Abstract
Improvement in motor function after anterior cruciate ligament (ACL) injury is achieved by appropriate rehabilitation. However, it has been questioned whether training after injury can lead to sensory improvement. We hypothesized that motor function can be restored after unilateral non-reconstructed ACL injury, whereas the sensory function cannot, i.e., there would be no difference in functional performance or knee muscle strength between subjects with ACL injury and uninjured controls, but the subjects with ACL injury would have poorer kinesthesia than the uninjured controls. This is a Cross-Sectional Study, wherein 56 (20 women and 36 men) individuals with unilateral non-reconstructed ACL injury were assessed at a mean of 15 years (SD 1.4 years) after the initial injury. All patients initially underwent rehabilitation and were advised to modify their activity level, in order to cope with the ACL insufficiency. At 15 years, they had good subjective function and acceptable activity level. Twenty-eight (14 women and 14 men) uninjured subjects served as controls. Patients and controls were assessed with the one-leg hop test for distance, isometric and isokinetic knee muscle strength, and kinesthesia (the threshold to detection of passive motion). The individuals with ACL injury had the same or better functional performance, measured by the one-leg hop test for distance, and knee muscle strength compared with the uninjured controls. Kinesthesia was poorer in the patient group than in the control group. The results indicate that motor function can be restored but that the sensory function is persistently disturbed after ACL injury.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
An anterior cruciate ligament (ACL) injury leads to defective passive joint stability and defective neuromuscular function. The sensorimotor system covers the whole process from a sensory stimulus to muscle activation. Sensory information from mechanoreceptors in structures in and around the injured joint plays an important role in joint stability [14, 29]. Due to the loss of mechanoreceptors after the injury, the sensory system is disturbed [9], with possible effects on neuromuscular function.
Improvements in neuromuscular function are achieved by appropriate rehabilitation, and observed at short-term follow-up (less than 2 years after injury and treatment) [17, 22], with persistent effects at long-term follow-up (more than 5 years after injury) [2, 18, 28]. Various methods of assessing the motor aspect of neuromuscular function, e.g., muscle strength, functional performance, and movement and muscle activation patterns, are frequently included in studies on treatment after ACL injury, whereas methods of assessing sensory function, e.g., proprioceptive acuity, are rarely included [22]. Moreover, it has been questioned whether training after injury can lead to proprioceptive improvement, although improvement in motor function can be obtained [5].
Two common measures of proprioception are kinesthesia, e.g., the threshold to detection of a passive motion (TDPM), and joint position sense (JPS), e.g., the active reproduction test. The TDPM is the most established test, is more reliable, and more sensitive in detecting differences between groups, such as between patients with ACL injury and uninjured controls, than measures of JPS [9].
The uninjured leg is often used as the control in studies on neuromuscular function after ACL injury. However, various methods of assessing neuromuscular function have shown that both legs are affected after a unilateral ACL injury [4, 15, 24, 33, 35], possibly due to physical inactivity, inherently poor function, disturbed sensory feedback from the injured joint with an effect also in the uninjured side [14], and/or modification of central motor programs following the loss of knee mechanoreceptors after the injury [7, 34]. It is, therefore, important to compare patients with a control group of uninjured subjects to ensure detection of impairment.
The purpose of the present study was to evaluate motor function, measured by functional performance and knee muscle strength, and sensory function, measured by kinesthesia, in individuals with unilateral non-reconstructed ACL injury, in comparison with uninjured individuals. We hypothesized that motor function can be restored after ACL injury, whereas sensory function cannot, i.e., there would be no difference in functional performance or knee muscle strength between the groups, but the subjects with ACL injury would have poorer kinesthesia than the uninjured subjects.
Subjects and methods
Patients and controls
Sixty-seven patients with unilateral non-reconstructed ACL injury, at a mean of 15 years (SD 1.4 years) after the initial injury, were included in the study. They were all from a cohort of 100 consecutive patients with ACL injury at a non-professional, recreational or competitive, activity level, who had been followed prospectively and regularly for 3 years [4, 8, 36, 37], and finally at 15 years after the initial injury [2, 16].
Inclusion criteria when the patients entered the study 15 years ago were: (1) age between 15 and 45 years; (2) acute knee trauma to a previously normal knee, with complete ACL rupture, with or without associated lesions; and (3) an uninjured contralateral extremity. Patients on a professional athletic level (i.e., a Tegner score of 10) and not willing to risk a decrease in activity level (n < 5), those who specifically requested a primary ligament reconstruction (n = 2–3), those with fracture seen on radiographs, or those with psycho-social disorders were excluded. The diagnosis was verified in all patients by stability testing and arthroscopy, by the same orthopedic surgeon (TF), within 10 days of injury. Thirty-one patients had injured their right knee (8 women) and 25 their left knee (12 women). Five of the 56 subjects (1 woman and 4 men) had radiographic osteoarthritis (OA) [2]. A detailed description of patient recruitment, and the patients’ knee injuries (e.g., number of patients with isolated ACL injury, and associated lesions) has been given elsewhere [16, 36, 37].
All patients initially underwent rehabilitation and were advised to modify their activity level in order to cope with the ACL insufficiency. The aim of the initial treatment was to achieve good knee function without discomfort or lack of confidence in the knee, on a satisfactory activity level from the patient’s perspective, and to reduce the risk of new injuries and degenerative changes in the longer perspective. The intention was to treat the patients without primary reconstructive surgery. Patients in doubt were actively encouraged not to undergo primary ACL reconstruction. All patients underwent rehabilitation, with the overall aim of regaining joint mobility and restoring muscle function [37]. The majority of the patients underwent neuromuscular training, supervised by physical therapists specializing in knee injury training [36]. Training started within a week of arthroscopy and continued for 5–8 months. This training method, which has been described in detail elsewhere [2, 37, 38], is based on biomechanical and neuromuscular principles, with the aim of improving neuromuscular control and achieving compensatory functional stability (leg, hip, and trunk muscles). Depending on the perceived instability, the patients were advised to modify their activities in order to cope with the ACL insufficiency. All patients were advised to avoid contact sports, particularly soccer, basketball and team handball. Patients with more than one significant re-injury, who would not accept a further prophylactic decrease in activity level, or those with a symptomatic reparable meniscal tear, were advised to undergo ACL reconstruction. Reconstructed patients were subsequently excluded, since the treatment model without reconstruction had not succeeded, i.e., these patients were regarded as treatment failures [16, 36].
Six of the 100 patients were lost to the 15-year follow-up (four had moved abroad and two did not reply). Sixty-seven subjects (71%) still had a unilateral non-reconstructed ACL injury, 22 (23%) subjects had undergone ACL reconstruction, and 6 (6%) had sustained an ACL injury to the contralateral knee (one of these patients had also undergone reconstructive surgery) [16]. Fifty-six (20 women and 36 men) of the 67 subjects with unilateral non-reconstructed ACL injury at the 15-year follow-up attended the assessment of neuromuscular function [2]. These 56 subjects were considered to be a representative sample of the 67 subjects with unilateral ACL injury; the 11 patients lost to follow-up have been described in detail previously [2].
Twenty-eight uninjured volunteers (14 men and 14 women) with no major orthopedic lesions, or neurological pathology constituted the control group. The patients’ and uninjured subjects’ age, height, weight, Tegner activity level scale [31], Lysholm knee score [31], and KOOS [27] are given in Table 1. No significant differences were found between the subjects with ACL injury and the uninjured controls in age, height, weight, or Tegner activity level scale. The patients had significantly lower Lysholm score (P < 0.001) and KOOS scores (P ≤ 0.001) than the uninjured controls. The patients’ KOOS scores did not differ from the reference values of an age- and gender-matched population-based group [19].
The Research Ethics Committee of Lund University approved the study. All subjects gave their written informed consent to participate in the study.
Assessment
One-leg hop test for distance
The one-leg hop test with the arms free, aiming at a more functional execution of the hop, was used [36]. The subjects were told to hop as far as possible, taking off and landing on the same foot, maintaining their balance for about 2–3 s. The test was performed three times with each leg, alternating the right and left leg, the hop distance being measured from toe to toe. A trial one-leg hop preceded the measurements. The subjects wore shoes, e.g., sneakers. The best value of the three hops was used in the analysis. The reliability of this test is high in uninjured subjects (ICC 0.96) [3], (ICC 0.92) [20] and in individuals with ACL injury (ICC 0.89) [20].
Knee muscle strength
Measurements of isometric and concentric isokinetic strength of the knee muscles, used and described in detail previously in the patient group [2], were performed with a Biodex Multi-Joint System II isokinetic dynamometer (Biodex Medical Systems Inc., Shirley, New York, NY, USA) with Biodex Advantage software, version 4.5. With the knee in 60° flexion, three maximum isometric contractions of the knee extensors and flexors were performed. The contraction time and relaxation time were both 5 s. Peak torque (Nm) was used in the analysis. The isokinetic concentric knee muscle strength was measured by 40 consecutive maximal reciprocal contractions at an angular velocity of 90° s−1. The range of motion of the knee joint was set at 0–100°. Peak torque and total work (Nm) were used in the analysis. The Biodex dynamometer has been shown to be valid and reliable [30, 32].
Kinesthesia test
Kinesthesia was measured in a specifically designed apparatus, which has been used and described in detail in previous studies, see for example [10, 11, 24, 25]. Measurements of the threshold for detection of passive motion (TDPM) were performed towards knee extension (TE) and knee flexion (TF) in a lateral decubitus position from the two starting positions, 20° and 40°, giving the variables TE20, TE40, TF20, and TF40. The median values of three consecutive measurements of these four variables were determined. The variables from the 20° starting position (TE20 and TF20) were used in the present study since these variables were found to be more reliable than those from the 40° starting position [1]. For the TE20 and TF20, ICC values were above 0.60. A difference in TDPM of at least 10% would be needed to be confident of detecting a real change between groups [1]. The sum of TE20 and TF20, giving an index value, was used for statistical analysis. Higher values indicate poorer proprioceptive acuity [25].
All tests were performed on both legs; the right leg being tested first.
Statistical analysis
Since men are stronger and hop a longer distance than women, and the sex distribution between the groups was uneven (64% men in the patient group and 50% men in the control group), men and women were analyzed separately with regard to the one-leg hop test and knee muscle strength. To avoid the subjectivity in choosing one of the legs, the average of the right and left legs in the control group, i.e., (right + left)/2 [21], was used for comparison with the subjects with ACL injury.
Studies have shown that knee OA is associated with defective motor and sensory function [9, 12]. However, there were too few subjects with OA (n = 5) to permit comparisons of values between those with and without OA. Visual analysis of plots showed that the values of the subjects with OA did not differ substantially from the values of those without OA.
The primary outcome was the one-leg hop test for distance. We have previously reported impaired functional performance in the injured and uninjured legs in patients compared with uninjured controls; the magnitude of the difference being 15% [4]. A sample size calculation estimated that at least 30 individuals (i.e., about 15 individuals per group) would be required to show a 15% difference between patients and controls in the one-leg hop test (SD 28 cm) with 80% power at the 5% significance level.
The independent t test, or the Mann–Whitney U test when appropriate, was used for the inter-group comparisons. A level of P ≤ 0.05 was chosen to indicate statistical significance.
Results
One-leg hop test for distance
No differences were found between the individuals with ACL injury and the controls in the men, or between the injured leg and the controls in the women (Table 2; Fig. 1). The women with ACL injury hopped a longer distance with their uninjured leg than the control group (P = 0.04; Table 2).
One-leg hop test (cm) in the injured and uninjured legs and in the control group in the men. The box includes the first to third quartiles with median values shown as a line through the box. The whiskers show values below 1.5 box lengths from the upper or lower edge of the box. The circle denotes an outlier (i.e., the value was between 1.5 and 3 box lengths from the upper edge of the box)
Knee muscle strength
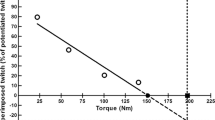
There were no differences between the individuals with ACL injury and the controls in peak torque isometric extension or flexion (Table 2; Fig. 2). Peak torque and total work in isokinetic extension were significantly higher in both legs among the men and the women with ACL injury than in the controls (Table 2; P < 0.006). Peak torque and total work in isokinetic flexion were significantly higher in the uninjured leg than in the controls among the women (P = 0.05 and 0.02, respectively), but not in the injured leg or in the men (Table 2).
Peak torque, isometric extension (Nm) in the injured and uninjured legs and in the control group in the men. The box includes the first to third quartiles with median values shown as a line through the box. The whiskers show values below 1.5 box lengths from the upper or lower edge of the box. The circles denotes outliers (i.e., the value was between 1.5 and 3 box lengths from the upper edge of the box)
Kinesthesia
The mean difference (95% CI) between the injured leg and the control group was 1.2° (0.2–2.3°; P = 0.03) and between the uninjured leg and control group 0.8° (0.1–1.5°; P = 0.02), with higher values in the patient group. When analyzing men and women separately, differences were observed between the injured leg and control group (mean difference 1.8, 95% CI 0.2–3.4; P = 0.03) and the uninjured leg and control group (mean difference 1.2, 95% CI 0.2–2.1; P = 0.01) among the men, but not in the women (injured leg vs. control: mean difference 0.4; 95% CI −0.5 to 1.3; P = 0.4, and uninjured leg vs. control: mean difference 0.5, 95% CI −0.6 to 1.5, P = 0.4; Fig. 3).
Kinesthesia, measured as the threshold for detection of passive motion (degrees), in the injured and uninjured legs and in the control group in the men. The box includes the first to third quartiles with median values shown as a line through the box. The whiskers show values below 1.5 box lengths from the upper or lower edge of the box. The circle denotes an outlier (i.e., the value was between 1.5 and 3 box lengths from the upper edge of the box), and the asterisks denote extreme values (i.e., cases with values more than 3 box lengths from the upper edge of the box)
In summary, there were no differences in the one-leg hop test or in knee muscle strength between the groups (in some variables the patients had better values than the controls), but the subjects with ACL injury had poorer kinesthesia than the uninjured controls. These results are illustrated in the men in Figs. 1–3.
Discussion
Our pre-defined hypothesis, that there were no differences between the patients with ACL injury and the controls in hop distance or knee muscle strength was confirmed. In some variables, the patients even had better values than the controls. However, the patients had poorer kinesthetic acuity than the uninjured controls. We have previously reported small differences between the injured and uninjured legs in the one-leg hop test and in knee muscle strength in this patient group, indicating good neuromuscular function [2]. The results in the present study showing no differences, or even better values, in the one-leg hop test and knee muscle strength in the patients compared to the controls, further support our postulation of good neuromuscular function at the long-term follow-up in these patients.
It has been reported that quadriceps weakness and poor functional performance are related to an increased risk of future joint problems after knee injury [26]. In our 15-year follow-up study, the patients had higher values of knee extensor strength than the uninjured controls. Possible explanations of this may be our treatment regime, including non-operative treatment, neuromuscular training, thorough information on the role of the muscles in knee joint stabilization, and advice regarding activities. It cannot be excluded that familiarity during the test could have been higher in the patients (e.g., they were familiar with the test from previous follow-ups, and they may have been highly motivated to perform their best) than in the controls (i.e., the controls were not followed prospectively). However, despite high familiarity, quadriceps activation failure may be present. Studies have shown quadriceps weakness in patients with ACL injury compared with uninjured controls [6, 33]. In these studies, superimposed electrical stimulation on maximal voluntary quadriceps activation, a sensitive method of detecting muscle strength deficiency, was quantified [6, 33]. However, other reasons for the observed findings in these studies may be that patients who were dissatisfied with their knee function (i.e., complaining of instability at the least in sports activity) were included [33], and that measurements were taken at a mean of 8 weeks (range 1–19 weeks) after the injury [6], while improvements in muscle strength have been observed up to 18 months or more after injury [15, 23, 35].
We found that the patients had significantly poorer kinesthesia in both legs than the controls. This has also been reported by others [13, 24]. The magnitude of the mean difference between the groups was over 30%, which is in line with a previous study where the same device was used [24]. When men and women were analyzed separately, the difference remained only among the men. This is possibly due to too small sample size, leading to effects on the statistical power. However, since no differences have been found between men and women in proprioceptive acuity [1, 11], they can be analyzed as one group. Several studies have shown a decrease in proprioceptive acuity after ACL injury, which has been reported in a review [9], although improvements have been observed during neuromuscular training in a prospective longitudinal study [10]. The present study had a cross-sectional design. Thus, it cannot be excluded that the patients had poor proprioceptive acuity in both legs before they suffered their injury. If so, this may be one reason for sustaining the injury.
Several studies have reported the effects of an ACL injury on motor function [22] or sensory function [9]. However, to our knowledge, our study is the first to compare measures of both sensory and motor function in a group of patients with ACL injury to uninjured controls. The results, showing the same or higher values for the one-leg hop test and knee muscle strength in the patients compared to the controls, indicate that motor function had normalized at long-term follow-up in these patients. The poorer kinesthesia noted in the patients compared to the controls, indicates that the sensory function is persistently disturbed. The patients in the present study had good subjective function and acceptable activity level [16], and good neuromuscular function [2]. Thus, they can be considered well-functioning. The results of our study indicate that proprioceptive deficiency may occur without the presence of knee muscle weakness or impaired functional performance. This has also been observed by others [7]. Thus, muscle function can compensate not only for the defective passive joint stability, but also for the proprioceptive deficiency. Possible explanations of this may be central somatosensory changes with altered muscle patterns [7], i.e., more efficient muscle activation. The impact of these findings on the risk of sustaining re-injuries requires further studies, and there may be a breakpoint at which the discrepancy between motor and sensory function becomes a risk factor during more strenuous activity.
Conclusions
The patients had the same, or better, functional performance and knee muscle strength but poorer kinesthesia than a control group of uninjured subjects. This indicates that although motor function can be restored after ACL injury, the sensory function is persistently disrupted.
References
Ageberg E, Flenhagen J, Ljung J (2007) Test-retest reliability of knee kinesthesia in healthy adults. BMC Musculoskelet Disord 8:57
Ageberg E, Pettersson A, Friden T (2007) 15-year follow-up of neuromuscular function in patients with unilateral nonreconstructed anterior cruciate ligament injury initially treated with rehabilitation and activity modification: a longitudinal prospective study. Am J Sports Med 35:2109–2117
Ageberg E, Zätterström R, Moritz U (1998) Stabilometry and one-leg hop test have high test-retest reliability. Scand J Med Sci Sports 8:198–202
Ageberg E, Zätterström R, Moritz U, Fridén T (2001) Influence of supervised and nonsupervised training on postural control after an acute anterior cruciate ligament rupture: a 3-year longitudinal prospective study. J Orthop Sports Phys Ther 31:632–644
Ashton-Miller JA, Wojtys EM, Huston LJ, Fry-Welch D (2001) Can proprioception really be improved by exercises? Knee Surg Sports Traumatol Arthrosc 9:128–136
Chmielewski TL, Stackhouse S, Axe MJ, Snyder-Mackler L (2004) A prospective analysis of incidence and severity of quadriceps inhibition in a consecutive sample of 100 patients with complete acute anterior cruciate ligament rupture. J Orthop Res 22:925–930
Courtney C, Rine RM, Kroll P (2005) Central somatosensory changes and altered muscle synergies in subjects with anterior cruciate ligament deficiency. Gait Posture 22:69–74
Fridén T, Erlandsson T, Zätterström R, Lindstrand A, Moritz U (1995) Compression or distraction of the anterior cruciate injured knee. Variations in injury pattern in contact sports and downhill skiing. Knee Surg Sports Traumatol Arthrosc 3:144–147
Fridén T, Roberts D, Ageberg E, Waldén M, Zätterström R (2001) Review of knee proprioception and the relation to extremity function after an anterior cruciate ligament rupture. J Orthop Sports Phys Ther 31:567–576
Fridén T, Roberts D, Zätterström R, Lindstrand A, Moritz U (1997) Proprioception after an acute knee ligament injury: a longitudinal study on 16 consecutive patients. J Orthop Res 15:637–644
Fridén T, Roberts D, Zätterström R, Lindstrand A, Moritz U (1996) Proprioception in the nearly extended knee. Measurements of position and movement in healthy individuals and in symptomatic anterior cruciate ligament injured patients. Knee Surg Sports Traumatol Arthrosc 4:217–224
Hurley MV (2003) Muscle dysfunction and effective rehabilitation of knee osteoarthritis: what we know and what we need to find out. Arthritis Rheum 49:444–452
Jerosch J, Prymka M (1996) Knee joint proprioception in normal volunteers and patients with anterior cruciate ligament tears, taking special account of the effect of a knee bandage. Arch Orthop Trauma Surg 115:162–166
Johansson H, Sjölander P, Sojka P (1991) Receptors in the knee joint ligaments and their role in the biomechanics of the joint. Crit Rev Biomed Eng 18:341–368
Konishi Y, Aihara Y, Sakai M, Ogawa G, Fukubayashi T (2006) Gamma loop dysfunction in the quadriceps femoris of patients who underwent anterior cruciate ligament reconstruction remains bilaterally. Scand J Med Sci Sports 17(4):393–399
Kostogiannis I, Ageberg E, Neuman P, Dahlberg L, Friden T, Roos H (2007) Activity level and subjective knee function 15 years after anterior cruciate ligament injury: a prospective, longitudinal study of nonreconstructed patients. Am J Sports Med 35:1135–1143
Kvist J (2004) Rehabilitation following anterior cruciate ligament injury: current recommendations for sports participation. Sports Med 34:269–280
Myklebust G, Holm I, Maehlum S, Engebretsen L, Bahr R (2003) Clinical, functional, and radiologic outcome in team handball players 6 to 11 years after anterior cruciate ligament injury: a follow-up study. Am J Sports Med 31:981–989
Paradowski PT, Bergman S, Sunden-Lundius A, Lohmander LS, Roos EM (2006) Knee complaints vary with age and gender in the adult population. Population-based reference data for the Knee injury and Osteoarthritis Outcome Score (KOOS). BMC Musculoskelet Disord 7:38
Paterno MV, Greenberger HB (1996) The test-retest reliability of a one legged hop for distance in young adults with and without ACL reconstruction. Isokinet Exerc Sci 6:1–6
Ranstam J (1998) Repeated measurement and analysis units. Review of basic principles. Acta Orthop Scand 69:345–346
Risberg M, Lewek M, Snyder-Mackler L (2004) A systematic review of evidence for anterior cruciate ligament rehabilitation: how much and what type? Phys Ther Sport 5:125–145
Risberg MA, Holm I, Tjomsland O, Ljunggren E, Ekeland A (1999) Prospective study of changes in impairments and disabilities after anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther 29:400–412
Roberts D, Friden T, Stomberg A, Lindstrand A, Moritz U (2000) Bilateral proprioceptive defects in patients with a unilateral anterior cruciate ligament reconstruction: a comparison between patients and healthy individuals. J Orthop Res 18:565–571
Roberts D, Fridén T, Zätterström R, Lindstrand A, Moritz U (1999) Proprioception in people with anterior cruciate ligament-deficient knees: comparison of symptomatic and asymptomatic patients. J Orthop Sports Phys Ther 29:587–594
Roos EM (2005) Joint injury causes knee osteoarthritis in young adults. Curr Opin Rheumatol 17:195–200
Roos EM, Roos HP, Ekdahl C, Lohmander LS (1998) Knee injury and Osteoarthritis Outcome Score (KOOS)—validation of a Swedish version. Scand J Med Sci Sports 8:439–448
Salmon LJ, Russell VJ, Refshauge K, Kader D, Connolly C, Linklater J, Pinczewski LA (2006) Long-term outcome of endoscopic anterior cruciate ligament reconstruction with patellar tendon autograft: minimum 13-year review. Am J Sports Med 34:721–732
Solomonow M, Krogsgaard M (2001) Sensorimotor control of knee stability. A review. Scand J Med Sci Sports 11:64–80
Taylor NA, Sanders RH, Howick EI, Stanley SN (1991) Static and dynamic assessment of the Biodex dynamometer. Eur J Appl Physiol Occup Physiol 62:180–188
Tegner Y, Lysholm J (1985) Rating systems in the evaluation of knee ligament injuries. Clin Orthop 198:43–49
Timm KE, Gennrich P, Burns R, Fyke D (1992) The mechanical and physiological performance reliability of selected isokinetic dynamometers. Isokinet Exerc Sci 2:182–188
Urbach D, Nebelung W, Weiler HT, Awiszus F (1999) Bilateral deficit of voluntary quadriceps muscle activation after unilateral ACL tear. Med Sci Sports Exerc 31:1691–1696
Valeriani M, Restuccia D, DiLazzaro V, Franceschi F, Fabbriciani C, Tonali P (1996) Central nervous system modifications in patients with lesion of the anterior cruciate ligament of the knee. Brain 119:1751–1762
Wojtys EM, Huston LJ (2000) Longitudinal effects of anterior cruciate ligament injury and patellar tendon autograft reconstruction on neuromuscular performance. Am J Sports Med 28:336–344
Zätterström R, Fridén T, Lindstrand A, Moritz U (2000) Rehabilitation following acute anterior cruciate ligament injuries—a 12 month follow-up of a randomized clinical trial. Scand J Med Sci Sports 10:156–163
Zätterström R, Fridén T, Lindstrand A, Moritz U (1998) Early rehabilitation of acute anterior cruciate ligament injury—a randomized clinical trial. Scand J Med Sci Sports 8:154–159
Zätterström R, Fridén T, Lindstrand A, Moritz U (1992) Muscle training in chronic anterior cruciate ligament insufficiency—a comparative study. Scand J Rehabil Med 24:91–97
Acknowledgments
We would like to thank all the subjects who volunteered for this study, Annika Pettersson, Malin Scharffenberg, Johan Flenhagen, and Henrik Nilsson for data collection, and Per-Erik Isberg for statistical advice. This study was supported by the Swedish National Centre for Research in Sports, and the Faculty of Medicine, Lund University.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ageberg, E., Fridén, T. Normalized motor function but impaired sensory function after unilateral non-reconstructed ACL injury: patients compared with uninjured controls. Knee Surg Sports Traumatol Arthr 16, 449–456 (2008). https://doi.org/10.1007/s00167-008-0499-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-008-0499-9