Abstract
Trochleoplasty is a surgical procedure, whose goal is to change the abnormal shape of the femoral trochlea in patients with recurrent patellar dislocation. Such surgeries that aim to reshape the articular surface of a bone without damaging it are quite unique in orthopaedic surgery. Although in the beginning, trochleoplasty was reserved for the refractory cases where previous surgery has failed, the last years it became more and more popular because of a better knowledge of anatomy and biomechanics and a greater availability of instruments. The roots of the deepening trochleoplasty could be found in the previous century when the first surgeons tried to directly remove the dysplastic bone with pioneer interventions but with devastating consequences. Since then, multiple procedures have been described and are analysed in this review; each one with its unique features, advantages and pitfalls. Regardless of the technique used, the very recent bibliography presents very encouraging results from the application of trochleoplasty with other procedures in a selected population with severe trochlear dysplasia and recurrent patellar dislocation, in whom the benign neglect of dysplasia would lead to unfavourable results. Level of evidence IV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Trochleoplasty is a surgical procedure, which will help the surgeon to change the shape of the distal femur articular surface, in particularly the trochlea. Similar surgeries that reshape the articular surface of a bone are not so often in orthopaedics. The goal of trochleoplasty is quite ambitious because this surgery changes what the natural evolution has done during bone growth (Fig. 1). Trochleoplasty involves working directly on the patellofemoral (PF) joint with a high risk of cartilage damage, modification of the congruency between the two articulating bones and alteration of joint kinematics. All these factors are fundamental for the long-term joint preservation and could potentially lead to early arthritis. The reason for that drastic surgical choice is to achieve stability and congruency in patients with recurrent patellar dislocation. Continuous stability of the PF joint throughout the whole knee range of motion is of absolute importance for the normal function of the extensor mechanism, human erect stance and bipedalism. Trochleoplasty became more and more popular during recent years because of a better knowledge of joint anatomy and biomechanics. The technical offer in terms of surgical instrumentation and imaging technology also allowed surgeons to attempt more extreme procedures.
The roots of the deepening trochleoplasty could be found in 1890. An English surgeon doctor Bilton Pollard identified in certain patients a condition where the distal femur is ‘ill-shaped or ill-developed’ as the main reason for irreducible patellar dislocation [40]. Pollard considered that the presence of this severe trochlear dysplasia led to persisting patellar dislocation, and he performed an open surgery to correct it. Pollard’s founding intervention had been reported by another English surgeon, Douglas Drew in 1908, who focused on the ‘possibly congenital’ reduced lateral facet height in patients with persisting patellar dislocation [22]. Drew stated that patellar dislocation results mostly from a congenital dysplastic distal femur and considered genu valgum, as a secondary factor. In these patients, the presence of trochlear dysplasia had not been yet clearly identified, but the abnormal and flat trochlear shape led these two surgeons to perform a procedure where they widened and deepened the groove by directly removing the cartilage and cutting and gauging the trochlea. They reserved the surgical treatment of this condition, in cases where patellar dislocation persists after genu valgum correction with a Macewen’s osteotomy (varization distal femoral osteotomy) [40]. This revision option included the ‘division of the capsule and deepening of the trochlear surface of the femur’ and may be now considered as the first described type of trochleoplasty technique [40]. Although at the time there was little attention paid to the preservation of the cartilage, it is interesting to notice that first Pollard [40] and then Drew [22] considered that trochlear dysplasia is mostly caused because of an elevated groove in the midline of the trochlea.
The possible disadvantages from damaging the trochlear cartilage and exposing cancellous bone had been already identified as a risk factor. A few years later, J.B. Murphy, who was mostly focused in surgical techniques for the prevention of ankylosis, considered the shallow trochlear groove as a principal factor for patellar dislocation, and he thought that its correction must focus on deepening the groove [35]. Murphy was concerned about the damage of the cartilage and the exposure of cancellous bone in contact to the patella and added fat tissue between the patella and the femur in a ‘biologic interposition’ fashion in order to reduce scarring and adhesions by the exposed cancellous femoral bone [35].
Until that time, trochleoplasty procedures appeared in the European medical literature and surgeons considered that the principal factor of trochlear dysplasia was the elevated trochlear groove. This is why the techniques to correct it so far involved deepening of the trochlea posteriorly. At the time, there was no trochlear dysplasia classification to identify the possible many variants of this pathology and medical publications travelled more difficultly than today. These are probably some of the reasons that a year later, a different aspect appeared in the other side of the Atlantic. The American surgeon Fred H. Albee from the ‘New York Postgraduate Medical School Clinic’ was not treating knee pathologies specifically, but his work was mostly focused on bone grafting. In 1915, Albee published a general textbook about techniques for bone grafts, where he considered that trochlear dysplasia was the result of a reduced lateral facet height and that the abnormal flat surface of the trochlea was mostly because of a depressed lateral facet rather than an elevated trochlea in the midline [1]. So, he attempted to correct it by addressing the reduced lateral facet height: the lateral facet was osteotomized, and a mobile flat was created. The flap was elevated anteriorly enough to create a mechanical block for pathological lateral patellar translation. Then a bone graft was impacted under the lateral facet in order to augment and stabilize the reconstruction [1]. This was the ‘lateral facet-elevating’ trochleoplasty (Fig. 2). Similar trochleoplasty techniques that involved the augmentation of the dysplastic lateral facet with graft were described later by Brisard [15] and Kobayashi and Toshihiro [30], but they are rarely used because they cause increased patellofemoral contact forces and pain.
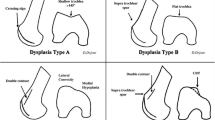
After the later introduction of the first trochlear dysplasia description and the definition of the normal range of the sulcus angle by Brattström in 1964 [14], the different characteristics and anomalies were better studied. Attention was paid to whether the dysplasia is caused by an anteriorly elevated trochlear groove in the midline, a posteriorly depressed (hypoplastic) lateral facet or both (Fig. 3). These findings in addition to the study of the normal values of the sulcus angle led Masse in 1978 to present a more drastic concept for correcting trochlear dysplasia [33]. Masse described another type of deepening trochleoplasty. In order to reduce the elevated groove in the midline, he did not work directly anteriorly on the cartilaginous groove, but he undermined the bone posteriorly to it, according to a technique he had learnt from Merle D’Aubigné [21]. After perforating and ‘emptying’ the cancellous bone behind the elevated groove, he created a free flap that could be pushed posteriorly and thus reduce the deformity [33]. Unfortunately, the groove was then depressed by directly impacting and hammering the cartilaginous trochlea. Although the cartilage was not violated by directly working on it as in the earliest trochleoplasties, it was probably damaged by the strikes of the hammer. This was the reason for the associated distal femur fractures he had with this technique. Nevertheless, Masse reported ‘good’ results in 15 patients with this technique [33].
The protection of the cartilaginous trochlea and the recreation of a normal sulcus angle were the key points of the following and most time-lasting type of deepening trochleoplasty, described by the Lyonnaise team of Henri Dejour in 1987 (Fig. 4) [19]. Dejour presented his deepening trochleoplasty whose goal was to depress the elevated groove or ‘bump’, as he named it [20], and also to create a narrower and normal sulcus angle, but without damaging the cartilage. In his technique, he also burred and undermined the cancellous bone behind the elevated groove, but then he osteotomized the trochlea in the midline, thus creating two independent flaps and a V-shaped groove that could be pushed posteriorly and form a normal sulcus angle. With this technique, the supratrochlear prominence was reduced posteriorly, but also a normal sulcus angle and a deep trochlear groove were recreated so that the patella engages properly [19, 20]. The two flaps were fixed with the use of two metallic screws, respectively.
The evolution of the fixation devices and the respect to the cartilage were the main advances for the subsequent types of trochleoplasties. In 1994, Bereiter presented another type of trochleoplasty known as the ‘Bereiter’ or ‘thin-flap’ technique (Fig. 5) [7]. In this procedure, a 3–5 mm osteochondral flap is first elevated from the whole of the trochlea. Then, the underlying cancellous bone is burred and deepened until the prominence disappears, the groove is flush with the anterior femoral cortex, and a V-shaped groove is fashioned on the cancellous bone. The osteochondral flap is depressed on the newly shaped bone and is fixed with sutures throughout its perimeter [7]. This technique was later followed by von Knoch et al. [46] with a maximum of 14-year follow-up and successful results, by Utting et al. [44] and by Fucentese et al. [25, 26] with similarly successful results. In 2010, Blønd and Schöttle performed the ‘Bereiter’ trochleoplasty by arthroscopy: while working through suprapatellar portals, they elevated a thin osteochondral trochlear flake, undermined the cancellous bone behind it with the use of an arthroscopic shaver and fixed the flap with the use of anchors and absorbable sutures (Fig. 6) [12].
In 2002, French surgeon Goutallier presented another technique for trochleoplasty that was named ‘recession’ or ‘recession-wedge’ trochleoplasty [27]. In this procedure, the abnormal flat or even convex trochlear shape and the wide sulcus angle were disregarded. Emphasis was given on the supratrochlear spur that was considered impossible for the patellar to override during flexion. The goal was only to ‘push’ and depress the prominent trochlea to the level of the anterior femoral cortex (Fig. 7). Surgery was technically less demanding than the deepening trochleoplasty since the cartilage of the trochlea was not violated, but on the other hand, the convexity of the groove and the wide sulcus angle did not change. The procedure was introduced for the treatment of patellar dislocation and anterior knee pain. Beaufils has followed this technique and has presented his successful results from the ‘recession-wedge’ trochleoplasty [6, 43]. The rationale of the recession trochleoplasty is to create a ‘closing-wedge’ osteotomy plane directed from proximally to distally at the level and behind the dysplastic trochlea. After the wedge is removed, the trochlea is pushed posteriorly. The cartilage is not violated, the sulcus angle is not changed, but there is a drastic effect on ‘pushing’ the prominence posteriorly. There is theoretical risk when damage to the subchondral bone will create a thin flap under the cartilage with impaired vascularization. It is interesting to notice that their results in terms of the post-operative development of patellofemoral osteoarthritis are similar to the ones after deepening [16, 21, 37, 45] or ‘Bereiter’ trochleoplasty [25, 44, 46], where the cartilage is actually ‘osteotomized’ or elevated as a flap, respectively. This along with the data of Fucentese et al. [25] and Schöttle et al. [42] on the good early cartilage viability after trochleoplasty, probably put emphasis on the higher significance of the established preoperative degenerative changes and the effect of patellar dislocation on PF cartilage, rather than the consequence of trochleoplasty on the long-term development of patellofemoral arthritis.
The interest on studying the morphology of trochlear dysplasia was also strong in the works of Biedert, who analysed the decreased trochlear depth and identified its cause as either an elevated trochlea floor or a flattened lateral and/or medial condyle [9]. He compared the height of the medial, central and lateral third of the trochlea according to the width of the lateral condyle, and he discovered that a reduced height of the lateral condyle more than 77 % was pathologic and that in more than 80 % of patients with patellar dislocation the pathology is located in the middle (elevated groove) and medial (hypoplastic facet) third [9]. These patients would benefit from a deepening trochleoplasty procedure [9]. Biedert et al. [10] also recorded another type of trochlear dysplasia that could not be included in the earlier Dejour’s classification in which none of the previously described radiological findings existed: the ‘too short lateral articular trochlea’ and he also introduced the ‘lateral condylar index’. This corresponds to the relative length of the anterior and posterior lateral femoral condyle and values of 86 % or less are considered pathognomonic of a short trochlea that does not extend proximally enough to engage the patella [10]. He suggested that these patients would benefit from a trochlea-lengthening osteotomy with or without elevating the lateral facet [8]. In this technique, a sagittal osteotomy of the lateral femoral condyle is performed and the facet is elevated with the addition of autograft under it, which also extends more proximally.
Other less known described techniques for trochleoplasty include the ‘proximal groove plasty’ by Peterson et al. in 1988 [38]. In this simplistic technique, a rounded osteotome is used to remove the supratrochlear spur and to create a ‘new’ groove in its place. The surrounding supratrochlear synovium is advanced and sutured around the trochlea. The height of the facets is not changed, and the effects from the obvious cartilage damage are not known. A similar abrasion trochleoplasty was described by Beals and Buehler in a small number of children with severe dysplasia, patellar dislocation, chromosomal abnormalities and limited motor demands [5]. Peterson and Vasiliadis have also presented an open proximal open trochleoplasty (‘grooveplasty’) where a curved osteotome removes from the central dysplastic groove the amount of bone and cartilage required in order to create a deep sulcus (Fig. 8) [39].
In 2010, D. Dejour presented the modification of the ‘Lyon’s School’ sulcus-deepening trochleoplasty with the combination of soft-tissue procedures for the treatment of recurrent patellar dislocation in patients with underlying high-grade trochlear dysplasia (type B and D) [18]. This new surgical technique was also the result of the more meticulous analysis of the 4 types of dysplasia and the introduction of a new and the most consistent so far classification of trochlear dysplasia (Fig. 9). The rationale of this surgical procedure is to restore the normal anatomy and to reshape the trochlea by undermining the cancellous bone and deepening the groove. The amount of bone removal is determined to have a new trochlear groove flushed with the anterior femoral cortex and to make the prominence disappear. The trochlea is osteotomized with a scalpel carefully over the position of the new trochlear groove. In this technique, the new trochlear groove is positioned according to the preoperative TT-TG value in a more lateral position, in order to reduce an excessive TT-TG value within normal limits. This had been previously shown by Schöttle et al. in 2005 [41], who demonstrated a 10 mm TT-TG reduction in their series after trochleoplasty. This TT-TG reduction may alleviate the need for an additional distal procedure (tibial tuberosity medialization). The trochlear facets are pushed gently posteriorly until they are flush with the femoral cortex, and they are fixed with anchors and absorbable sutures (Fig. 10). The important points of this technique are that a thick osteocartilaginous flap is created, enough bone can be removed to make the prominence disappear, the sulcus angle is decreased, and additionally, a ‘proximal’ realignement procedure by lateralizing the trochlear groove is performed [18].
Trochleoplasty procedures are more and more widely performed as a primary or a revision option in selected patients with recurrent patellar dislocation and underlying trochlear dysplasia. There are publications including results from hundreds of patients treated by trochleoplasty with different techniques. Despite the different surgical rationale behind each technique, all these authors present extremely successful results in terms of recurrence of dislocation. Residual pain or stiffness may complicate surgery, but patellar redislocation is rare among these results. Trochleoplasty is not a panacea for any patient with patellar dislocation, but should be tried in patients with high-grade trochlear dysplasia, in whom the patella cannot override the severe trochlear bony prominence during early flexion. Authors also present different results in terms of post-operative functional scores, the presence of post-operative apprehension sign or crepitus, but they all present almost 0 % of redislocation rate after trochleoplasty [4, 6, 16, 17, 23, 36, 37, 43]. The possible damage of cartilage after trochleoplasty seems to be minimal, but is also difficult to evaluate in these patients, in whom it is well-established that the recurrent patellar dislocation—if left untreated—will eventually lead to patellofemoral osteoarthritis [32].
In conclusion, regardless of the technique used, most authors agree that:
-
Trochleoplasty procedures are technically demanding, but they remain extremely successful in the treatment of recurrent patellar dislocation, if the proper inclusion criteria are met.
-
The ideal indication for trochleoplasty is true and documented patellar dislocation with underlying high-grade (type B and D) trochlear dysplasia, and especially after previous failed surgery.
-
Patellofemoral arthritis, skeletally immature patients and isolated patellofemoral pain are contra-indications of trochleoplasty.
-
Trochleoplasty procedures are always combined with other soft-tissue procedures (e.g. medial patellofemoral ligament reconstruction) and possibly with bony procedures (e.g. tuberosity osteotomies), when this is needed according to the ‘menu à la carte’ introduced by the Lyon Group of Dejour [20].
The recognition of the importance of trochlear dysplasia in the aetiology of patellar dislocation is growing and has been embraced by surgeons in Europe [4, 6, 8, 10, 12, 16, 17, 21, 23, 25–27, 36, 37, 42–46] but also, in the United States [3, 13, 23, 24], in the U.K. [21, 34] and in Japan [28, 29]. There are convincing data that there is a subgroup of patients with recurrent patellar dislocation and underlying high-grade trochlear dysplasia, in which the ‘benign neglect’ of dysplasia and the application of traditional surgery is ill-fated [6, 13, 27, 43, 44, 46]. The sound biomechanical evidence from the surgical treatment of trochlear dysplasia with sulcus-deepening trochleoplasty by Amis [2] and the satisfactory clinical results published by Von Knoch et al. [46], Verdonk et al. [45], Donell et al. [21], Blønd et al. [11, 12], Schöttle et al. [42], Goutallier et al. [27], Fucentese et al. [26], Thaunat et al. [43], Beaufils et al. [6], Nelitz et al. [36], Banke et al. [4], Koch et al. [31], Ntagiopoulos et al. [37], Dejour et al. [16] and others, confirm that trochlear dysplasia is a distinctive pathology in the aetiology of patellar dislocation, which must not be ignored or under-diagnosed, and that its treatment should be in the armamentarium of knee specialists. Trochleoplasty is known as a technically demanding procedure, and the evaluation and surgery should be kept among surgeons with special knowledge and surgical skills, in order to avoid future complications. Based on the literature, there is now indications that this seldom procedure should spread out.
References
Albee FH (1915) Bone graft wedge in the treatment of habitual dislocation of the patella. In: Albee FH (ed) Bone-graft surgery, vol 88. Med Record, New York, p 257
Amis AA, Oguz C, Bull AM, Senavongse W, Dejour D (2008) The effect of trochleoplasty on patellar stability and kinematics: a biomechanical study in vitro. J Bone Joint Surg Br 90(7):864–869
Arendt E (2005) Anatomy and malalignment of the patellofemoral joint: its relation to patellofemoral arthrosis. Clin Orthop Relat Res 436:71–75
Banke IJ, Kohn LM, Meidinger G, Otto A, Hensler D, Beitzel K, Imhoff AB, Schottle PB (2013) Combined trochleoplasty and MPFL reconstruction for treatment of chronic patellofemoral instability: a prospective minimum 2-year follow-up study. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-013-2603-z
Beals RK, Buehler K (1997) Treatment of patellofemoral instability in childhood with creation of a femoral sulcus. J Pediatr Orthop 17(4):516–519
Beaufils P, Thaunat M, Pujol N, Scheffler S, Rossi R, Carmont M (2012) Trochleoplasty in major trochlear dysplasia: current concepts. Sports Med Arthrosc Rehabil Ther Technol 4:7
Bereiter H, Gautier E (1994) Die trochleaplastik als chirurgische Therapie der rezidivierenden Patellaluxation bei Trochleadysplasie des Femurs. Arthroskopie 7:281–286
Biedert RM (2010) Trochlear lengthening osteotomy with or without elevation of the lateral trochlear facet. In: Arendt E, Dejour D, Zaffagnini S (eds) Patellofemoral pain, instability and arthritis: clinical presentation and treatment, vol 1. Springer, New York, pp 209–217
Biedert RM, Bachmann M (2009) Anterior-posterior trochlear measurements of normal and dysplastic trochlea by axial magnetic resonance imaging. Knee Surg Sports Traumatol Arthrosc 17(10):1225–1230
Biedert RM, Netzer P, Gal I, Sigg A, Tscholl PM (2011) The lateral condyle index: a new index for assessing the length of the lateral articular trochlea as predisposing factor for patellar instability. Int Orthop 35(9):1327–1331
Blond L, Haugegaard M (2013) Combined arthroscopic deepening trochleoplasty and reconstruction of the medial patellofemoral ligament for patients with recurrent patella dislocation and trochlear dysplasia. Knee Surg Sports Traumatol Arthrosc
Blønd L, Schöttle PB (2010) The arthroscopic deepening trochleoplasty. Knee Surg Sports Traumatol Arthrosc 18(4):480–485
Bollier M, Fulkerson JP (2011) The role of trochlear dysplasia in patellofemoral instability. J Am Acad Orthop Surg 19(1):8–16
Brattstroem H (1964) Shape of the intercondylar groove normally and in recurrent dislocation of patella. A clinical and X-ray-anatomical investigation. Acta Orthop Scand Suppl 68(Suppl 68):61–148
Brisard P (1950) Tactique opératoire dans le traitement des luxations congénitales et récidivantes de la rotule. Acta Orthop Belg 16:452–456
Dejour D, Byn P, Ntagiopoulos PG (2013) The Lyon’s sulcus-deepening trochleoplasty in previous unsuccessful patellofemoral surgery. Int Orthop 37(3):433–439
Dejour D, Ntagiopoulos PG, Saffarini M (2012) Evidence of trochlear dysplasia in femoral component designs. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-012-2268-z
Dejour D, Saggin P (2010) The sulcus deepening trochleoplasty-the Lyon’s procedure. Int Orthop 34(2):311–316
Dejour H, Walch G, Neyret P, Adeleine P (1990) Dysplasia of the femoral trochlea. Rev Chir Orthop Reparatrice Appar Mot 76(1):45–54
Dejour H, Walch G, Nove-Josserand L, Guier C (1994) Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc 2(1):19–26
Donell ST, Joseph G, Hing CB, Marshall TJ (2006) Modified Dejour trochleoplasty for severe dysplasia: operative technique and early clinical results. Knee 13(4):266–273
Drew D (1908) Dislocation of the patella (? Congenital); Operation; Cure. Proc R Soc Med 1 (Clin Sect):11–13
Duncan ST, Noehren BS, Lattermann C (2012) The role of trochleoplasty in patellofemoral instability. Sports Med Arthrosc Rev 20(3):171–180
Fithian DC, Neyret P, Servien E (2008) Patellar instability: the Lyon experience. Curr Orthop Pract 19(3):328–338
Fucentese SF, Schöttle PB, Pfirrmann CW, Romero J (2007) CT changes after trochleoplasty for symptomatic trochlear dysplasia. Knee Surg Sports Traumatol Arthrosc 15(2):168–174
Fucentese SF, Zingg PO, Schmitt J, Pfirrmann CW, Meyer DC, Koch PP (2011) Classification of trochlear dysplasia as predictor of clinical outcome after trochleoplasty. Knee Surg Sports Traumatol Arthrosc 19(10):1655–1661
Goutallier D, Raou D, Van Driessche S (2002) Retro-trochlear wedge reduction trochleoplasty for the treatment of painful patella syndrome with protruding trochleae. Technical note and early results. Rev Chir Orthop Reparatrice Appar Mot 88(7):678–685
Horikawa A, Kodama H, Miyakoshi N, Yamada S, Miyamoto S (2011) Recurrent dislocation of the patella accompanying hypotrochlea of the femur and malalignment of the patella. Ups J Med Sci 116(4):285–288
Kobayashi A, Ou A (1994) Condyloplasty of lateral epicondyle of the femur for patellar instability. Seikei-saigaigeka. Orthop Surg Traumatol 37:49–57
Kobayashi A, Toshihiro O (1991) Condyloplastie latérale du fémur pour instabilité fémoro-patellaire. Rev Chir Orthop Reparatrice Appar Mot 77:158
Koch PP, Fuchs B, Meyer DC, Fucentese SF (2011) Closing wedge patellar osteotomy in combination with trochleoplasty. Acta Orthop Belg 77(1):116–121
Maenpaa H, Lehto MU (1997) Patellofemoral osteoarthritis after patellar dislocation. Clin Orthop Relat Res 339:156–162
Masse Y (1978) Trochleoplasty. Restoration of the intercondylar groove in subluxations and dislocations of the patella. Rev Chir Orthop Reparatrice Appar Mot 64(1):3–17
Mulford JS, Wakeley CJ, Eldridge JD (2007) Assessment and management of chronic patellofemoral instability. J Bone Joint Surg Br 89(6):709–716
Murphy JB (1914) Congenital luxation of the patella. In: Clinics of John B. Murphy, vol 1. WB Saunders, USA, pp 817–838
Nelitz M, Dreyhaupt J, Lippacher S (2013) Combined trochleoplasty and medial patellofemoral ligament reconstruction for recurrent patellar dislocations in severe trochlear dysplasia: a minimum 2-year follow-up study. Am J Sports Med 41(5):1005–1012
Ntagiopoulos PG, Byn P, Dejour D (2013) Midterm results of comprehensive surgical reconstruction including sulcus-deepening trochleoplasty in recurrent patellar dislocations with high-grade trochlear dysplasia. Am J Sports Med 41(5):998–1004
Peterson L, Karlsson J, Brittberg M (1988) Patellar instability with recurrent dislocation due to patellofemoral dysplasia. Results after surgical treatment. Bull Hosp Joint Dis Orthop Inst 48(2):130–139
Peterson L, Vasiliades HS (2010) Proximal open trochleoplasty (grooveplasty). In: Zaffagnini S, Dejour D, Arendt E (eds) Patellofemoral pain, instability, and arthritis: clinical presentation, imaging, and treatment, vol 1. Springer, New York, pp 213–224
Pollard B (1891) Old dislocation of patella reduced by intra articular operation. Lancet 1:988
Schottle PB, Fucentese SF, Pfirrmann C, Bereiter H, Romero J (2005) Trochleaplasty for patellar instability due to trochlear dysplasia: a minimum 2-year clinical and radiological follow-up of 19 knees. Acta Orthop 76(5):693–698
Schöttle PB, Schell H, Duda G, Weiler A (2007) Cartilage viability after trochleoplasty. Knee Surg Sports Traumatol Arthrosc 15(2):161–167
Thaunat M, Bessiere C, Pujol N, Boisrenoult P, Beaufils P (2011) Recession wedge trochleoplasty as an additional procedure in the surgical treatment of patellar instability with major trochlear dysplasia: early results. Orthop Traumatol Surg Res 97(8):833–845
Utting MR, Mulford JS, Eldridge JD (2008) A prospective evaluation of trochleoplasty for the treatment of patellofemoral dislocation and instability. J Bone Joint Surg Br 90(2):180–185
Verdonk R, Jansegers E, Stuyts B (2005) Trochleoplasty in dysplastic knee trochlea. Knee Surg Sports Traumatol Arthrosc 13(7):529–533
von Knoch F, Bohm T, Burgi ML, von Knoch M, Bereiter H (2006) Trochleaplasty for recurrent patellar dislocation in association with trochlear dysplasia. A 4- to 14-year follow-up study. J Bone Joint Surg Br 88(10):1331–1335
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ntagiopoulos, P.G., Dejour, D. Current concepts on trochleoplasty procedures for the surgical treatment of trochlear dysplasia. Knee Surg Sports Traumatol Arthrosc 22, 2531–2539 (2014). https://doi.org/10.1007/s00167-014-3013-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-014-3013-6