Abstract
Gait alterations after ACL reconstruction have been reported in the literature. The current study examined a group of 14 patients who all had an ACL reconstruction with a patellar tendon autograft. Kinetic and kinematic data were obtained from the knee during walking. The flexion-extension deficit (FED) calculated from the angular difference between maximal flexion and maximal extension during the stance phase in the ACL-reconstructed and the normal knee was measured. We investigated whether these alterations in gait are related to quadriceps strength and residual laxity of the knee. It may be that patients modify their gait patterns to protect the knee from excessive anterior translation of the tibia by reducing the amount of extension during stance. On the other hand, persistent quadriceps weakness may also cause changes in gait patterns as the quadriceps is functioning as an important dynamic stabilizer of the knee during stance. Results showed that patients had a significantly higher FED value (4.9±4.0) than a healthy control group in a previous study (1.3±0.9). This is caused mainly by an extension deficit during midstance. External extension moments of the knee (TZMAX were significantly lower in the current patients group than in a healthy control group (TZMAX −0.27±0.19 Nm/kg in patients vs. −0.08±0.06 Nm/kg in controls). There were no significant correlations between quadriceps strength and gait analysis parameters. Furthermore no correlation was found between the amount of laxity of the knee and gait. The relevance of this study lies in the fact that apparently the measured gait alterations cannot be explained solely by often used biomechanical indicators such as laxity and strength. The measured gait alterations may be a result of the surgical procedure with subsequent modified motor programming.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Anterior cruciate ligament (ACL) reconstruction has become a routine surgical procedure in the past 15 years. Since the early 1990s more aggressive rehabilitation programs have been advocated [30] including immediate full knee extension, weight bearing as tolerated, and early initiation of closed chain exercises emphasizing quadriceps strengthening. Subsequently coordinative exercises are implemented with the goal of return to sports 4–6 months after surgery. Several quantitative tests are described in the literature such as arthrometric knee laxity testing [3, 9, 30] and isokinetic strength testing [7, 11, 39] to evaluate the outcome of these surgical procedures. It has been demonstrated that laxity tests may not necessarily provide information about the functional status of the knee [33]. Furthermore, it is commonly accepted that return of a strong quadriceps muscle after knee injuries is vital for functional and athletic use of the lower extremity [4, 16, 23, 32] although others have not confirmed this correlation [1, 10]. Reports about isokinetic peak torque measurements taken approx. 6 months after ACL reconstruction and comparing the involved with the noninvolved side show quadriceps ratios ranging from 59.5% to more than 90% [7, 17, 31, 36, 37, 38]. Despite the differences reported the consensus seems that quadriceps strength does not return to normal levels by this time after surgery. This is interesting considering that most athletes are able to resume sports approximately 6 months after surgery.
We know from investigations performed at our gait laboratory [26] that a large percentage of patients show significant abnormalities during gait even 26 weeks after ACL reconstruction, equivalent to the time period when most patients return to sports. In fact our findings showed that the return of normal gait may even take more than 1 year. The most striking differences were an extension deficit and reduced external extension moments in the involved knee in the midstance phase of gait. The question arises as to the nature of different biomechanical strategies used, either consciously or unconsciously, by patients after ACL reconstruction. It may be that patients modify their gait patterns to protect the knee from excessive anterior translation of the tibia by reducing the amount of extension during stance. On the other hand, persistent quadriceps weakness may also cause changes in gait patterns as the quadriceps functions as an important dynamic stabilizer of the knee during stance.
The purpose of this study was to determine alterations in gait among patients whose ACL-deficient knees were surgically reconstructed with patellar tendon autograft, and if so, whether these are related to residual laxity and quadriceps strength. We chose to take the measurements 26 weeks after surgery as we know from a previous study that kinetic and kinematic characteristics of gait are still significantly different from controls [26].
Material and methods
Subjects
The study was carried out at the Otto Bock Research Department, Biomechanics Laboratory, Göttingen, Germany, and included 14 (7 men and 7 women) with a mean age of 24 years (range 21–40), mean height of 183 cm (range 162–192), and mean weight of 74.4 kg (range 56–101). All had a complete rupture of the ACL that was arthroscopically reconstructed using the central one-third of the patellar tendon. All patients participating in the study were collegiate or recreational athletes. After surgery they completed an intensive rehabilitation program as outpatients three times per week at the same rehabilitation center. The program included immediate weight bearing, range of motion exercises, pool therapy, stationary bicycle and closed chain strengthening, and coordination exercises. Running was permitted after 10 weeks, and once dynamic stability was satisfactory, agility and sports specific exercises were started. Return to sports involving pivoting and jumping was allowed after 6 months. Patients gave their consent to participate in this study and were free to withdraw from the study at any time. The study conformed the principles of the Declaration of Helsinki and German laws.
Clinical examination
All patients were examined by the same two physical therapists with, respectively, 10 and 8 years experience in orthopedics. The examination consisted of passive range of motion measurements of both knees for knee extension and flexion with a standard goniometer and instrumented laxity testing using the KT-1000 arthrometer (MEDmetric, San Diego, Calif., USA) applying a force of 89 N. Side-to-side differences are reported for comparison.
Isokinetic testing
Muscular performance of both knees was evaluated on an isokinetic testing device (Lido Active, Loredon Biomedical, Davis, Calif., USA) of both knees at a velocity of 60°/s. All patients had two or three training sessions on the isokinetic device in the weeks prior to testing to familiarize them with the testing procedure. The subjects performed a 15-min warm-up on a stationary bicycle (Kardiomed Bike, Proxomed, Karlstein, Germany) before the test procedure. Testing was carried out with the subjects in a seated position with the hip in 90° flexion and the thigh fixated with straps. The range of motion for the knee was set at 0° to 90° flexion. The noninvolved side was tested first. Prior to testing ten submaximal repetitions were performed. The test procedure consisted of ten maximal concentric repetitions for flexion and extension at a speed of 60°/s. The patients received standardized verbal commands, but visual information from the curves as displaced on the monitor was withheld. The peak torque of quadriceps and hamstring strength was compared with the noninvolved side and was expressed as a ratio (involved torque/noninvolved torque×100).
Gait analysis
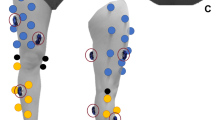
Gait analysis was performed for level walking at our gait laboratory using a four-camera optoelectric system (Primas, Delft Motion Analysis, Delft, The Netherlands) with a 100-Hz frequency for collection of the two-dimensional data. Reflective markers were placed on the subjects at anatomical landmarks according to the description in a previous paper [26]. The markers were placed at the greater trochanter, lateral femoral epicondyle, lateral malleolus, and on the outside of the shoe representing the location of the head of the fifth metatarsal. Thus only sagittal plane motions could be calculated. Two force plates (Kistler Instruments, Winterthur, Switzerland) embedded in a 12-m-long walkway measured the ground reaction forces of both legs with a sampling rate of 400 Hz. The two-dimensional data derived from the four cameras were synchronized with the collection of data from the force plates. All subjects were instructed to walk steadily during the test procedure. For each subject a specific starting point was determined from test trials so that the subject would contact the platform each time with the same limb without having to consciously focus to touch the plate. All subjects walked with sport shoes. The data used in this study were obtained from the mean values of 10–12 consistent cycles of walking over the walkway. Definitions of the quantitative parameters were described in detail in an earlier publication from our institution [26]. For the purpose of this study we summarize the most important kinetic and kinematic parameters.
To describe the kinematic changes during the stance phase, we calculated the angular difference between maximal flexion and maximal extension in the ACL-reconstructed and the normal knee. We defined this as the flexion-extension feficit (FED; Fig. 1). The determination of whether a significant FED value is due to reduced flexion or extension motion during stance can be made with the calculation of joint torques. In 90% of cases a higher value is associated with an extension deficit in stance [26]. The external, sagittal moment acting on the knee joint was calculated from kinematic data and ground reaction forces. During normal human gait there is an external flexion moment in the first 50% of stance which is followed by an external extension moment in the second half. The difference between the maximal values of the external flexion moments comparing the ACL-reconstructed knee with the normal knee is defined as TZMIN whereas the difference between maximal external extension moments is defined as TZMAX (Fig. 2). In this study we calculated only TZMAX as this has been shown to be a sensitive indicator of gait abnormalities [26]. All measurements were performed 26 weeks after surgery on all subjects.
Sagittal knee angles (θ) during the stance phase (t expressed as percentage of stance phase) for the reconstructed knee (left) and normal knee (right). D ACL Difference between maximal knee flexion an extension for the reconstructed knee; D NOR difference between maximal knee flexion an extension for the normal knee; FED DACL−DNOR
The sagittal knee moments during stance phase (t expressed as percentage of stance phase) normalized to body weight (M Z ). The external flexion (M ZMIN ) and extension (M ZMAX ) moments are shown for the ACL-reconstructed knee (left) and normal knee (right). The difference between the maximal values of the external flexion moments comparing the ACL-reconstructed knee with the normal knee is defined as T ZMIN and the difference between maximal external extension moments T ZMAX
Statistical analysis
Linear correlation coefficients were calculated with SPSS 10.0 for Windows to determine the relationship between isokinetic strength, laxity measurements, and gait analysis.
Results
Gait analysis
The mean value of FED in our patients during stance phase of gait was 4.9±4.0° and was significantly different from that of a control group in a previous study (P<0.01; Fig. 3). The mean external extension torque, TZMAX, was −0.27±0.19 Nm/kg, also significantly different from controls (P<0.05; Fig. 4).
Kinematic flexion extension deficit FED for the current patient group in comparison to the earlier recorded data of a comparable patient group (n=35, mean age 27 years) and a healthy control group (n=30, mean age 28 years) [27]. *P<0.01 vs. controls
External extension moments TZMAX for the current patient group in comparison to the earlier recorded data of comparable patient group (n=35, mean age 27 years) and a healthy control group (n=30, mean age 28 years) [27]. *P<0.01 vs. controls
Laxity examination and isokinetic strength
Laxity measurements with the KT-1000 with a 89-N force showed a mean side to side difference of 20.9 mm. The mean isokinetic quadriceps peak torque ratio at 60°/s for the involved side was 74.9±17.8% of the noninvolved side.
Correlation between laxity, isokinetic strength, and gait analysis
The linear correlation coefficients between clinical examination, isokinetic strength, and gait analysis are summarized in Table 1. There was a correlation between FED and TZMAX (P<0.05) but not between laxity examination, isokinetic quadriceps torque, and gait analysis parameters. We present four scatter diagrams showing the correlation between FED and isokinetic quadriceps peak torque (Fig. 5), that between TZMAX and laxity (Fig. 6), that between FED and laxity (Fig. 7), and that between TZMAX and isokinetic quadriceps strength (Fig. 8).
Discussion
The results of this study show that typical kinetic and kinematic deficits are present after ACL reconstruction. The abnormalities concern mainly range of motion, the extension motion of the knee, and the external extension moments acting on the knee joint during the stance phase of gait. In this context a there was statistically significant relationship between FED and TZMAX. In other words, we found that when FED reaches normal values, the most important kinetic parameter, expressed as TZMAX, also returns to normal values [26]. Neither FED nor TZMAX were related to quadriceps strength or laxity of the knee.
The concept of gait modification in ACL-deficient knees, termed quadriceps avoidance, as a strategy to reduce anterior displacement of the tibia is perhaps the most popularized [2, 6]. Others have not confirmed the phenomenon of quadriceps avoidance [5, 24, 26, 27, 34]. Cicotti et al. [8] reported consistent electromyographic activity of the vastus lateralis muscle during gait in patients with ACL-reconstructed knees compared to controls. Our results concerning the absence of a significant relationship between laxity and gait analysis are in general agreement with those of Rudolph and coworkers [25]. They examined subjects with ACL-deficient knees who were classified as copers and noncopers. Copers compensated well functionally for ACL injury compared to noncopers, who were not able to stabilize their knees and were scheduled for surgery. They found that the amount of laxity in their subjects was unrelated to gait patterns. The above conflicts in the literature may be due to differences in the method by which kinetic and kinematic data are calculated, examination of ACL-deficient or ACL-reconstructed knees, length of time after surgery, sample size, and statistical analysis used.
Our study showed that 6 months after ACL reconstruction patients had a mean isokinetic quadriceps peak torque ratio of 74.9%, which is near the values reported by others [17, 31, 36]. Our data show no statistical relationship between isokinetic quadriceps strength and gait analysis parameters. Some researchers have found positive relationships between isokinetic quadriceps peak torque and functional performance [4, 16, 23] while others have found only a low or no correlation [1, 10, 18, 29]. Several studies examining the effect of strength on gait analysis have been published. Snyder-Mackler and coworkers [32] studied 110 patients after ACL reconstruction and reported a relationship between isometric quadriceps strength and lower values of extension and flexion motion during the stance phase. In general the kinematic differences that they reported are in agreement with our findings; however, in contrast to their findings, the differences that we measured were unrelated to quadriceps strength. Lewek et al. [19] examined the relationship between isometric strength of the quadriceps on gait mechanics. They classified patients with ACL-reconstructed knees in two groups of strong quadriceps with strength ratios higher than 90% and those with ratios lower than 80%. They found a significant relationship between strength and knee angles and moments during the early phase of stance. Mittlmeier and colleagues [21] found that weakness of the quadriceps measured isokinetically 24 weeks after ACL reconstruction was related to gait abnormalities. However, they studied gait by assessing plantar pressure distribution which cannot calculate for joint moments as we did in our study. Rudolph et al. [25] did not find a correlation between isometric quadriceps strength and the amount of knee flexion during weight acceptance in subjects with ACL-deficient knees. It must be noted that kinetic testing usually involves maximal muscle activation whereas kinetic and kinematic parameters obtained during gait do not place maximal demands on the knee joint. This is a possible explanation for the lack of relationship between isokinetic quadriceps strength and gait analysis parameters.
Several investigators [5, 20, 24] have described the dynamic stabilizing function of the hamstrings in ACL-deficient knees. Less is known about the role of the hamstrings in a population with ACL-reconstructed knees. Cicotti et al. [8] reported near normal activity of the hamstrings during the swing phase of gait in ACL-reconstructed knees compared to controls. Work at our own institution [28] has shown that the activity of the gastrocnemius muscle is significantly reduced during the stance phase.
Although improvements in surgical techniques and more aggressive rehabilitation programs have been implemented, several authors continue to report persistent deficits in quadriceps strength [13, 22, 35]. Engelhardt and coworkers [11] showed that afferent signals from the central nervous system inhibit the activation of the quadriceps muscle after injury or surgery of the knee, causing the often observed atrophy of the quadriceps. Freiwald et al. [13, 14] demonstrated that isokinetic torque of the quadriceps is significantly lower 12 weeks after ACL reconstruction than preoperatively. The maximal isokinetic quadriceps ratio was 81% of that of the normal knee 16 months after surgery. Interestingly, the patients had a Lysholm score higher than 95 points and had all resumed their preoperative sports level. Recently Keays et al. [17] corroborated these findings. They showed that an isokinetic peak torque ratio of the quadriceps of 88% before surgery and decreasing to 72% 6 months after surgery despite intensive quadriceps training. Interestingly, functional tests improved by in the same time period. One may conclude that isokinetic quadriceps peak torque is not as important a predictor of function as initially thought. It may be that when a, so far undefined, “peak torque deficit” is crossed, subjective and objective limitations become noticeable. From the perspective of the theories in motor learning it appears that reprogramming of the central nervous system after ACL reconstruction allows improvement in functional tasks despite weakness of the quadriceps [15]. The clinical implication may be that focusing primarily on return of full quadriceps strength is no longer warranted, and that rehabilitation should rather implement goal-oriented exercises that replicate the functional demands as in sports or work [15].
Several limitations must be addressed in this study. First, we had a relatively small patient population. Second, the findings can be applied only to patients who undergo the same surgical procedures as those in our study population. Third, to our knowledge, the external validity of gait analysis has not been demonstrated to more athletic functional demands of the knee. The kinematic and kinetic data as measured in this study thus applies only to gait. Studying more strenuous activities such as running, jumping, and cutting movements may provide more relevant information about the differences in kinetic and kinematic parameters necessary for sports-related function of the knee. These could then be used as indicators of a safe return to sports after ACL reconstruction.
Our study clearly indicates that gait analysis parameters in ACL-reconstructed knees are not related to quadriceps strength and laxity. Central reprogramming of the central nervous system may be the reason [15] why gait is significantly altered after surgical reconstruction of the ACL [12] as these changes cannot be fully explained by quadriceps weakness and laxity of the knee.
References
Anderson MA, Gieck JH, Perrin D, Weltman A, Rutt R, Denegar C (1991) The relationships among isometric, isotonic and isokinetic concentric and eccentric quadriceps and hamstrings force and three components of athletic performance. J Orthop Sports Phys Ther 14:114–120
Andriacchi TP, Birac D (1993) Functional testing in the anterior cruciate ligament-deficient knee. Clin Orthop 288:40–47
Bach BR, Jones GT Hager CA (1995) Arthrometric results of arthroscopically assisted anterior cruciate ligament reconstruction using autograft patellar tendon substitution. Am J Sports Med 23:179–185
Barber SD, Noyes FR, Mangine RE, McCloskey JW, Hartman W (1990) Quantitative assessment of functional limitations in normal and anterior cruciate ligament deficient knees. Clin Orthop 255:204–214
Beard D, Soundarapandian R, O’Connor J, Dodd C (1996) Gait and electromyographic analysis of anterior cruciate ligament deficient subjects. Gait Posture 4:83–88
Berchuk M, Andriacchi TP, Bach BR, Reider B (1990) Gait adaptions by patients who have a deficient anterior cruciate ligament. J Bone Joint Surg Am 72:871–877
Carter TR, Edinger S (1999) Isokinetic evaluation of anterior cruciate ligament reconstruction: hamstring versus patellar tendon. Arthroscopy 15:169–172
Ciccotti M, Kerlan R, Perry J, Pink M (1994) An electromyographic analysis of the knee during functional activities. II. The anterior cruciate ligament-deficient and reconstructed profiles. Am J Sports Med 22:651–658
Daniel DM, Stone ML, Sachs R, Malcolm L (1985) Instrumented measurement of anterior knee laxity in patients with acute anterior cruciate ligament disruption. Am J Sports Med 13:401–407
Delitto A, Irrgang JJ, Harner CD, Fu FH (1993) Relationship of isokinetic peak torque and work to one legged hop and vertical jump in ACL reconstructed knees. Phys Ther 73:85
Engelhardt M, Reuter I, Freiwald J (2001) Alterations of the neuromuscular system after knee surgery. Eur J Sports Traum Rel Res 23:75–81
Ferber R, Osternig LR, Woollacott MH, Wasielewski NJ, Lee JH (2002) Gait mechanics in chronic ACL deficiency and subsequent repair. Clin Biomech 17:274–285
Freiwald J, Jager A, Starker M (1993) EMG-assisted functional analysis within the scope of follow-up of arthroscopically managed injuries of the anterior cruciate ligament. Sportverletz Sportschaden 7:122–128
Freiwald J, Reuter I, Engelhardt M (1999) Neuromuscular and motor system alterations after knee trauma and knee surgery. A new paradigm. In: Lehmann (ed) Overload, performance incompetence and regeneration in sport. Kluwer, New York, pp 81–100
Freiwald J, Engelhardt M (2002) Status of motor learning and coordination in orthopedic rehabilitation. Sportorthop Sporttraum 18:5–11
Karlsson J, Lundin O, Lossing IW, Peterson L (1991) Partial rupture of the patellar ligament. Results after operative treatment. Am J Sports Med 19:403–408
Keays SL, Bullock-Saxton J, Keays AC (2000) Strength and function before and after anterior cruciate ligament reconstruction. Clin Orthop 373:174–183
Kovaleski JE, Heitman RJ, Andres DPS, Gurchiek LR, Pearsall AW IV (2001) Relationship between closed-linear-kinetic and open-kinetic-chain isokinetic strength and lower functional performance. J Sport Rehabil 10:196–204
Lewek M, Rudolph K, Axe M, Snyder-Mackler L (2002) The effect of insufficient quadriceps strength on gait after anterior cruciate ligament reconstruction. Clin Biomech 17:56–63
Liu W, Maitland ME (2000) The effect of hamstring muscle compensation for anterior laxity in the ACL-deficient knee during gait. J Biomech 33:871–879
Mittlmeier T, Weiler A, Sohn T, Kleinhans L, Mollbach S, Duda G, Sudkamp NP (1999) Functional monitoring during rehabilitation following anterior cruciate ligament reconstruction. Clin Biomech 14:576–584
Natri A, Jarvinen M, Latvala K, Kannus P (1996) Isokinetic muscle performance after anterior cruciate ligament surgery. Long-term results and outcome predicting factors after primary surgery and late-phase reconstruction. Int J Sports Med 17:223–228
Noyes FR, Barber SD, Mangine RE (1991) Abnormal lower limb symmetry determined by function hop test after anterior cruciate ligament rupture. Am J Sports Med 19:513–518
Roberts CS, Rash GS, HonakerJT, WachowiakMP, Shaw JC (1999) A deficient anterior cruciate ligament does not lead to quadriceps avoidance gait. Gait Posture 10:189–199
Rudolph KS, Eastlack ME, Axe MJ, Snyder-Mackler L (1998) Movement patterns after anterior cruciate ligament injury: a comparison of patients who compensate well for the injury and those who require operative stabilization. J Electromyogr Kinesiol 8:349–362
Schmalz T, Blumentritt S, Wagner R, Gokeler A (1998) Gait analysis of patients within one year after anterior cruciate ligament reconstruction. Phys Med Rehabil Kurortmed 8:1–8
Schmalz T, Blumentritt S, Wagner R, Junge R (1998) Evaluation with biomechanical gait analysis of various treatment methods after rupture of the anterior cruciate ligament. Sportverletz Sportschaden 12:131–137
Schmalz T, Freiwald J, Greiwing A, Köcher L, Ludwig H, Blumentritt S (2001) Mechanical and electromyographical gait parameters in the course of rehabilitation afetr anterior cruciate ligament reconstruction. Eur J Sports Traum Rel Res 23:146–151
Sekiya I, Muneta T, Ogiuchi T, Yagishita K, Yamamoto H (1998) Significance of the single-legged hop test to the anterior cruciate ligament-reconstructed knee in relation to muscle strength and anterior laxity. Am J Sports Med 26:384–388
Shelbourne KD, Nitz P (1990) Accelerated rehabilitation after anterior cruciate ligament reconstruction. Am J Sports Med 18:292–299
Shelbourne KD, Foulk DA (1995) Timing of surgery in acute anterior cruciate ligament tears on the return of quadriceps muscle strength after reconstruction using an autogenous patellar tendon graft Am J Sports Med 23:686–689
Snyder-Mackler L, Delitto A, Baily SL, Stralka SW (1995) Strength of the quadriceps femoris muscle and functional recovery after reconstruction of the anterior cruciate ligament. J Bone Joint Surg Am 77:1166–1173
Snyder-Mackler L, Fitzgerald KG, Bartolozzi AR, Cicotti MG (1997) The relationship between passive joint laxity and functional outcome after anterior cruciate ligament injury. Am J Sports Med 25:191–195
Timoney JM, Inman WS, Quesda PM, Sharkey PF, Barrack RL, Skinner HB, Alexander AH (1993) Return of normal gait patterns after cruciate ligament reconstruction. Am J Sports Med 21:887–889
Yasuda K, Ohkoshi Y, Tanabe Y, Kaneda K (1992) Quantitative evaluation of knee instability and muscle strength after anterior cruciate ligament reconstruction using patellar and quadriceps tendon. Am J Sports Med 20:471–475
Wilk KE, Andrews JR (1992) Current concepts in the treatment of anterior cruciate ligament disruption. J Orthop Sports Phys Ther 15:279–293
Wilk KE, Keirns MA, Andrews JR, Clancy WG, Arrigo CA, Erber DJ (1991) Anterior cruciate ligament reconstruction rehabilitation: a six month follow-up of isokinetic testing in recreational athletes. Iso Exerc Sci 1:36–43
Wilk KE, Romaniello WT, Soscia SM, Arrigo CA, Andrews JR (1994) The relationship between subjective knee scores, isokinetic testing and functional testing in the ACL-reconstructed knee. J Orthop Sports Phys Ther 20:60–73
Witvrouw E, Bellemans J, Verdonk R, Cambier D, Coorevits P, Almqvist F (2001) Patellar tendon versus doubled semitendinosus and gracilis tendon for anterior cruciate ligament reconstruction. Int Orthop 25:308–11–20
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gokeler, A., Schmalz, T., Knopf, E. et al. The relationship between isokinetic quadriceps strength and laxity on gait analysis parameters in anterior cruciate ligament reconstructed knees. Knee Surg Sports Traumatol Arthrosc 11, 372–378 (2003). https://doi.org/10.1007/s00167-003-0432-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-003-0432-1