Abstract
Purpose
The aim of our study was to evaluate knee rotational laxity and proprioceptive function 2 years after partial anterior cruciate ligament (ACL) reconstruction. According to our hypothesis, partial ACL reconstruction could restore knee laxity and function to the intact level.
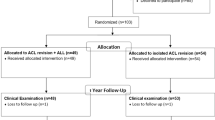
Methods
We conducted a study in fifteen consecutive patients undergoing partial ACL reconstruction. Fifteen anteromedial bundle tears were identified intraoperatively. Partial ACL reconstructions were performed by the same senior surgeon using a single-incision technique. A bone–patellar tendon–bone graft was used in 13 cases and a double-stranded semitendinosus graft in 2 cases of chronic patellar tendonitis. The mean age at surgery was 29 years. The time between ACL tear and surgery averaged 7.8 months (range 2.5–29.5 months).
We developed an original device designed to assess knee proprioception (passive and active) and measure weight-bearing rotational laxity in full extension and at 30°, 60° and 90° of knee flexion. All measurements were taken on both the reconstructed and healthy knee.
Results
The mean follow-up of the study was 3.4 years (range 2.6–4.4). No statistically significant difference in rotational laxity, active or passive proprioception could be observed between the reconstructed and healthy knee. External rotation was significantly greater than internal rotation in full extension and at 30° of flexion in the reconstructed and the healthy knee (P < 0.05). For each knee, active proprioception was found to be significantly different (higher) than passive proprioception (P < 0.05).
Conclusion
Our study did not detect any difference in rotational laxity and proprioception between the reconstructed and the healthy knee. Therefore, partial ACL reconstruction appears to restore satisfactory knee laxity and function in case of partial ACL tear.
Level of evidence
IV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Proprioception is a major mechanism contributing to knee stability and function. Knee injury, such as tear of the anterior cruciate ligament (ACL), causes changes in proprioception, thus acting as a crucial element during rehabilitation. Partial ACL tears may account for up to 1/3 of all ACL tears. During standard ACL reconstruction, the remnants of the ACL insertion sites are usually resected to avoid overstuffing the intercondylar notch. However, preservation of the ACL insertion fibers that remain in continuity after ACL partial tears is advocated since these fibers may have the potential to produce collagen [13].
There are several available methods used to measure knee proprioception and quantify rotational knee laxity in vivo and in vitro but all have their own limitations leading to approximations regarding measurement accuracy and exhaustiveness [4, 5, 12]. Opto-electronic kinematic analysis of the knee joint has already proved useful in assessing patients with a knee prosthesis. In order to investigate the various factors involved in healthy and ACL-deficient knees, the authors developed an original system for in vivo kinematic analysis of knee proprioception and rotational laxity.
The objective of our study was to analyze knee rotational laxity and proprioceptive function 2 years after partial ACL reconstruction. We hypothesized that partial ACL reconstruction would restore knee laxity and function to the intact level.
Materials and methods
We conducted a study in 15 consecutive patients undergoing partial ACL reconstruction in 2007. The mean age at surgery was 29 years (range 16.7–47). The mean time between ACL tear and surgery was 7.8 months (range 2.5–29.5).
Surgical procedure
Partial ACL reconstructions were performed by the same senior surgeon using the single-incision technique. The mean operative time was 70 min (range 42–108).
A standard lateral parapatellar portal was created for the arthroscope, while the instruments were introduced through a medial parapatellar portal. Arthroscopic evaluation included complete joint assessment and thorough exploration of the ACL lesion. Fifteen anteromedial (AM) bundle tears were diagnosed intraoperatively. The objective was to obtain a 7- to 8-mm-diameter graft for the reconstruction of the AM bundle to avoid overstuffing the intercondylar notch. A bone–patellar tendon–bone transplant was used in 13 cases, and a double-stranded semitendinosus graft in 2 cases of chronic patellar tendonitis.
The graft was fixed to the femur by means of a bioabsorbable screw and secured to the tibia using a bioabsorbable screw combined with a postfixation staple in case of double-stranded semitendinosus graft.
The postoperative rehabilitation protocol was similar to that used after standard ACL reconstruction.
Experimental system (Fig. 1)
We developed a new system designed to assess knee rotational laxity and proprioception. The device was made of a Polaris® System (Northern Digital Inc., Ontario, Canada) (Fig. 2) (optical tracking system that measures the 3D positions of the passive markers) and a portable workstation integrating the new data acquisition software. A tripod composed of 3 passive markers was placed on the thigh and leg of each patient.
A calibration procedure was carried out prior to each measurement. The full extension and neutral rotation positions of the knee could then be determined. Passive and active proprioception as well as rotational laxity was evaluated on both the reconstructed and healthy knee. The software enabled the clinician to visualize the real-time data displayed on the screen (Fig. 1). These data were then saved and stored in the patient record in our institution for further evaluations.
Measurement of rotational laxity (Fig. 2)
Internal and external rotations under weight-bearing conditions were evaluated with the knee in full extension and at 30° of flexion. Measurement started with the patient in the standing position and the knee in full extension with both feet separated by 20 cm in neutral rotation. The first stage consisted in resetting the system and proceeding with calibration. Then, the patient was asked to achieve maximal internal trunk rotation and return to the neutral position. Finally, the patient was asked to achieve maximal external trunk rotation and return to the neutral position. This acquisition sequence was repeated 5 times. The test was also performed at 30° of knee flexion while the patient could control on the screen the accuracy of the flexion angle during internal and external rotations.
Measurement of proprioception (Fig. 1)
The evaluation was performed with the patient in a sitting position on the edge of the table, the knee relaxed at 90° of flexion. The calf and the foot were allowed to hang freely. The patient was blindfolded during the test. For the evaluation of active proprioception, the patient was instructed to reproduce a knee flexion angle of 30°, 60°, then 90° (angle reproduction test). For the evaluation of passive proprioception, the clinician held the foot of the patient in the neutral position while bending his knee. The patient was asked to say “stop” when he thought his knee was flexed at 30°, 60° and 90°. Proprioception was evaluated three times with the knee flexed at 30°, 60°, then 90°. The mean value of the three successive tests was recorded.
Statistical analysis
The nonparametric Wilcoxon test for paired samples was used to compare parameters from the evaluations using commercial software (JMP 7.0, SAS Campus Drive, North Carolina, USA). Statistical significance was set to P < 0.05.
Results
The mean postoperative follow-up was 3.4 years (range 2.6–4.4). The mean clinical evaluation time for each patient using our new device was 15 min.
We did not find any statistically significant difference in rotational laxity and active or passive proprioception between reconstructed and healthy knees (Tables 1, 2). External-rotation laxity was found to be significantly greater than internal-rotation laxity in full extension and at 30° of knee flexion in reconstructed and healthy knees (P < 0.05). For each knee, active proprioception was found to be statistically different (higher) than passive proprioception (P < 0.05).
Discussion
At last follow-up, the most important finding of the present study was that proper restoration of knee laxity and function was observed for the reconstructed knee with respect to the healthy knee. To our knowledge, this is the first study on rotational laxity and proprioception evaluation after partial ACL reconstruction.
ACL reconstruction is usually advocated for active patients to restore knee stability. However, in most cases, the authors focused on the mechanical properties of the graft rather than on the postoperative proprioceptive function of the operated knees. Adachi [2] reported the results of a study including 40 patients with a mean follow-up of 3.2 years after partial ACL reconstruction. He compared these results with those obtained after standard ACL reconstruction and found a statistically significant difference regarding the maxi manual postoperative laxity when using the KT-2000™ system. Adachi [2] also reported a statistically significant difference in proprioception between the two groups (a 0.7° mispositioning after partial ACL reconstruction and 1.7° after complete ACL repair). In another study, Adachi [1] established a correlation between the number of mechanoreceptors and proprioception.
Gobbi [8] did not find any difference in knee laxity and function between the double-bundle and single-bundle ACL reconstruction techniques. Measurement of knee proprioception may be achieved using various methods: the reflex hamstring contraction latency using electromyography (EMG) [3], the threshold to detect passive motion (TTDPM) [4, 5, 12], the joint position sense and the method used in our study [5, 12]. Proprioception seems to be strongly correlated with knee joint function and risk of instability [3]. According to Salvator-Vitwoet, the graft used in ACL reconstruction was poorly innervated unlike the native ACL. However, the mechanoreceptors of both the joint and the capsule have been shown to be crucial for postoperative recovery of knee proprioception [9, 11]. High-level athletes with chronic ACL deficiency reported improved knee function after strapping, although the biomechanical effects of this method are still unknown. In these cases, stimulation of skin mechanoreceptors could contribute to the improvement of knee proprioception. In our study, knee proprioception after partial ACL reconstruction was similar to that of the healthy knee. Ochi [10] has already reported the decline in proprioception in ACL-deficient knees and the postoperative improvement after ACL reconstruction. In our study, there was no significant difference in passive proprioception during flexion, whereas Fremerey [6] reported a loss of proprioception between 80° and 100° of knee flexion. Finally, the assessment of proprioception appears to be complex. However, as the pivot shift test and the Lachman test, it should be part of the knee evaluation before and after ACL reconstruction.
Furman [7] reported an increase in rotational laxity (>6°) after ACL section within the frame of a cadaver study that correlated the findings of Zaffagnini [14] in a study conducted in animals. In our study, at last follow-up, internal (10°) and external (14°) rotational laxity was not statistically different between the reconstructed and the healthy knee in full extension and at 30° of flexion.
The limitations of our study include the lack of preoperative evaluation and the relatively small sample of patients. Biases were reported in our study. The measurements were taken manually, which may have caused stimulation of skin mechanoreceptors and affect proprioception. In others studies, a leg support was used to compensate for this drawback. Corrigan [5] used a tourniquet during a 2-month period prior to the measurements in order to suppress any cutaneous information. In our study, patients were seated on the edge of a table, which may have modified joint position sense despite the absence of any contact around the knee. The main limitations were the use of skin markers and the potential risk of marker displacement during knee flexion. Despite the use of a strong fixation placed close to the knee, this drawback could not be completely avoided. However, this proprioception evaluation protocol has been validated and appears to have been correlated with the number of mechanoreceptors [1]. The main strength of our study was the use of our new system specifically designed for postoperative measurement of knee rotational laxity and proprioception under weight-bearing conditions after partial ACL reconstruction.
This new system could have a broad range of clinical applications since it provides accurate, reproducible and rapid measurements. In vitro, this protocol could allow kinematic evaluation of the knee prior to and after any ligamentous section (such as the ACL). In vivo, this protocol could provide easy postoperative analysis of ACL reconstructions (single or double bundle) and also be used for the assessment of various total knee prosthesis designs (fixed or mobile bearing, posterior-stabilized or cruciate retaining TKAs …).
Conclusion
Our study, based on an original system specifically designed to assess knee kinematics, did not exhibit any difference in rotational laxity and proprioception between the reconstructed and the healthy knee. According to our findings, partial ACL reconstruction could provide satisfactory recovery of knee laxity and function in the management of partial ACL tears, which confirms our hypothesis.
References
Adachi N, Ochi M, Uchio Y, Iwasa J, Ryoke K, Kuriwaka M (2002) Mechanoreceptors in the anterior cruciate ligament contribute to the joint position sense. Acta Orthop Scand 73(3):330–334
Adachi N, Ochi M, Uchio Y, Sumen Y (2000) Anterior cruciate ligament augmentation under arthroscopy. A minimum 2-year follow-up in 40 patients. Arch Orthop Trauma Surg 120(3–4):128–133
Beard DJ, Kyberd PJ, Fergusson CM, Dodd CA (1993) Proprioception after rupture of the anterior cruciate ligament. An objective indication of the need for surgery? J Bone Joint Surg Br 75(2):311–315
Boerboom AL, Huizinga MR, Kaan WA, Stewart RE, Hof AL, Bulstra SK, Diercks RL (2008) Validation of a method to measure the proprioception of the knee. Gait Posture 28(4):610–614
Corrigan JP, Cashman WF, Brady MP (1992) Proprioception in the cruciate deficient knee. J Bone Joint Surg Br 74(2):247–250
Fremerey RW, Lobenhoffer P, Zeichen J, Skutek M, Bosch U, Tscherne H (2000) Proprioception after rehabilitation and reconstruction in knees with deficiency of the anterior cruciate ligament: a prospective, longitudinal study. J Bone Joint Surg Br 82(6):801–806
Furman W, Marshall JL, Girgis FG (1976) The anterior cruciate ligament. A functional analysis based on postmortem studies. J Bone Joint Surg Am 58(2):179–185
Gobbi A, Mahajan V, Karnatzikos G, Nakamura N (2011) Single- versus double-bundle ACL reconstruction: is there any difference in stability and function at 3-year followup? Clin Orthop Relat Res [Epub ahead of print]
Hewett TE, Paterno MV, Myer GD (2002) Strategies for enhancing proprioception and neuromuscular control of the knee. Clin Orthop Relat Res 402:76–94
Ochi M, Iwasa J, Uchio Y, Adachi N, Sumen Y (1999) The regeneration of sensory neurones in the reconstruction of the anterior cruciate ligament. J Bone Joint Surg Br 81(5):902–906
Rozzi SL, Lephart SM, Gear WS, Fu FH (1999) Knee joint laxity and neuromuscular characteristics of male and female soccer and basketball players. Am J Sports Med 27(3):312–319
Skinner HB, Barrack RL, Cook SD (1984) Age-related decline in proprioception. Clin Orthop Relat Res 184:208–211
Sonnery-Cottet B, Lavoie F, Ogassawara R, Scussiato RG, Kidder JF, Chambat P (2010) Selective anteromedial bundle reconstruction in partial ACL tears: a series of 36 patients with mean 24 months follow-up. Knee Surg Sports Traumatol Arthrosc 18(1):47–51
Zaffagnini S, Martelli S, Falcioni B, Motta M, Marcacci M (2000) Rotational laxity after anterior cruciate ligament injury by kinematic evaluation of clinical tests. J Med Eng Technol 24(5):230–236
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chouteau, J., Testa, R., Viste, A. et al. Knee rotational laxity and proprioceptive function 2 years after partial ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 20, 762–766 (2012). https://doi.org/10.1007/s00167-012-1879-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-012-1879-8