (n.s.). In addition, the MAP–LAP differences were highly variable. The MAP–LAP difference ranged from −11 to 15 mm for males and −13.5 to 15 mm for females (Table 1).
Correlations between intraoperatively measured ML and AP dimensions
There was a significant positive correlation between intraoperatively measured ML and AP dimensions in both males and females, with the AP dimension increasing as the ML dimension increased. The line for males is above the line for females, indicating that males generally have a larger ML dimension than females for a given AP dimension (Fig. 2).
Comparison of the dimensions of intraoperatively resected proximal tibias with the dimensions of five different tibial implants
For males, all sizes of the Duracon and UKnee tibial implants tended to be undersized in the ML dimension for a given AP dimension. The other three kinds of implants with smaller AP dimensions showed ML undersizing; however, when they had larger AP dimensions, there was ML overhang (Fig. 3). For females, all five tibial implants with smaller AP dimensions were undersized in the ML dimension while those with larger AP dimensions had overhang in the ML dimension (Fig. 4).
The tibial mediolateral (ML) dimension versus the middle anteroposterior (AP) dimension of the intraoperatively resected proximal tibial surfaces of 799 knees in females compared with the dimensions of tibial implants from five companies. The smaller the size of the tibial implants, the greater the extent of undersizing. Similarly, the larger the tibial implant, the greater the overhang
Comparison of the aspect ratio and AP dimension of resected tibial surfaces with those of five different tibial implants
The ML/AP aspect ratio of the resected tibias decreased with increasing AP dimension in both males and females. The line for males is above the line for females, showing that males generally have a larger aspect ratio than females for a given AP dimension (Fig. 5).
Notably, only the Duracon implant showed a decline in the aspect ratio with increasing AP. The aspect ratio of the other implants either did not change or increased (NexGen) with increasing AP dimension. In addition, though the aspect ratio of the Duracon implant decreased with increasing AP dimension, the rate of change did not match that of the measured morphological data (Figs. 6, 7).
Discussion
The most important finding of the current study is that the intraoperatively measured proximal tibial dimensions showed significant gender difference and mismatching with the dimensions of currently used tibial implants. In our study, males showed a higher ML dimension and ML/AP aspect ratio than females for a given AP dimension. In addition, compared with currently used tibial implants, the smaller implants showed tibial ML undersizing and the larger implants showed tibial ML overhang.
The tibial ML and AP dimensions are two parameters that are used to select an implant that is the correct size. In a Thai population, Chaichankul et al. [1] reported mean values of 74.4 and 50.2 mm for the tibial ML and AP dimensions of males, and mean values of 65 and 43.2 mm for females (determined by MRI). Cheng et al. [4] studied 172 Chinese knees using CT imaging and reported mean ML and AP dimension values of 76.4 and 51.3 mm for males and 68.8 and 45.7 mm for females, respectively. In those studies, the tibial resection surface at the level of a constant cutting depth was used to measure morphological data. This is not suitable for tibial implant design as the dimension of the resected tibial surface varies considerably depending on the level at which the cut is made. In this study, we measured the dimensions of the very large resected proximal tibial surface directly after completion of tibial cutting. These data should be more accurate and useful for analyzing whether the resected tibial surface and the tibia component are a good match [3, 21]. To determine whether standard tibial components are appropriately sized for use in the Chinese population, we compared the morphological AP and ML dimension data with the AP and ML dimensions of five currently used tibial implants. Our results showed that these implants were not suitable for Chinese population. The smaller implant size was too small, and the larger implant size was too large for tibias with a given AP dimension. This leads to implant ML undersizing with smaller AP dimensions and to overhang with implants that have a larger AP dimension.
There has been considerable controversy regarding symmetric versus asymmetric tibial component design. Several studies report that the proximal tibia is asymmetric, with a medial plateau that is larger than the lateral plateau. Cheng et al. [4] reported that the medial plateau was larger than the lateral plateau by a mean of 5.6 mm in males and 5.1 mm in females. Hitt et al. [11] confirmed that the medial plateau was larger than the lateral plateau by a mean of 5.2 mm in males and 4.3 mm in females during 337 consecutive TKAs. The same findings were found in our study that the medial plateau was larger than the lateral plateau by a mean of 3.0 mm for males and 3.8 mm for females. In theory, an asymmetric tibial component would be expected to cover the tibial surface more completely than a symmetric component. However, there is no compelling evidence that an asymmetric or a symmetric design leads to better coverage and function. Some researchers have proposed using an asymmetrical tibial component [23, 24], while others prefer a symmetrical one [12, 15].
Although previous studies showed that the proximal tibia has a larger medial plateau than the lateral plateau as a whole [4, 11, 15], none of these studies took into account the variability of the MAP–LAP difference in the proximal tibia, which was shown in the present study. The MAP–LAP differences of the resected proximal tibias were highly variable. Our study showed that the MAP–LAP difference ranged from −11 to 15 mm for males and from −13.5 to 15 mm for females. This spread of values indicates that a small number of patients have a lateral tibial plateau that is larger than the medial plateau. This was similar to findings of a study by Westrich et al. [22] that measured the resected tibial surfaces of Japanese patients. In that study, the LAP/MAP ratios at 10, 20, and 30 % distances from the periphery to the middle AP ranged from 92.1 to 114.3 %, from 86.8 to 116.3 %, and from 82.5 to 115.6 %, respectively. This also showed that some patients have larger lateral tibial plateaus.
In TKA, tibial implants that closely match the resected tibial surface provide the best stability and stress transfer characteristics. A good match is also important for minimizing soft tissue complications, tibia component sinking, and loosening as well as to avoid long-term postoperative complications [12, 15]. If the implant surface does not match the resected bone surface, there will be undersizing or overhang [9]. Chau et al. reported that tibial component overhang larger than 3 mm demonstrated significantly worse Oxford Knee Scores and pain scores when compared to overhang less than 3 mm after 5 years surgery. The authors suggested that tibia component overhang does not exceed 3 mm.
The ML/AP aspect ratio is used to describe the shape of the anticipated tibial component [15]. An appropriate aspect ratio is critical for ensuring that the tibial component provides ideal coverage of the resected tibial surface. Our morphological data showed that the aspect ratio (ML/AP) decreased as the AP dimension increased. Similarly, other studies also show a pattern of decreasing aspect ratio with increasing AP dimension [1, 4]. In contrast to this pattern in the study population, most implants have a constant or increased (NexGen) aspect ratio with an increasing AP dimension. Thus, it is clear that tibial components that are based on data from other populations could lead to undersizing or overhang problems in a Chinese TKA population. Of the five currently used tibial implants in this study, four kinds of prosthesis, which are manufactured by the European and American countries, were designed based on anthropometric data from Caucasian knees. One of them, the UKnee, was designed and manufactured in Taiwan based on the data from Chinese patients living in southern China. However, our TKA patients lived mainly in northern China. Studies showed that there are genetic and morphological differences in the populations of southern and northern China, although both are considered part of the Han ethnic group. Zhao et al. [27] reported that STAT4 polymorphism is significantly associated with rheumatoid arthritis susceptibility in northern, but no association with southern Hans Chinese subpopulations [16] Gu et al. [7] demonstrated that a smaller midface and a shorter overall mandibular length were observed in southern Chinese, whereas significantly increased vertical dimension and a retrusive chin were noted in northern Chinese. The mismatching of these tibial implants illustrates the importance of designing implants based on the characteristics of different ethnicities and subpopulations.
Several previous studies have shown that the tibial ML/AP aspect ratio does not vary substantially between males and females [10, 26]. However, significant gender differences appear when the ML/AP aspect ratio is adjusted using a given AP dimension [25]. The tibial implants used currently are unisex; that is, gender differences are not taken into consideration. The present study showed that in a Chinese population, the proximal tibias had a higher ML/AP aspect ratio in males than in females for a given AP dimension (Fig. 5). This indicated that the tibial ML dimension tends to be undersized in males and to have overhang in females for a tibial implant with a given AP dimension. For this reason, the differences of the proximal tibial shapes according to gender may be a concern when designing tibial components for Chinese males and females. In this population, males need a more oval-shaped tibial prosthesis (to prevent component undersizing) and females need a more spherically shaped tibial prosthesis (to prevent component overhang) for a given AP dimension.
Recent studies have demonstrated ethnic differences in proximal tibia morphology [6, 9, 14]. Especially, Asian populations have been reported to have smaller size than Caucasian populations. Yue et al. [26] demonstrated that the ML and AP dimension of Chinese populations is smaller than Caucasian population by an average of 3.5 and 3.5 mm for males and 3.2 and 2.0 mm for females, respectively. Mahfouz et al. [19] reported mean ML and AP dimension values of Asian population is smaller than Caucasian population by mean of 10.9 and 5.5 mm for males and 0.6 and 1.9 mm for females, respectively. However, most existing TKA components designs are based on the Caucasian population. Some studies have compared the matching of current tibia implant systems in Chinese, Korean populations and found that implants tend to overhang or undersize in these Asian populations [4, 8, 17]. Iorio et al. [13] reported that Japanese patients had significantly less postoperative range of motion and a higher revision rate than American patients after primary TKAs. These suggested ethnic differences should be taken into account when designing TKA components fit for use in Asian populations.
The limitation of this study was that the slide calipers used to measure data is accurate to 0.5 mm, which should be noted when interpreting the results. Another limitation is that the study does not provide clinical outcomes and further study should be needed to concentrated on clinical research.
Conclusion
The present study evaluated the morphology of proximal tibia after bone cutting during TKA in a large group of Chinese population. Our results showed that males have larger dimensions and aspect ratios than their female counterparts, and no one current used tibia implant could matching the intraoperatively measured resected tibias surface very well. These anthropometric data may be useful for future designing suitable tibial implants for use in the Chinese population, especially for design of gender-specific prostheses.
References
Chaichankul C, Tanavalee A, Itiravivong P (2011) Anthropometric measurements of knee joints in Thai population: correlation to the sizing of current knee prostheses. Knee 18:5–10
Chau R, Gulati A, Pandit H, Beard DJ, Price AJ, Dodd CA, Gill HS, Murray DW (2009) Tibial component overhang following unicompartmental knee replacement-does it matter? Knee 16:310–313
Cheng KC, Chen YL, Ye ML, Chun HH (1999) A new approach of designing the tibial baseplate of total knee prostheses. Clin Biomech 14:112–117
Cheng FB, Ji XF, Lai Y, Feng JC, Zheng WX, Sun YF, Fu YW, Li YQ (2009) Three dimensional morphometry of the knee to design the total knee arthroplasty for Chinese population. Knee 16:341–347
Chin PL, Tey TT, Ibrahim MY, Chia SL, Yeo SJ, Lo NN (2011) Intraoperative morphometric study of gender differences in Asian femurs. J Arthroplasty 26:984–988
Dai Y, Bischoff JE (2013) Comprehensive assessment of tibial plateau morphology in total knee arthroplasty: influence of shape and size on anthropometric variability. J Orthop Res 31(10):1643–1652
Gu Y, Hagg U, Wu J, Yeung S (2011) Differences in dentofacial characteristics between southern versus northern Chinese adolescents. Aust Orthod J 27:155–161
Ha CW, Na SE (2012) The correctness of fit of current total knee prostheses compared with intra-operative anthropometric measurements in Korean knees. J Bone Joint Surg Br 94(5):638–641
Hartel MJ, Loosli Y, Gralla J, Kohl S, Hoppe S, Röder C, Eggli S (2009) The mean anatomical shape of the tibial plateau at the knee arthroplasty resection level: an investigation using MRI. Knee 16:452–457
Harwin SF, Greene KA, Hitt K (2007) Early experience with a new total knee implant: maximizing range of motion and function with gender-specific sizing. Surg Technol Int 16:199–205
Hitt K, Shurman JR II, Greene K, McCarthy J, Moskal J, Hoeman T, Mont MA (2003) Anthropometric measurements of the human knee: correlation to the sizing of current knee arthroplasty systems. J Bone Joint Surg [Am] 85-A:115–122
Incavo SJ, Ronchetti PJ, Howe JG, Tranowski JP (1994) Tibial plateau coverage in total knee arthroplasty. Clin Orthop Relat Res 299:81–85
Iorio R, Kobayashi S, Healy WL, Cruz AI Jr, Ayers ME (2007) Primary posterior cruciate-retaining total knee arthroplasty: a comparison of American and Japanese cohorts. J Surg Orthop Adv 16(4):164–170
Küçükdurmaz F, Tuncay I, Elmadağ M, Tunçer N (2014) Morphometry of the medial tibial plateau in Turkish knees: correlation to the current tibial components of unicompartmental knee arthroplasty. Acta Orthop Traumatol Turc 48(2):147–151
Kwak DS, Surendran S, Pengatteeri YH, Park SE, Choi KN, Gopinathan P, Han SH, Han CW (2007) Morphometry of the proximal tibia to design the tibial component of total knee arthroplasty for the Korean population. Knee 14:295–300
Li H, Zou Q, Xie Z, Liu Y, Zhong B, Yang S, Zheng P, Yang F, Fang Y, Wu Y (2009) A haplotype in STAT4 gene associated with rheumatoid arthritis in Caucasians is not associated in the Han Chinese population, but with the presence of rheumatoid factor. Rheumatology (Oxford) 48:1363–1368
Lim HC, Bae JH, Yoon JY, Kim SJ, Kim JG, Lee JM (2013) Gender differences of the morphology of the distal femur and proximal tibia in a Korean population. Knee 20:26–30
Liu Z, Yuan G, Zhang W, Shen Y, Deng L (2013) Anthropometry of the proximal tibia of patients with knee arthritis in Shanghai. J Arthroplasy 28(5):778–783
Mahfouz M, Abdel Fatah EE, Bowers LS, Scuderi G (2012) Three-dimensional morphology of the knee reveals ethnic differences. Clin Orthop Relat Res 470:172–185
Mahoney OM, Kinsey T (2010) Overhang of the femoral component in total knee arthroplasty: risk Factors and clinical consequences. J Bone Joint Surg [Am] 92:1115–1121
Uehara K, Kadoya Y, Kobayashi A, Ohashi H, Yamano Y (2002) Anthropometry of the proximal tibia to design a total knee prosthesis for the Japanese population. J Arthroplast 17(8):1028–1032
Westrich GH, Haas SB, Insall JN, Frachie A (1995) Resection specimen analysis of proximal tibial anatomy based on 100 total knee arthroplasty specimens. J Arthroplasy 10:47–51
Westrich GH, Agulnick MA, Laskin RS, Haas SB, Sculco TP (1997) Current analysis of tibial coverage in total knee arthroplasty. Knee 4:87–91
Wevers HW, Simurda M, Griffin M, Tarrel J (1994) Improved fit by asymmetric tibial prosthesis for total knee arthroplasty. Med Eng Phys 16:297–300
Yang B, Yu JK, Zheng ZZ, Lu ZH, Zhang JY, Cheng JH (2013) Computed tomography morphometric study of gender differences in osteoarthritis proximal tibias. J Arthroplasy 28:1117–1120
Yue B, Varadarajan KM, Ai S, Tang T, Rubash HE, Li G (2011) Differences of knee anthropometry between Chinese and white men and women. J Arthroplast 26:124–130
Zhao Y, Liu X, Liu X, Su Y, Li Y, Zhang X, Zhu L, Wang S, Wang T, Jiang Q, Liu X, Li X, Huang C, Jia R, Lu X, Guo J, Li Z (2013) Association of STAT4 gene polymorphism with increased susceptibility of rheumatoid arthritis in a northern Chinese Han subpopulation. Int J Rheum Dis 16:178–184
Acknowledgments
This Study was funded by the Sino-Germany Cooperation Project of Ministry of Science and Technology of China (No. 2011DFA31340); the Beijing Science and Technology Planning Projects of Beijing Science and Technology Committee (No. Z131100005213004); Instrument Research Project of the National Natural Science Foundation (No. 81327001).
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yang, B., Song, Ch., Yu, Jk. et al. Intraoperative anthropometric measurements of tibial morphology: comparisons with the dimensions of current tibial implants. Knee Surg Sports Traumatol Arthrosc 22, 2924–2930 (2014). https://doi.org/10.1007/s00167-014-3258-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-014-3258-0