Abstract
Purpose
In this prospective case control study, the effectiveness of surgical management of irreparable rotator cuff tears in terms of patient’s status and quality of life was evaluated in two groups of patients: one group receiving arthroscopic debridement associated with acromioplasty and bursectomy and the other receiving an arthroscopic partial repair of the rotator cuff tear.
Methods
Sixty-eight patients (47 males and 21 females) undergoing arthroscopic shoulder surgery for massive irreparable rotator cuff tear were enrolled in our study. Patients were divided into two groups: Group AP (debridement associated with acromioplasty and bursectomy) and Group PR (partial repair). Pre- and post-operative range of motion (ROM), modified-UCLA shoulder score and strength measurement were performed. The RC-QOL was used at the time of the last follow-up to assess patients’ perception of their quality of life.
Results
The final follow-up was 7.8 (±2.3, range 5–9) years. ROM measures were significantly increased from pre- to post-operative evaluations, with significant intergroup differences (P < 0.001). The overall modified-UCLA shoulder score showed a mean pre-operative value of 7.6 ± 2.6 (95 % CI 6.7–8.5) for Group AP and 8.6 ± 4.1 (95 % CI 7.0–9.9) (n.s.) for Group PR. The post-operative values at the latest follow-up showed a statistically significant improvement in both groups [21.4 ± 3.7 (95 % CI 20.1–22.7) for Group AP and 28.8 ± 4.2 (95 % CI 27.3–30.2) for Group PR] (P < 0.0001), with a significant intergroup difference (P < 0.0001). The RC-QOL demonstrated a statistically significant difference between the groups [Group AP: 61.8 ± 6.1(95 % CI 59.6–63.9); Group PR: 71.2 ± 9.8 (95 % CI 67.7–74.6)] (P < 0.0002).
Conclusion
Both techniques are effective in reducing patients’ symptoms, with higher functional outcomes for partial repair. However, the choice of which technique to undertake should take into account the patients’ features concerning the acromio-humeral interval and levels of daily activities.
Level of evidence
Therapeutic case–control study, Level III.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Rotator cuff tears (RCT) are common causes of shoulder pain and dysfunction, impairing the quality of life to a similar extent as diabetes mellitus, hypertension, congestive heart failure, myocardial infarction and depression [27, 28, 30]. Despite the great improvements in the surgical management of rotator cuff tears, not all tears are amenable to surgical repair. The natural history of a RCT is the progression of the lesion with fatty degeneration and retraction of the muscular tissue [11, 14, 24, 29, 32, 33]. Although it could be possible in some patients to achieve adequate mobilization of the tissues to try and repair the tear, the clinical results are often unsatisfactory with a high failure rate as demonstrated at magnetic resonance (MRI) or ultrasonography (US) imaging [16]. Long lasting symptoms, small acromio-humeral interval (<5 mm) and high degree of fatty degeneration of the muscle and tendinous tissue are the factors that may prompt to not repair the lesion [26]. Alternative treatments have been investigated to manage an irreparable rotator cuff tear, including non-operative and operative options. The operative options include debridement associated with acromioplasty and bursectomy, partial repair, muscle transfers (latissimus dorsi, pectoralis major) and total reverse and partial joint replacement [10, 19, 23]. In this case–control study, we evaluated the status and quality of life in two groups of patients with massive irreparable rotator cuff tears: one group received an arthroscopic debridement associated with acromioplasty and bursectomy and the other received an arthroscopic partial repair of the rotator cuff tear. The null hypothesis that, in a homogenous group of patients with an arthroscopically confirmed massive irreparable lesion of the rotator cuff, there is no clinical difference between debridement associated with acromioplasty and bursectomy and partial repair was tested.
Materials and methods
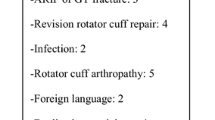
Inclusion criteria were: (1) daily and nocturnal pain, not necessary in a continuous fashion; (2) failure of a 6-month period of conservative measures (NSAIDs, intra-articular injection of corticosteroids and physiotherapy); (3) strength and range of movement (ROM) loss. Exclusion criteria were: (1) prior surgery of the shoulder; (2) severe gleno-humeral arthritis (V degree according to Hamada et al.); (3) cervical radiculopathy; (4) capsulo-ligamentous lesions; (5) inflammatory arthritides; (6) shoulder instability; (7) previous fractures of the glenoid and of the greater and smaller tuberosity. General contraindications to surgery were: cardiovascular diseases (including myocardial infarction, heart disorders, coronary artery disease, pre-operative cardiac procedures, cerebrovascular disease, lower extremity ischaemia, neurological diseases and diabetes) or psychiatric illness.
Sixty-eight patients (47 males and 21 females) who presented to our institution during the period 2002–2006 to undergo arthroscopic shoulder surgery for massive irreparable rotator cuff tear met our inclusion criteria and were prospectively enrolled in our study. The diagnosis was based on for all the patients on clinical exam and confirmed by MRI imaging. The median age at surgery was 62 years (47–76 years) and the median follow-up was 7 years (5–9 years). All patients had non-traumatic, degenerative rotator cuff disease. Patients were divided into two groups: 34 patients (Group AP: 22 men and 12 women) treated with debridement associated with acromioplasty and bursectomy and 34 patients (Group PR: 25 men and 9 women) received a partial repair. The median time between the onset of symptoms and the surgical repair was 10 months (7–13) in the Group AP, and 8 months (4–12) in the Group PR, with no statistically significant difference. The dominant arm was involved in 29 patients in Group AP and in 31 patients in Group PR with no statistically significant difference (n.s.) between the two groups (χ = 0.09). Patients were assessed at baseline immediately before the index operation, and post-operatively for a minimum 5-year follow-up. Clinical and operative details were thoroughly recorded for each patient.
Surgical technique
All surgical procedures were performed by two orthopaedic surgeons comparable for surgical skills and experience: one (RP) performed all Group AP procedures and the other (FF) performed all Group PR procedures. All the patients received a pre-operative interscalene block. All the procedures were performed with the patient in the beach chair position with 8–10 lb of traction applied to the arm to be operated on. Gravity joint irrigation was provided using 4 L saline bags hung at a height of 8 feet. An arthroscopic pump was not used. After careful arthroscopic evaluation of the full-thickness rotator cuff tear through standard posterior and anterior portals, the extent of tear and the tendon retraction were measured intra-operatively in both the coronal and sagittal planes according to the classification system described by Boileau et al. [4]. Biceps tenotomy was performed in all patients of both groups. At acromioplasty, the coraco-acromial ligament was preserved as much as possible in patients of both groups.
Debridement, bursectomy and acromioplasty
Once the rotator cuff lesion was identified, a thorough debridement of the avascular, devitalized tissue of the tendon edge was performed together with a partial synovectomy; attention was then directed to the subacromial space where a standard subacromial decompression was performed. The under surface of the acromioclavicular joint was examined and, if osteophytes or degenerative changes were present, an adequate debridement was undertaken.
Partial repair
After the footprint was identified at the greater tuberosity, it was prepared using a shaver (Arthex, Naples, FL, USA) until a bleeding surface was achieved. We performed a partial repair of the irreparable lesion according to the technique previously described by Burkhart et al. [7].
Post-operative Management
Patients of both groups wore a sling for 4 weeks post-operatively, and they were allowed free flexion and internal rotation from the first post-operative day. At 4 weeks, patients were allowed unrestrained ROM in all directions, while strengthening exercises were started 6–8 weeks after the index surgery. On the first post-operative day, passive external rotation was started, while overhead stretching was allowed 4 weeks post-operatively to avoid damaging the repair. At 4 weeks, the sling was removed, and overhead stretching with a rope and pulley was started. Isoinertial strengthening and strengthening of the deltoid and of the scapular stabilizers were initiated at 6 or 8 weeks after the surgery.
Evaluation
An independent investigator not involved in the surgical management of the patients performed all the outcome assessments. Pre-operative evaluations were performed at the day before surgery, and the results of post-operative evaluation at the final follow-up were recorded at an average of 7.8 years (5–9; SD: ±3; 95 % CI: 26–28). Each patient was evaluated for pre- and post-operative range of motion. Pre- and post-operative modified-UCLA shoulder score and pre- and post-operative measurement of the strength were performed using a handheld dynamometer (PowerTrack MMT; JTech Medical Industries, Alpine, Utah, and Muscletester; Hoggan Health Industries, South Draper, Utah) which measures forces ranging from 4.4 to 445 N in 4.4 N increments. Elevation, external rotation, internal rotation and hand behind back lift-off were assessed. Finally, the RC-QOL [30] was used at the time of the last follow-up to assess patients’ perception of their quality of life.
Imaging
All patients received a standard pre-operative assessment using standard radiographs (antero-posterior projections, neutral, external and internal rotation) and MRI scans. Oblique coronal, oblique sagittal and axial T2-weighted spin-echo MRIs [repetition time (RT): 3,200 ms; echo time (ET): 85 ms] were obtained in all patients. According to Hamada et al. [17], the acromio-humeral interval (AHI) was assessed pre-operatively for each patient (Table 1). Fatty infiltration was evaluated using MRI scans and classified according to Goutallier et al. [15].
Functional assessment
A modified-UCLA rating scale for pain, function, ROM and patient satisfaction was used [22]. Manual assessment of strength was performed in all patients before return to work.
Range of motion
The shoulder range of motion (forward elevation, external rotation and internal rotation) was recorded pre-operatively and starting from the second post-operative month using a goniometer. Measurements were made following standard guidelines [2] in the supine position with the scapula stabilized by anterior pressure on the shoulder against the examining table [2]. The examiner obtained three measurements for each shoulder, and the mathematical mean was used for statistical purposes.
Quality of life (RC-QOL)
The RC-QOL questionnaire is a simple disease-specific outcome measure that evaluates the impact of rotator cuff disease on the general quality of life [15]. This questionnaire has been cross-culturally validated in Italian [30].
Statistical analysis
The statistical test used to analyse the trial was the uncorrected Chi-square test. The data used to design the study were the following: alpha value, 0.05; power, 0.8; ratio between cases and control, 1; probability of the event in cases, 0.3; probability of the event in controls, 0.3. According to the power analysis calculation, a total of 32 patients in each group were needed. Thirty-four patients in each group were recruited. Data are presented using mean, median or standard deviation, 95 % CI, and range and data ranges as appropriate. Statistical analysis was performed with the SPSS software package, version 11.0 (SPSS, Chicago, IL). To analyse non-continuous rated scores, the non-parametric Mann–Whitney U test was used. For scores rated by continuous numbers, the Student’s t test was applied. The significance level was set as P < 0.05. Test–retest reliability data were analysed by intra-class correlation (ICC) for numerical continuous data and the Cohen’s Kappa for nominal scales. Linear regression analysis was performed to investigate the association between the AHI and the modified-UCLA score as well as for fatty infiltration.
Results
Patients were homogeneous for the investigated measures. Pre-operative UCLA values presented no statistically significant differences between the two groups [Group AP 7.6 ± 2.6 (95 % CI 6.7–8.5) Group PR 8.6 ± 4.1 (95 % CI 7.0–9.9) (n.s.)].
Surgical findings
A massive (>5 cm) tear was found in 27 patients in Group AP and 29 in Group PR (mean tear size 52.3 ± 1.6), while 7 patients in Group AP and 5 in Group PR had a large (3–5 cm) tear (mean tear size 38.6 ± 2.3). For massive tears treated with partial repair, the mean decrease in tear size was 14.2 ± 3.1 cm, while for large tear it was 11.3 ± 4.1 cm. The median number of anchors used was 2 (ranging 2–5).
Coexisting lesions were long head biceps tendinopathy in 26 patients of Group AP and 23 in Group PR, all treated with a tenotomy. A Type 2 SLAP lesion, found in 4 patients in Group AP and 5 in Group PR, was repaired using one suture anchor.
Range of motion
The ROM of both groups at the latest follow-up (post-operative forward elevation, internal rotation and external rotation) were significantly improved (P < 0.001) compared with pre-operative values, with significant intergroup differences (external rotation, n.s.; internal rotation, P < 0.0001; forward flexion, P < 0.0001) (Table 2). The test–retest reliability for the ROM measures was 0.89.
Functional assessment
Pain decreased by discharge (on the second post-operative day) for the Group AP and remained stable for all the follow-up period (P < 0.0001). Group PR patients reported no significant differences between pre- and post-operative pain measure for the first post-operative month, but successively pain decreased significantly from the pre-operative period (P < 0.0001). At final follow-up, there were no significant intergroup differences (n.s.). Results from modified-UCLA shoulder score showed at the latest follow-up a statistically significant improvement in both groups (P < 0.0001) (Table 3). Intergroup differences in ROM, function and strength were statistically significantly different (P < 0.0001) starting from the first post-operative month to the whole duration of the study (Table 4). There was a statistically significant improvement in strength between pre-operative evaluation and the last follow-up for patients undergoing partial repair (P < 0.0001), while patients who underwent debridement did not experience significant post-operative strength gains (n.s.). The same was observed with regard to function: patients who underwent partial repair experienced a significant improvement between pre- and post-operative measures (P < 0.0001), while patients who underwent debridement did not improve significantly (n.s.). Post-operatively, average satisfaction scores increased significantly compared with the pre-operative ones for both groups (P < 0.0001) (Table 4). According to the UCLA rating system, 8 patients (33 %) had an excellent result (34–35 points), 13 (54 %) a good result (28–33 points) and 3 (13 %) a fair result (21–27 points) in the Group AP, whereas 9 patients (34 %) had an excellent result (34–35 points), 15 patients (58 %) a good result (28–33 points) and 2 (8 %) a fair result (21–27 points) in the Group PR. There were no poor results (0–20 points). There was evidence of a negative association between the AHI and the modified-UCLA score (β = −0.87 for Group AP; β = −0.83 for Group PR) and fatty infiltration stage (β = −0.79 for Group AP; β = −0.74 for Group PR) and tear size (β = −0.66 for Group AP; β = −0.72 for Group PR). Moreover, manual workers, who were considered as high demand, reported worse outcomes compared with non-manual workers: 24.2 ± 2.7 for workers and 31.8 ± 3.5 for non-workers, at the 2-year follow-up (P < 0.001), and 21.9 ± 4.3 for manual workers and 29.3 ± 3.2 for non-manual workers at the last follow-up. The test–retest reliability for the UCLA shoulder score was 0.91.
Quality of life (RC-QOL)
The Group PR achievel statistically significant better result then the Group AP at RC-QOL scores (P < 0.0001) (Table 3).
Discussion
The most important finding in this study is that both techniques, with the association of biceps tenotomy, reduced patients’ complaints with regard to pain and shoulder function. However, the finding that higher functional outcomes are achieved from the partial repair technique compared with the debridement associated with acromioplasty and bursectomy goes against our null hypothesis. Moreover, outcomes are comparable with those of the currently available literature [7, 8, 12, 25]. For the overall cohort, both techniques decreased shoulder pain improving patients’ quality of life. When considering the first three post-operative months, patients treated with debridement only experienced less pain compared with patients who underwent partial repair. In particular, in the debridement group, pain measures decreased immediately after surgery maintaining the same poor values for all the follow-up period. On the contrary, patients who underwent partial repair continued to experience a painful shoulder, especially with nocturnal pain for the first post-operative month that required higher NSAIDs consumption. In concomitance with the full passive shoulder mobilization (since the second post-operative month), pain measures decreased settling to a slightly higher but not statistically significant value compared with the debridement group. This may result from the tissue tensioning consequent to the partial repair of the rotator cuff. Consistently with other authors [3, 6–8, 31], we noticed different outcomes among the two groups of patients with regard to ROM measures and to strength and function domains of the UCLA shoulder. These differences may be due to the ability of the partial repair to restore the functional anatomy of the shoulder, allowing a near-to-normal arc of movement, strength and function. Since the first post-operative assessment (at the 6th post-operative month), strength measures increased in patients who underwent a partial repair, maintaining a stable value at the last follow-up. On the contrary, patients who underwent debridement did not show any increase in strength, maintaining the same pre-operative values. These findings support the theory that partial repair of irreparable rotator cuff lesions leads to improved shoulder biomechanics. The first to propose this concept were Burkhart et al. [7], who noticed that some patients, despite a large rotator cuff tear, maintained a normal shoulder function. This was possible because, despite the lesion of the tendons, the coronal and axial forces of the glenohumeral joint were still balanced. It seemed logical to the author that, in patients with massive dysfunctional rotator cuff tears, it would be possible to restore shoulder function by repairing rotator cuff enough to achieve a functional tear, that is, a tear in which the forces and moments between the anterior and posterior aspect of the shoulder are balanced [6]. Two negative prognostic factors were noticed: the AHI and the patients’ daily activity levels. Pre-operatively both parameters were assessed, but they did not affect the treatment choice. During the follow-up period, the worst outcomes were related to grade 2 or superior acromio-humeral interval and to high-demand patients. Based on these findings, for patients with a pre-operative AHI grade 2 or higher, partial repair will not bring any gain in terms of shoulder function and strength compared with debridement associated with long head biceps tenotomy. Therefore, the best outcomes could be reached without any attempt at repair. Moreover, for patients with high daily activity levels the partial repair technique will not improve enough shoulder function, making it necessary to consider a reverse total shoulder arthroplasty or a tendon transfer.
Post-operative outcomes of this investigation are comparable with those of the available literature. In a study on 24 patients with massive rotator cuff tear undergoing partial repair, Duralde and Bair [8] reported that 67 % of patients showed good to excellent results at ASES score, and 92 % of patients were subjectively satisfied with the results of surgery. In the study by Berth et al. [3], patients with massive rotator cuff tear received either debridement or a partial repair. Post-operatively, both groups demonstrated highly significant improvements compared with pre-operative values, and the overall Constant score in the partial repair group was superior to the outcome in the debridement group. A recent report comparing pre- to post-operative results in a case series of 27 patients undergoing partial repair [20] showed that all shoulder (simple shoulder test, Constant and UCLA score) scores showed a significant improvement.
Iagulli et al. [18] compared two groups of patients, one in which a complete cuff repair was achieved, and the other in whom only a partial repair was possible. Forty-one patients with only partial repair achieved a post-operative mean UCLA score of 29.49, and 45 patients with complete repair achieved a mean UCLA score of 29.64: no statistically significant differences in post-operative outcomes were noted.
Further alternative and effective treatment options for the management of massive irreparable tear are available: Fenlin et al. [9] proposed the “tuberoplasty”, that is, the creation of a new articulation between the acromion and the humeral head. With this technique, 95 % of 20 patients were satisfied at the UCLA shoulder score, and 68 % were completely free from pain. Lee et al. [21] reported on 32 patients treated with arthroscopic decompression and tuberoplasty showing significant improvement in post-operative Constant and UCLA shoulder scores. Gerber et al. [13] showed significant improvement in subjective shoulder value and Constant scores in 68 patients with massive rotator cuff tear receiving a latissimus dorsi transfer.
Despite the promising results of these techniques, partial repair has been preferred: this technique is relatively simple, does not require additional surgical steps and can be performed arthroscopically.
Results from post-operative assessment demonstrate that both the debridement alone and partial repair are effective in markedly reducing pain. This effect could explain why a high rate of patient’s satisfaction and no poor results were achieved. In addition, since any post-operative assessment based on MRI or ultrasonography was not performed, it is not possible to report the rate of partial repair failure or tear progression among the investigated patients. However, there is only a weak correlation between the status of the rotator cuff tendons and the functional performances of patients [1, 5, 34].
Strengths of the study are that all post-operative investigations were performed by an independent assessor, and no patients were lost during the follow-up. Also, standardized and validated scales were used, and data were collected prospectively. On the other hand, partial repair is a salvage procedure, and represents an attempt to restore at least some of the functional anatomy of the rotator cuff. Debridement is only a symptomatic approach. For this reason, partial repair should be compared with other techniques that aim to restore rotator cuff function such us latissimus dorsi transfer or shoulder arthroplasty.
This study has several limitations. Firstly, two surgeons were involved in the study, one per each surgical technique. However, they were both fully trained and fully conversant with the technique they were undertaking. Moreover, the mean patients’ age is relatively high. Therefore, the high rate of patients’ satisfaction could be masked by the fact that an elderly population has lower functional needs. A younger and more active study population would have other requirements, but those patients would likely wish a treatment plan more effective in restoring shoulder function, such as a tendon transfer. Also, the follow-up period, although with an average of nearly 8 years, could not be long enough to detect a clinically relevant deterioration of the positive surgical effects. Finally, a post-operative shoulder MRI or ultrasonography was not performed; therefore, it is not possible to establish the rate of tear progression for Group AP, of re-tear for Group PR, and changes in fatty infiltration for both groups.
Conclusion
This study demonstrated that the post-operative outcomes of both techniques are largely comparable. However, since partial repair leads to higher functional outcomes, in everyday clinical work repair should at least be attempted to obtain better functional results and reduction in pain.
References
Ainsworth R (2006) Physiotherapy rehabilitation in patients with massive, irreparable rotator cuff tears. Musculoskeletal Care 4(3):140–151
American Academy of Orthopaedic Surgeons (1965) Joint motion. Method of measuring and recording. Churchill Livingstone, Edinburgh
Berth A, Neumann W, Awiszus F, Pap G (2010) Massive rotator cuff tears: functional outcome after debridement or arthroscopic partial repair. J Orthop Traumatol 11(1):13–20
Boileau P, Brassart N, Watkinson DJ, Carles M, Hatzidakis AM, Krishnan SG (2005) Arthroscopic repair of full-thickness tears of the supraspinatus: does the tendon really heal? J Bone Joint Surg Am 87(6):1229–1240
Bokor DJ, Hawkins RJ, Huckell GH, Angelo RL, Schickendantz MS (1993) Results of nonoperative management of full-thickness tears of the rotator cuff. Clin Orthop Relat Res 294:103–110
Burkhart SS (1997) Partial repair of massive rotator cuff tears: the evolution of a concept. Orthop Clin North Am 28(1):125–132
Burkhart SS, Nottage WM, Ogilvie-Harris DJ, Kohn HS, Pachelli A (1994) Partial repair of irreparable rotator cuff tears. Arthroscopy 10(4):363–370
Duralde XA, Bair B (2005) Massive rotator cuff tears: the result of partial rotator cuff repair. J Shoulder Elbow Surg 14(2):121–127
Fenlin JM Jr, Chase JM, Rushton SA, Frieman BG (2002) Tuberoplasty: creation of an acromiohumeral articulation-a treatment option for massive, irreparable rotator cuff tears. J Shoulder Elbow Surg 11(2):136–142
Franceschi F, Papalia R, Palumbo A, Del Buono A, Maffulli N, Denaro V (2012) Operative management of partial- and full-thickness rotator cuff tears. Med Sport Sci 57:100–113
Franceschi F, Papalia R, Palumbo A, Vasta S, Maffulli N, Denaro V (2011) Management of postoperative shoulder stiffness. Sports Med Arthrosc 19(4):420–427
Gartsman GM (1997) Massive, irreparable tears of the rotator cuff. Results of operative debridement and subacromial decompression. J Bone Joint Surg Am 79(5):715–721
Gerber C, Maquieira G, Espinosa N (2006) Latissimus dorsi transfer for the treatment of irreparable rotator cuff tears. J Bone Joint Surg Am 88(1):113–120
Goutallier DBJ, Patte D (1990) Assessment of the trophicity of the muscles of the ruptured rotator cuff by CT scan. In: Post M, Morrey BF, Hawkins RJ (eds) Surgery of the shoulder. Mosby, St Louis, pp 11–13
Goutallier D, Postel JM, Bernageau J, Lavau L, Voisin MC (1994) Fatty muscle degeneration in cuff ruptures. Pre- and postoperative evaluation by CT scan. Clin Orthop Relat Res 304:78–83
Goutallier D, Postel JM, Gleyze P, Leguilloux P, Van Driessche S (2003) Influence of cuff muscle fatty degeneration on anatomic and functional outcomes after simple suture of full-thickness tears. J Shoulder Elbow Surg 12(6):550–554
Hamada K, Yamanaka K, Uchiyama Y, Mikasa T, Mikasa M (2011) A radiographic classification of massive rotator cuff tear arthritis. Clin Orthop Relat Res 469:2452–2460
Iagulli ND, Field LD, Hobgood ER, Ramsey JR, Savoie FH 3rd (2012) Comparison of partial versus complete arthroscopic repair of massive rotator cuff tears. Am J Sports Med 40(5):1022–1026
Khair MM, Gulotta LV (2011) Treatment of irreparable rotator cuff tears. Curr Rev Musculoskelet Med 4(4):208–213
Kim SJ, Lee IS, Kim SH, Lee WY, Chun YM (2012) Arthroscopic partial repair of irreparable large to massive rotator cuff tears. Arthroscopy 28(6):761–768
Lee BG, Cho NS, Rhee YG (2011) Results of arthroscopic decompression and tuberoplasty for irreparable massive rotator cuff tears. Arthroscopy 27(10):1341–1350
Longo UG, Vasta S, Maffulli N, Denaro V (2011) Scoring systems for the functional assessment of patients with rotator cuff pathology. Sports Med Arthrosc 19(3):310–320
Merolla G, Saporito M, Porcellini G (2011) Conservative management of rotator cuff tears: literature review and proposal for a prognostic prediction score Muscle. Ligament and Tendons Journal 1(1):12–19
Nakagaki K, Ozaki J, Tomita Y, Tamai S (1996) Fatty degeneration in the supraspinatus muscle after rotator cuff tear. J Shoulder Elbow Surg 5(3):194–200
Ogilvie-Harris DJ, Demaziere A (1993) Arthroscopic debridement versus open repair for rotator cuff tears. A prospective cohort study. J Bone Joint Surg Br 75(3):416–420
Oh JH, Kim SH, Ji HM, Jo KH, Bin SW, Gong HS (2009) Prognostic factors affecting anatomic outcome of rotator cuff repair and correlation with functional outcome. Arthroscopy 25(1):30–39
Osti L, Papalia R, Del Buono A, Denaro V, Maffulli N (2010) Comparison of arthroscopic rotator cuff repair in healthy patients over and under 65 years of age. Knee Surg Sports Traumatol Arthrosc 18(12):1700–1706
Ostor AJ, Richards CA, Prevost AT, Speed CA, Hazleman BL (2005) Diagnosis and relation to general health of shoulder disorders presenting to primary care. Rheumatology (Oxford) 44(6):800–805
Papalia R, Franceschi F, Vasta S, Gallo A, Maffulli N, Denaro V (2012) Shoulder stiffness and rotator cuff repair. Br Med Bull [Epub ahead of print]
Papalia R, Osti L, Leonardi F, Denaro V, Maffulli N (2010) RC-QOL score for rotator cuff pathology: adaptation to Italian. Knee Surg Sports Traumatol Arthrosc 18(10):1417–1424
Porcellini G, Castagna A, Cesari E, Merolla G, Pellegrini A, Paladini P (2011) Partial repair of irreparable supraspinatus tendon tears: clinical and radiographic evaluations at long-term follow-up. J Shoulder Elbow Surg 20(7):1170–1177
Steinbacher P, Tauber M, Kogler S, Stoiber W, Resch H, Sanger AM (2010) Effects of rotator cuff ruptures on the cellular and intracellular composition of the human supraspinatus muscle. Tissue Cell 42(1):37–41
Wildemann BKF (2011) Biological aspects of rotator cuff healing Muscle. Ligament and Tendons Journal 1(4):160–167
Zingg PO, Jost B, Sukthankar A, Buhler M, Pfirrmann CW, Gerber C (2007) Clinical and structural outcomes of nonoperative management of massive rotator cuff tears. J Bone Joint Surg Am 89(9):1928–1934
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Franceschi, F., Papalia, R., Vasta, S. et al. Surgical management of irreparable rotator cuff tears. Knee Surg Sports Traumatol Arthrosc 23, 494–501 (2015). https://doi.org/10.1007/s00167-012-2317-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-012-2317-7