Abstract
A single latent variable model of health status and therapeutic health care utilization is estimated for parents and own children of 6,557 US households. The equation system that identifies latent health status simultaneously determines a number of indicators of general health, including presence of morbidity symptoms, mobility limitations, medication needs, and utilization of therapeutic health care services. The main goal of the paper was to obtain an unbiased estimate of parents’ marginal substitution rate between own and child health. Results indicate that parents’ valuation of their children’s health exceeds their valuation of own health by almost twofold on average.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Introduction
Children and their parents get illnesses. When an illness occurs, budget-constrained parents must choose between household consumption and the purchase of therapeutic health care. This paper employs a behavioral model of parent–child therapeutic health care use to assess a parent’s marginal rate of substitution between own and child health.Footnote 1 As children generally reside in households with parents who make primary decisions for them, an empirical test of a preference-based model of parental decision making linking a parent’s value of own health to her child’s health can provide scientifically and policy-relevant information about core issues of intrahousehold production and exchange. The refereed literature in economics contains a wealth of estimates for adult values of own health that are well-grounded in economic theory, but a paucity of such estimates for children.Footnote 2 Estimates of a parent’s value of own health relative to her value of child health are even scarcer.Footnote 3
In this paper, we use data on 6,557 US families from the 1999 US National Health Interview Survey to estimate a unified family, parent–child model with multiple indicators and multiple causes (MIMIC) of latent parent and latent child health. Latent health identifies a measure of parent-perceived own and child health status incorporating the multidimensional aspects of general health, including the physical, mental, and behavioral. The impact of a marginal change in latent health status upon parental choices to obtain and to use therapeutic family health care services identifies parents’ marginal rate of substitution between own health and child health. It thus represents a theoretically consistent and empirically feasible way of understanding parents’ valuation of the health of their children.
The MIMIC model developed herein may be preferred to the use of health status proxies (such as self-assessed health, time spent ill, or self-reported or clinical disease records) to estimate parents’ derived demands for own and for child health care services, as incomplete or inaccurate measures of underlying latent health status likely lead to bias in demand estimates and the health status values implied by these estimates (Leamer 1978; Wolfe and Behrman 1984; van der Gaag and Wolfe 1991). Section 2 outlines the analytical basis for use of the MIMIC model described in Section 3. Section 3 further outlines the conditions under which the model in Section 2 can be implemented empirically to estimate the parental marginal rate of substitution between own and child health. Section 4 concludes that on average, sample parents value their children’s health over their own health by almost twofold.
2 Family health and health care utilization
The household production literature emphasizes that along with relative prices and income, technical or biological processes condition input selections by family households in their production activities (Rosenzweig and Schultz 1983). When economic assessment of own health or health of family members is the focus, empirical applications of this literature (Becker 1993; Jacobson 2000) generally assume a parent or adult caregiver as the central decision maker who maximizes a joint utility function that is weakly separable intertemporally and is subject to budget and time constraints and a production technology for own and for child health:
where parental utility, U P, is a twice-differentiable, concave function of consumption goods, Z, that directly affect utility. A subset of Z (e.g., smoking or exercise) can also affect the “general health” of the parent, H P, and/or the child, H C. As in Grossman (1972) and Zelizer (1994), we interpret general health (hereafter referred to as health) as motivated by consumption, not investment. The production functions, H P(·) and H C(·), denote twice-differentiable and concave functions of health-related inputs, including specialized therapeutic inputs, M P and M C, which only affect utility indirectly by way of their impact on parent or child health. As is commonly assumed (Kenkel 1994), M P and M C denote scalar measures of health care services utilization (e.g., number of visits to a health care provider within a specified time period). Also, in expression 1, the household’s commodity set is “partitioned” according to three mutually exclusive and exhaustive bundles, Z, M P, and M C. Commodity bundling implies parental preferences are separable (or quasi-separable) in their respective partitions (Blackorby et al. 1978). The vectors, γ U and γ H, denote exogenous individual influences (such as education and age) on parental preferences and/or the production of family health.
Given smooth substitutability between parental work and other activities, the full-income budget constraint can be written as:
with \( r_{k} = q_{k} + wt_{k} ,k = Z,M, \), and \( Y = A + w{\left( {T - t_{s} } \right)} \). q k is the money price of commodity k, w is the opportunity cost of time, t k is the time required to consume one unit of commodity k, and t S is time spent away from the work place. Full income, Y, is the sum of non-labor income, A, and labor income, \( w{\left( {T - t_{\operatorname{S} } } \right)} \). Expression 2 requires total time available to be allocated among all possible uses of time, including non-health and health-related activities and the value of wage and non-wage income to equal total expenditures in the marketplace.Footnote 4 Households allocate their time between work and other consumption activities and allocate their income between health-related expenditures and expenditures on other goods to maximize utility. Parents choose Z, M P, and M C to maximize expression 1 subject to 2.
The first-order necessary conditions are:
plus the full-income constraint, \( Y - r_{Z} Z - r_{M} {\left( {M_{\operatorname{P} } + M_{\operatorname{C} } } \right)} = 0 \), where λ is the Lagrangian multiplier denoting the shadow price of Y. Expressions 3, 4, and 5 require the value of each good in marginal utility terms to equal its respective full price. Combining 4 and 5,
which states that at the optimum, parents equate the ratio of marginal health productivities of own versus child health care services to the parents’ utility substitution rate (i.e., the ratio of marginal benefits) between own and child health. Our goal was to assess parents’ relative value of own vs child health empirically by estimating the right-hand side of expression 6.
Solution of the above utility maximization problem yields parents’ demands for non-health and health-related commodities, along with their marginal utility of full-income, expressed in terms of all exogenous parameters in the model. Combining these exogenous parameters, γ U, γ H, q, w, and A, into the vector X, parents’ Marshallian demands and marginal utility of full-income are, respectively, Z* = Z(X), \( M^{ * }_{\operatorname{P} } = M_{\operatorname{P} } {\left( X \right)} \), \( M^{ * }_{\operatorname{C} } = M_{\operatorname{C} } {\left( X \right)} \) and λ* = λ(X). Substituting health-related demands into the health production functions yields parents’ optimum levels of own and child health:
and
Given the assumed curvature properties of production functions H P(·) and H C(·), 7a and 7b can be defined implicitly by their respective output distance functions, \( D^{\operatorname{o} }_{\operatorname{P} } \) and \( D^{o}_{C} \), which are homogenous in parent and child health,
and
8a and 8b give the maximum amount (distance) by which parents must either inflate or deflate health-related quantities, Z, M P, or M C, to reach their respective optimum general health contours defined by \( H^{*}_{P} \) and \( H^{*}_{C} \), conditional on individual values of X (Färe and Primont 1990). Clearly, parents’ utility-maximizing production contours are reached if and only if \( D^{o}_{P} {\left( \cdot \right)} = D^{o}_{C} {\left( \cdot \right)} = 1 \).
As commodity bundles are quasi-separable in Z, M P, and M C, expressions 8a and 8b expand to
and
where \( D^{o}_{P} = D^{o}_{C} = 1 \) if and only if the quasi-distance functions, \( D^{Z}_{\operatorname{P} } {\left( \cdot \right)} = D^{Z}_{\operatorname{C} } {\left( \cdot \right)} = D^{{M_{\operatorname{P} } }}_{\operatorname{P} } {\left( \cdot \right)} = D^{{M_{\operatorname{C} } }}_{\operatorname{C} } {\left( \cdot \right)} = 1 \) (Blundell and Robin 2000, p 60). Results in 9a and 9b provide a suitable basis for our empirical model in two ways; first, as the quasi-distance functions, \( D^{{M_{P} }}_{\operatorname{P} } {\left( \cdot \right)} = D^{{M_{C} }}_{\operatorname{C} } {\left( \cdot \right)} = 1 \) at the optimum, parents’ preferred quantities, \( M^{ * }_{P} \) and \( M^{ * }_{c} \), derive from \( D^{{M_{P} }}_{\operatorname{p} } {\left( \cdot \right)} \) and \( D^{{M_{\operatorname{C} } }}_{\operatorname{C} } {\left( \cdot \right)} \) via analytical inversion (see, e.g., McLaren et al. 2000; Wong and McLaren 2005). Formally,
and
Second, applying the implicit function rule to 10a and using \( D^{o}_{P} = {H^{ * }_{P} } \mathord{\left/ {\vphantom {{H^{ * }_{P} } {H_{\operatorname{P} } {\left( \cdot \right)}}}} \right. \kern-\nulldelimiterspace} {H_{\operatorname{P} } {\left( \cdot \right)}} \) from 8a,
Expression 11 depicts parents’ change in own health care services utilization resulting from an exogenous change in own health. When 11 is divided by \( {\partial M^{ * }_{C} } \mathord{\left/ {\vphantom {{\partial M^{ * }_{C} } {\partial H^{ * }_{C} }}} \right. \kern-\nulldelimiterspace} {\partial H^{ * }_{C} } \), the marginal substitution rate in expression 6 is obtained. An estimate of 6 can therefore be accomplished by estimating expressions 10a and 10b and evaluating the marginal impact of health on parents’ demand for own and for child health care services.Footnote 5
3 Empirical implementation
Treating “health” as a determinant of the demand for health care services is common in the health economics literature (Anderson 1968; Manning et al. 1982; Wedig 1988; Zweifel and Breyer 1997). As most medical care is therapeutic rather than preventive (major exceptions include well-baby care, immunizations, and care during pregnancy), people seek care when they perceive a health problem. Thus, in any empirical analysis of health care demand, the consumptive aspect of health plays a critical role; it must be accounted for in empirical models to minimize potential biases and incorrect interpretations of other policy relevant factors in the model, such as differences in income, insurance, and access to and quality of care. But general health is unobserved and plausibly multidimensional. Standard practice is to add one or more (treated as separable) proxy variables to control for variation of multidimensional health in demand equations for health care utilization. The choice of these proxy variables is almost always guided by data availability (e.g., Gerking and Stanley 1986), but this choice can impact the estimation results because technical interdependencies and non-allocable inputs go unrecognized. Thus, when analyzing the demand for health care, it is desirable, whenever possible, to employ multiple health indicators jointly. No one of the available health measures is by itself a sufficient proxy for health (van der Gaag and Wolfe 1991, p 55).
We estimate expressions 10a and 10b using an empirical model closely paralleling that of Wolfe and Behrman (1984). By “explaining” errors in the use of single indicators as measures of health, their model is able to use a variety of health proxies simultaneously as “indicators” of imperfectly revealed signals of the latent general health measure, H*. Our indicators include both health proxy measures and therapeutic utilization of health care for parents and children who reside together. As causal factors in a latent health production function, we include predetermined sociodemographic variables that are plausibly correlated with one or more of the included health indicators. Thus, H* defines a single latent variable in a MIMIC model.
Using our Section 2 notation, the model consists of three linear equations:
where 12 is a latent health status function, 13 is a health care utilization function, and 14 is a measurement function showing how latent health status is expressed through each observable but imperfect indicator. The vector M* represents m observed dimensions of parental health care utilization (m = 2 for parent and child utilization); the vector I represents n observed indicators of parent and child health (below we use n = 5 observed health indicators). The matrix X consists of k observed exogenous or predetermined family, resource, and demographic characteristics. Given that parents and children are nested within a family, model variables i = H*, X, M*, and I are stacked and estimated jointly according to
The B, a, c, and d are sets of unknown parameters. Error terms, δ, ɛ, and ϕ, are assumed to be mutually independent and normally distributed with zero mean and finite variance and do not differ systematically between parent and child. Any correlation across indicators for a household member is driven by the common factor, H* (Jöreskog and Goldberger 1975, p 632). We assume a linear-log form for our health care utilization 13 and measurement 14 functions to account for possible nonlinearities. This form also accommodates the fact that our data observes M* and I as zero bounded (or dichotomous), while satisfying the requirement that the output distance functions 8a and 8b be linear homogeneous in H*.Footnote 6
Specification and identification
To estimate 12, 13, and 14, we use data from the adult and child core samples of the 1999 US National Health Interview Survey (NHIS). From each family in the NHIS, one sample adult and one sample child (if one or more postnatal children age 17 or younger reside at home) were randomly selected, and information on each sample member was collected using the adult- and child-sample core questionnaires. Because some health issues differ between adults and children, the two questionnaires diverge on some items regarding specific health symptoms, but both collect the same basic information on health indicators, utilization of health care services, and health-related behaviors. For children, information is provided by a knowledgeable adult family member over the age of 18 who resides in the household. When combined, the two core samples provide a nationally representative sample of 6,557 parents (or caregivers) and children who reside together.Footnote 7
Table 1 presents definitions, means, and standard deviations of the covariates used to estimate the structural equations for parent own and child health status and health care utilization. We treat the 12-month period to which the data refer as short-term, implying that latent health status affects health care utilization, but health care utilization will not have had time to affect the long-term stock of health. Utilization, M*, is defined by total number of parent or child visits within the last 12 months to either: (1) a physician or medical professional at an office or health care clinic (or received a visit at home) or (2) a hospital emergency room or urgent care facility. Ninety percent of the subject children and 84% of their respondent parents had at least one such visit. As in Wolfe and Behrman (1984), M* is specified as a function of four categories of observed characteristics of the family and its members: (1) geographical variables related to regional differences in general prices and physician availability (e.g., whether the family resides in a metropolitan or rural area); (2) household resources including income, type of insurance coverage, and family size; (3) taste variables related to parental perceptions of physician quality and convenience; and (4) latent individual health status. Latent health, H*, is specified as a function of individual and family characteristics that relate to productive (Grossman and Kaestner 1997) and allocative (Kenkel 1990) efficiency in the production of health and knowledge of health alternatives, including parental educational attainments and family income, whether two parents reside in the household, individual biological age, number of siblings, race, and geographic location. Finally, as in expression 3, observed health status indicators, I, are a function of unobserved latent health status and stochastic terms that reflect other unobserved factors. The NHIS data supply five indicators of general health status: (1) whether the parent or child has a health impairment that limits mobility in any way; (2) whether a health condition (including mental illness or emotional or cognitive difficulty) currently requires a prescription medication to be taken for at least 3 months; (3) the number of short-term illnesses experienced within the last 30 days; (4) the number of other (including chronic) illnesses experienced (or ongoing) in the past 12 months; and (5) whether the parent believes that current own (or child) health status is worse in comparison to the previous year.Footnote 8 Errors in respondent reports of these indicators are presumed independent of observed family and member characteristics.
Empirical implementation of the MIMIC model incorporates restrictions of the type familiar to econometricians and additional restrictions familiar to psychometricians. We first discuss econometric issues regarding model identification. Identification in latent variable models is not as straightforward as just counting overall parameter exclusion restrictions (Wolfe and Behrman 1984, p 699; Bollen 1989, p 331). Substituting expression 12 into 13 and 14 gives the reduced forms:
and
which can be combined and written as
where
and
The covariance matrix for the disturbances in this reduced-form model is
where \( \Theta = \operatorname{var} {\left( u \right)} \), and \( \sigma ^{2}_{\delta } = \operatorname{var} {\left( \delta \right)} \). First, as the units of latent H* are arbitrary, identification of the a and d parameters in 17 requires normalization of a single element of the d vector. The choice of this normalization is arbitrary, as the remaining elements of d identify as constants of proportionality from the remaining columns of Π 12 (Van de Ven and Hooijmans 1991). Here, we use the normalization that the association between family short-term illnesses experienced and lnH* is one. As remaining elements of d are proportional to the normalized parameter chosen, the estimated impact of H* on parents’ utilization of own and/or child health care remains invariant to this choice. Nevertheless, in regressions not reported, we investigated the influence of alternative normalizations. We found no inconsistencies among our results.
Second, having solved for a, two additional elements (one in B and one in c) remain unidentified from the m × k elements in Π 12, requiring at least two exclusion restrictions on Π 12. We impose zero restrictions on two coefficients, age and sex, in the parent and child health care utilization equations (columns 3 and 4 of Tables 2, 3). McCool et al. (1995) provide evidence that the widely observed greater use of medical care by females than by males is due “...at all ages” to female biology rather than to male–female preference differences or to differences in the prices females face. As for age, the Grossman (1972) model of adult health production makes the deterioration of adult health with age its analytical linchpin. In contrast, children’s immune systems mature with age, implying improved health. Older children may also have an enhanced ability to cope with health shocks. We, thus, posit that subject age and gender influence the subject’s use of medical care only through their effects upon the subject’s latent health. Below, we explore further the empirical implications of this restriction. On grounds that they have no direct health effect, we also impose zero restrictions upon the taste (medical care quality and convenience) and price (insurance) variables for the general health expressions. These latter exclusions (i.e., of taste and price variables) are necessary to maintain consistency with the general health expressions as structural equations. Following Kenkel (1990) and Grossman and Kaestner (1997), income and education variables enter these structural equations as important determinants of whether and how people utilize health information and hence the positioning and the shape of their optimum health production contours. We thus have seven zero restrictions imposed upon the covariates in our system, giving us overidentification. Finally, given five indicator equations for each individual medical care use equation, our number (56) of variance–covariance parameters exactly equal the number of independent elements in our variance–covariance matrix; therefore, the covariances are identified (Wolfe and Behrman 1984, p 699).
A psychometric estimation issue arises given our assumption of a unified family structure. As parents (as primary decision makers) make choices involving intrahousehold allocation, the MIMIC model must be estimated jointly for adults and children. This then requires that equality constraints be imposed on the corresponding d coefficients across the adult and child subsamples. In the psychometric literature, this “invariance of factor loadings” is a minimum requirement for the comparability of latent means across multiple groups (Muthén and Christoffersson 1981; Marsh and Garyson 1994) or time periods (Finkel 1995).Footnote 9
Tables 2 and 3 present maximum likelihood estimates of the MIMIC model for parent and child health and therapeutic health care utilization based on the method of Chen (1981), whose unbiasedness requires that unobservables such as genetic health endowments and observed covariates be statistically independent. The first two columns of Table 2 present estimates of parent and child health (the parameter vector a in expression 12); columns three and four present estimates of parents’ utilization of own and child health care services. The five columns of Table 3 show estimates of parent and child general health indicators (the parameter vector d in expression 14).
In addition to the parameter estimates and estimates of their asymptotic t statistics, a series of goodness-of-fit measures is reported. The goodness-of-fit measures are defined as (see, e.g., Robins and West 1977):
and
where: V X = the sample variance–covariance matrix of lnX; \( R^{2}_{X} \) = the proportion of the variance of lnH* accounted for by lnX; \( R^{2}_{{I_{j} }} \) = the proportion of the variance of indicator I j accounted for by lnH*; and \( R^{2}_{{X,M,I}} \) = a measure of the overall explanatory power of the observables—this may be viewed as the R 2 from a theoretical regression of lnH* on lnX, M*, and I.
Results at the bottom of Tables 2 and 3 indicate highly significant negative associations between parent and child general health (lnH*) and all indicators of ill health. The \( R^{2}_{{I_{j} }} \)’s reveal that differences in lnH* account for more of the observed variance in self-assessed parent/child health (Worse) and number of health conditions (Other) experienced than of the observed variance in mobility limitations (IHMOB) and prescription drug use (PROBRX).
Results in column 1 at the top of Table 2 indicate that among sample parents, lower age and higher income are associated with higher latent health status. White parents are not significantly healthier than black parents (in terms of the magnitude of the estimated coefficients), and parents who live in metropolitan areas emerge as healthier than parents who reside in non-metropolitan areas. Parents with larger families emerge as healthier. Signs of the estimated coefficients for child health (in column 2 of Table 2) generally parallel the parent estimates in column one. A notable exception is child age, which is positively associated with better health.Footnote 10 Also, no added health benefit emerges for children who reside in metropolitan areas or for male children. Having both parents present in the household and more household income contributes positively to a child’s health.Footnote 11 The coefficient \( R^{2}_{{X,M,I}} \) implies that roughly 53% of the variation in unobserved parent and child health status is explained by all model observables including causes and indicators, and \( R^{2}_{X} = 0.336 \) indicates that observables in lnX account for almost two thirds of this 53%.
In the health care utilization equations (columns 3 and 4 of Table 2), the signs of the 15 coefficients conform to what one would expect a priori from Grossman’s (1972) consumption model. Parents’ choices to utilize own and/or child therapeutic health care services are very significantly associated with latent health status. As in Anderson (1968), van der Gaag and Wolfe (1991), and others, the negative signs of these coefficients indicate that as parent and child health increases, parents’ use of health care services declines in tandem with the negative relationship between general health and observed indicators of medical need, given families’ resources and their perceptions of medical care quality and accessibility/convenience. Also, as in Wolfe and Behrman (1984, p 701), the strong significance of the general health status coefficients “...indicates that the failure to control adequately for health status in estimating health care determinants in single-equation estimates may result in biased estimates of the impact of observed variables.” While controlling for latent health status, some of the direct determinants of health care utilization emerging as statistically significant include insurance coverage and family income (including CHIP families for children’s utilization), and parents’ self-assessments of physician quality and health care accessibility. In addition to the resource/quality variables, health care utilization appears to be significantly greater in the Northeast region for adults and for children and for adults in metropolitan areas. These associations probably reflect primarily the geographical pattern of the availability of health care facilities. Family size has a significant negative impact on child health care utilization and a negative but insignificant impact on adult utilization. Also, adult education and the presence of both parents have positive impacts on utilization for children. As in Kenkel (1990), these impacts probably reflect the idea that better informed consumers with cooperating spouses are more likely to seek out therapeutic medical care.
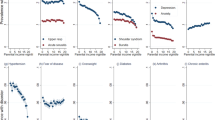
Table 4 reports overall sample and various subsample estimates of parents’ marginal substitution rates between child and own health. Substitution rate estimates are calculated as the ratio of derivatives of Table 2 columns 3 and 4 with respect to child and adult (log) latent health. Row 1 of Table 4 gives the overall sample mean substitution rate of 1.83 with a standard deviation of 1.73. As mentioned earlier, the unit scale of lnH* hinges on the indicator chosen for normalization, but does not influence the substitution rate—a relative measure independent of the units of H*. Our sample mean estimate of 1.83 is comparable to the relative values (means of roughly 2.0) that Liu et al. (2000) and Dickie and Messman (2004) estimate parents apply to reductions in their children’s vs their own acute illness symptoms (both these studies use a survey methodology), and the 1.5 relative value that Agee and Crocker (2007) estimate smoking mothers apply to protection of their children’s health from second-hand tobacco smoke exposure reduction vs protection of their own health from reducing smoking (this last study uses a revealed-preference methodology).
The lower panels in Table 4 present parental substitution rates estimated for selected subsamples identified in the literature as important determinants of parental resource allocation decisions within families. Substitution rates range from 0.9 to 5.16; parental rates tend to be lower for subsamples of families with only one parent present (average of 1.33) and for parents with lower income levels (average of 1.47 for families with income below the 1999 US poverty level). Some fairly significant differences also appear when families have greater child numbers; consistent with Becker’s (1993) increasing marginal utility of child numbers, sample families with five or more children reveal an average substitution rate in excess of two. The most dramatic change in parental substitution rate appears as children advance in age. The average rate among parents with infant children (less than 1 year) exceeds 5.0 and falls toward 1.0 or less as children approach adulthood. Dickie and Messman (2004) observe a similar pattern.
Sensitivity analysis
Although we interpret parents’ demand for medical services as driven largely by a curative or therapeutic motive, medical care demand is also driven by a preventive motive, consistent with Grossman’s (1972) concept of investment in health. For example, in the USA, an increase in health care utilization due to routine/preventive reasons is generally observed among women during pregnancy and childbearing, among children from birth to approximately age 2, and among adults over age 40. In contrast, routine/preventive visits among young adult males are relatively infrequent.
Our data exclude utilization due to only one the aforementioned reasons: mothers’ prenatal visits not counting visits due to medical problems associated with pregnancy. Examination of full sample correlation coefficients between visit type (e.g., office visits, surgeries, emergency room visits) and age or gender of sample children or parents provides some insight as to the extent of the “routine nature” of care in our data. For example, full sample correlations between parent or child age or gender and the number of emergency room visits, home visits, or surgeries are all quite low, ranging from 0.001 to 0.03 in absolute value. And sample correlation coefficients between office visits (a care type plausibly encompassing more of the “preventive” motive) and parent age, gender, or child gender, while slightly higher, are also quite low, ranging from 0.009 to 0.08 in absolute value.
There are, however, a couple of notable exceptions to these coefficients hinting at the presence of routine/preventive care in the data. First, we find a notably higher full sample correlation between child age and child office visits (−0.21); second, although the full sample correlation between parent gender and parent office visits appears low, the correlation between the subsample of adult males under age 30 and their office visits is notably higher (−0.3). Closer inspection of our data indicates that children of ages two and younger have a significantly higher average number of office visits than children of ages three and older, and adult males under age 30 have significantly lower numbers of office visits than sample males over age 30.
To investigate whether these higher correlations may be confounding any of the subsample differences found in our marginal substitution rate estimates, we compared our full sample MIMIC model estimates to estimates obtained using a subsample of families with subject children of ages three or older (N = 5,107). The N = 5,107 subsample serves two purposes: It eliminates families with potentially high rates of child health care motivated solely by routine/preventive reasons, and because parent and child age are so highly (positively) correlated, it eliminates the majority of younger sample males who have uncommonly low rates of care.
Compared to the full sample estimates, the N = 5,107 estimates reveal statistically significant changes in three coefficients of Table 2: The log of child health status on child health care use increases by 0.57, the log of child age on child health status decreases by 0.3, and parent Sex on parent health status decreases by 0.2. All three coefficients remain statistically significant without changes in sign. Also, there is a moderate decrease in and a loss in the significance of the coefficient for parent Age on parent health status. These coefficient changes imply that inclusion of families with children of ages two and younger (comprised largely of younger parents) into our full sample estimates leads to a decrease in the marginal impact of child health status on child health care use, plus an increase in the adult health benefit of being younger and an adult male. The first of these inclusion effects will bias downward our full sample marginal substitution rate estimate; the second effect leads to an upward bias. However, although we find the N = 5,107 subsample mean substitution rate of 2.11 to be higher than our full sample mean of 1.83 (presented in Table 4), this difference is not statistically significant.Footnote 12
Finally, to investigate further the possible confounding influence of preventive care on our results, we also estimated separate MIMIC models using “only surgeries” and “only emergency room (ER) visits” as the dependent variables for health care use (noting that these care types are intuitively more “curative” and correlate the least with parent or child age or gender). While the estimates using only ER visits exhibit a much higher variance (due largely to the fact that low income and uninsured families account for more ER visits), the mean substitution rate using only ER visits amounts to roughly 1.65. The mean rate using only surgeries has a much lower variance and is roughly 1.55. Both of these means do not differ significantly from the “all care types” mean of 1.83 in Table 4.
These “only ER” and “only surgeries” results also suggest that taking explicit account of differences in the efficacies of treating the various illnesses embedded within each of our health status indicators would not cause a statistically significant change in our estimated mean substitution rate. ER visits and especially surgery imply that sample subjects have chosen and have subsequently acted upon a particular course of treatment. Moreover, given that the poor and the uninsured make disproportionate use of ER medical care (Nadel 1992), our right-hand-side income and insurance covariates likely capture much of the difference between the efficacy of ER and other expressions of medical care consumption.
4 Conclusions
This paper develops and implements a model of latent health and health care utilization to achieve a consistent estimate of the impact of general health upon parents’ utilization of own and child therapeutic health care services. This health status impact is then used to estimate parents’ marginal rate of substitution between their own and their child’s health. The equation system identifying latent health status simultaneously determines several indicators of general health including presence of morbidity symptoms, mobility limitations, and medication needs, as well as the utilization of health care services. Estimates shaped by this system recognize that no single health indicator or proxy serves as an adequate measure of general health and that single indicators of general health engender errors of measurement. The estimates from a representative sample of 6,557 US households imply that parents value their children’s health over their own health by almost twofold.
Several caveats are worthy of mention. First, when parental preferences are involved, caring parents are likely to go to great lengths to ensure the health, safety, and welfare of their children; hence, the marginal utility of children’s health may well be greater than that of own health in parents’ utility functions. The substitution rates estimated herein are derived in the context of a utility maximization model and reflect parents’ preference-based values from their observed choices, conditional on family characteristics and resources. Use of this framework precludes identification of specific components of the parent/child health valuation disparity. For example, part of this disparity other than pure altruism may reflect parents’ risk averse desire to reduce “excess uncertainty” in evaluating own versus child’s health and their consequent assessment of the need for health care services.Footnote 13 Second, because three of the health status indicators used to estimate expressions 1 through 3 are dichotomous, the system estimated does not strictly satisfy the normality assumption. Although the dichotomous nature of these variables appears to have little effect on their point estimates, which compare reasonably to single-equation estimates using a limited dependent variable method (i.e., probit inclusive of a constant term),Footnote 14 the results in Tables 2 and 3 nevertheless could be sensitive to the form of the underlying distribution. Third, as in all econometric investigations, the results are conditional upon specification and available data. While the NHIS data provide a seemingly adequate collection of indicators for individuals’ general health status, lack of additional health proxy data precludes a more detailed analysis of optimal indicator choice. As in Leamer (1978) and in Atkinson and Crocker (1987), this choice, for any given data set and behavioral model, seems an empirical question revolving around the trade-off between specification uncertainty (the inclusion of yet more indicators) and the increased likelihood of correlated measurement errors in the included indicators.Footnote 15
Notes
The use of preventive care to evaluate a parental tradeoff between own and child health is problematic. There often is no trade-off because good parental health can have a positive impact on child health. Consider for example the well-known Barker (1998) thesis regarding maternal health during pregnancy, infant health, and the infant’s health as an adult. Also, parental health may affect a parent’s ability to use and choice of preventive care (Archer et al. 2006). A healthy parent is in a better position to nurture, monitor, and teach her child.
Viscusi et al. (1988) on household chemicals, Carlin and Sandy (1991) on seat belt use, Agee and Crocker (1996a,b) on body burdens of lead, Liu et al. (2000) on short-term morbidity symptoms, Jenkins et al. (2001) on bicycle helmets, Agee et al. (2004) on child abuse, and Dickie (2005) on acute illnesses appear to exhaust the list for children.
Liu et al. (2000), Dickie and Messman (2004), and Agee and Crocker (2007) exhaust this list. In the absence of a scientific consensus on this relative value, US federal agencies have been using unadjusted adult health values to make their mandated assessments of the value of policy interventions upon the health and safety of children. See for example the benefit transfer procedures outlined in Kuchler and Golan (1999), US Environmental Protection Agency (2000), and in Dockins et al. (2001). Agee and Crocker (2004) discuss in detail the analytical and empirical issues associated with these procedures.
r M in expression 2 assumes a single time cost for adult and child medical treatments and physician’s visits valued at the parent’s opportunity cost of time. We also assume a single market price vector for similar medical treatments/procedures, physician’s visits, drugs, insurance, and co-pays across individual household members. Given nearly 80% (17) of our sample households have private (Medicaid) coverage, we believe this assumption is plausible, as it is consistent with other empirical studies (e.g., Wolfe and van der Gaag 1981) which presume that individuals who reside together likely confront similar prices for similar medical goods/services via similar coverage.
Note that our distance function formulation uses information derived from both the multiple input health production functions and the parents’ utility function. It can be contrasted with formulations in Gerking and Stanley (1986) and elsewhere wherein the demand for health is the product of the marginal cost (derived from the underlying health production function with a single input, e.g., medical care) of a health impact and an exogenous change in the source (e.g., pollution) of the impact.
Monte Carlo results by Adamowicz et al. (1989) actually find the stability properties of linear-log forms of zero-bounded demand relations to exceed those of the more widely used linear and semilog forms.
This sample is net of any missing observations. The gross sample consists of roughly 9,000 households.
This information excludes normal health care use related to pregnancy and childbearing. Use due to problems experienced with pregnancy is included.
While invariance of factor loadings is necessary to arrive at a meaningful parental marginal substitution rate estimate, reduced forms 15 and 16 show that “group non-invariance” of parameters in a and B is necessary for observed covariates in X to capture individual and group differences among observed health status indicators, I, referred to as “formative” or “cause” indicators on latent H*, as well as for parental differences in their observed choices of own and child health care utilization, \( M^{ * }_{P} \) and \( M^{ * }_{C} \), referred to as “reflective” or “effect” indicators due to latent H* (Bollen and Lennox 1991).
The significance of family income in the child health regression contrasts with some earlier studies that find little to no association between income and health when child health is measured using only one from a variety of proxy measures (see, e.g., Edwards and Grossman 1980).
Model estimates using only the N = 1,450 subsample of families with children of ages two and younger indicate no added decrease in the marginal impact of child health status on child health care use. However, these estimates indicate a substantial increase in the adult health benefit of being male. Thus, the N = 1,450 subsample, which yields a mean substitution rate of 5.1, appears to be strongly influenced by a “parental youth” effect, i.e., younger parents with younger children have a higher estimated latent health status (particularly subsample males) and, given our Eq. 13, a higher coefficient estimate for \( H^{ * }_{P} \) results in a higher substitution rate.
Some rudimentary observations are of course possible. For instance, if parents’ pure altruism is presumed not to decline as their children age, the higher substitution rates observed in Table 4 for younger children might reflect parents’ “excess uncertainty,” in view of the fact that younger children do not communicate health indicators to parents as effectively as older children.
Probit estimates are available from the authors.
Indeed, high multicollinearity among indicators in a MIMIC model reduces stability of indicator coefficient estimates (Diamantopoulos and Winklhofer 2001). As the absolute value of the coefficient estimates of the indicators are interpreted as indicator validity coefficients (Bollen 1989), high multicollinearity renders assessment of indicator validity problematic. From a theoretical perspective, the list of indicators should be sufficiently inclusive to capture fully the construct’s (latent variable) domain of content (Nunnally and Bernstein 1994, p 484). Similar to other surveys used to assess health status in general populations (e.g., the oft-used SF-12 survey; Ware et al. 1998), the NHIS indicators span the domain of self-assessed health, physical functioning, mental health, and presence of acute and/or chronic illnesses. The statistical significance of all our Table 3 indicator coefficients (including coefficients of STI when alternative normalizations are specified) suggests our construct is comprised of valid indicators.
References
Adamowicz WL, Fletcher JJ, Graham-Tomasi T (1989) Functional form and the statistical properties of welfare measures. Am J Agric Econ 71(2):414–421
Agee MD, Crocker TD (1996a) Parental altruism and child lead exposure: inferences from the demand for chelation therapy. J Hum Resour 31(3):677–691
Agee MD, Crocker TD (1996b) Parents’ discount rate for child quality. South Econ J 63:36–50
Agee MD, Crocker TD (2004) Transferring measures of adult health benefits to children: a review of issues and results. Contemp Econ Policy 22(4):468–482
Agee MD, Crocker TD (2007) Parents’ valuation of children’s health benefits from environmental tobacco smoke control: evidence from mothers who smoke. Empir Econ 32(1):217–237
Agee MD, Crocker TD, Shogren JF (2004) An economic assessment of parents’ self-composure: the case of physical child abuse. Topics Econ Anal Policy 4(1):1161 (Article 9)
Anderson R (1968) A behavioral model of families’ use of health services. Center for health administration studies research series 25. University of Chicago Graduate School of Business, Chicago, IL
Archer DW, Crocker TD, Shogren JF (2006) Choosing children’s environmental risk. Environ Resour Econ 33(3):347–369
Atkinson SE, Crocker TD (1987) A Bayesian approach to assessing the robustness of hedonic property price studies. J Appl Econ 2(1):27–45
Barker DJP (1998) Mothers babies and diseases in later life. Churchill Livingston, London, UK
Becker GS (1993) A treatise on the family. Harvard University Press, Cambridge, MA
Blackorby C, Primont D, Russell R (1978) Duality separability and functional structure: theory and economic applications. North-Holland, Amsterdam
Blundell R, Robin J (2000) Latent separability: grouping goods without weak separability. Econometrica 68(1):53–84
Bollen KA (1989) Structural equations with latent variables. Wiley, New York, NY
Bollen KA, Lennox R (1991) Conventional wisdom on measurement: a structural equation perspective. Psychol Bull 110(2):305–314
Burdine JN, Felix MRJ, Abel AL (2000) The SF-12 as a population health measure: an exploratory examination of potential for application. Health Serv Res 35:885–905
Carlin PS, Sandy R (1991) Estimating the implicit value of a young child’s life. South Econ J 58:186–202
Chen C-F (1981) The EM approach to the multiple indicators and multiple causes model via the estimation of the latent variable. J Am Stat Assoc 76(375):704–708
Diamantopoulos A, Winklhofer H (2001) Index construction with formative indicators: an alternative to scale development. J Mark Res 38(2):269–277
Dickie M (2005) Parental behaviors and the value of children’s health: a health production approach. South Econ J 71:855–872
Dickie M, Messman VL (2004) Parental altruism and the value of avoiding acute illness: are kids worth more than parents? J Environ Econ Manage 48(3):1146–1174
Dockins C, Jenkins R, Owens N, Simon N, Wiggins L (2001) Valuation of childhood risk reductions: the importance of age risk preferences and perspective. US Environmental Protection Agency, Washington, DC
Edwards L, Grossman M (1980) Children’s health and the family. In: Scheffler R (ed) Annual series of research in health economics, vol 2. JAI, Greenwhich, CT
Färe R, Primont D (1990) A distance function approach to multioutput technologies. South Econ J 56:879–891
Finkel SE (1995) Causal analysis with panel data. Sage, London UK
Fleishman JA, Lawrence WF (2003) Demographic variation in SF-12 scores: true differences or differential item functioning? Med Care 41(7):S75–S86
Gerking S, Stanley L (1986) An economic analysis of air pollution and health: the case of St Louis. Rev Econ Stat 68(1):115–121
Gold RB, Sonfield A (2001) Expanding eligibility and improving outreach under CHIP. The Guttmacher report on public policy. Guttmacher Institute, http://www.guttmacher.org/pubs/tgr/04/3/gr040306.html
Grossman M (1972) On the concept of health capital and the demand for health. J Polit Econ 80(2):223–255
Grossman M, Kaestner R (1997) Effects of education on health. In: Behrman JR, Stacey N (eds) The social benefits of education. University of Michigan Press, Ann Arbor, MI, pp 69–123
Jacobson L (2000) The family as producer of health-an extended Grossman model. J Health Econ 19(5):611–637
Jenkins RR, Owens N, Wiggins LB (2001) Valuing reduced risks to children: the case of bicycle safety helmets. Contemp Econ Policy 19(4):397–408
Jöreskog KG, Goldberger AS (1975) Estimation of a model with multiple indicators and multiple causes of a single latent variable. J Am Stat Assoc 70(351):631–639
Kenkel D (1990) Consumer health information and the demand for medical care. Rev Econ Stat 72(4):587–595
Kenkel D (1994) Cost of illness approach. In: Tolley G, Kenkel D, Fabian R (eds) Valuing health for policy: an economic approach. University of Chicago Press, Chicago, IL, pp 42–71
Kuchler F, Golan E (1999) Assigning values to life: comparing methods for valuing health. Agriculture Economics Report No 784. Food and Rural Economics Division, Economic Research Service, US Department of Agriculture, Washington, DC
Leamer EE (1978) Specification searches: ad hoc inference with nonexperimental data. Wiley, New York, NY
Liu J-T, Hammitt JK, Wang J-D, Liu J-L (2000) Mother’s willingness-to-pay for own and her child’s health: a contingent valuation study in Taiwan. Health Econ 9(4):319–326
Manning WG, Newhouse JP, Ware JE (1982) The status of health in demand estimation. In: Fuchs VR (ed) Economic aspects of health. University of Chicago Press, Chicago, IL
Marsh HW, Garyson D (1994) Longitudinal stability of latent means and individual differences: a unified approach. Struct Equ Modeling 1(2):317–359
McCool J, Kiker BF, Ng YC (1995) Gender and the demand for medical care. Appl Econ 27(6):483–495
McLaren KR, Rossiter P, Powell A (2000) Using the cost function to generate flexible Marshallian demand systems. Empir Econ 25(2):209–227
Muthén B, Christoffersson A (1981) Simultaneous factor analysis of dichotomous variables in several groups. Psychometrika 46:407–419
Nadel V (1992) Emergency departments: unevenly affected by growth and change in patient use. US General Accounting Office, Human Resources Division Publication 93-4, Washington, DC
Nunnally JC, Bernstein IH (1994) Psychometric theory, 3rd. McGraw-Hill, New York, NY
Robins PK, West RW (1977) Measurement errors in the estimation of home value. J Am Stat Assoc 72(358):290–294
Rosenzweig M, Schultz TP (1983) Estimating a household production function: heterogeneity the demand for health inputs and their effects on birth weight. J Polit Econ 91(5):723–746
US Environmental Protection Agency (2000) Guidelines for preparing economic analyses. US Environmental Protection Agency, EPA 240-R-00-003, Washington, DC
Van de Ven W, Hooijmans E (1991) The MIMIC health status index. In: Duru G, Paelinck JHP (eds) Econometrics of health care. Kluwer, London, UK, pp 19–29
van der Gaag J, Wolfe B (1991) Estimating demand for medical care: health as a critical factor for adults and children. In: Duru G, Paelinck JHP (eds) Econometrics of health care. Kluwer, London, UK, pp 31–58
Viscusi WK, Magat WA, Forrest A (1988) Altruistic and private valuations of risk reduction. J Policy Anal Manage 7(2):227–245
Ware JE, Kosinski M, Keller SD (1998) SF-12 physical and mental health summary scales, 3rd edn. Quality Metric, Lincoln, RI
Wedig G (1988) Health status and the demand for health: results on price elasticities. J Health Econ 7(2):151–163
Wolfe BL, Behrman JR (1984) Determinants of women’s health status and health-care utilization in a developing country: a latent variable approach. Rev Econ Stat 66(4):696–703
Wolfe BL, van der Gaag J (1981) A new health status index for children. In: van der Gaag J, Perlman M (eds) Health economics and health economics. North Holland, Amsterdam, pp 283–304
Wong GKK, McLaren KR (2005) Specification and estimation of regular inverse demand systems: a distance function approach. Am J Agric Econ 87(4):823–834
Zelizer VA (1994) Pricing the priceless child: the changing social value of children. Princeton University Press, Princeton, NJ
Zweifel P, Breyer F (1997) Health economics. Oxford University Press, New York, NY
Acknowledgment
Insights and comments from two anonymous referees, Scott Atkinson, Karen Conway, and workshop participants at the University of Georgia are gratefully acknowledged. The US Environmental Protection Agency financially supported the research efforts through grant #R82871601. However, the research has not been subjected to the Agency’s required peer and policy review and therefore does not necessarily reflect the views of the Agency.
Author information
Authors and Affiliations
Corresponding author
Additional information
Responsible editor: Deborah Cobb-Clark
Rights and permissions
About this article
Cite this article
Agee, M.D., Crocker, T.D. Does parents’ valuation of children’s health mimic their valuation of own health?. J Popul Econ 21, 231–249 (2008). https://doi.org/10.1007/s00148-007-0159-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00148-007-0159-2