Abstract
Purpose
To describe bleeding and thrombotic events and their risk factors in patients receiving extracorporeal membrane oxygenation (ECMO) for severe coronavirus disease 2019 (COVID-19) and to evaluate their impact on in-hospital mortality.
Methods
The ECMOSARS registry included COVID-19 patients supported by ECMO in France. We analyzed all patients included up to March 31, 2022 without missing data regarding bleeding and thrombotic events. The association of bleeding and thrombotic events with in-hospital mortality and pre-ECMO variables was assessed using multivariable logistic regression models.
Results
Among 620 patients supported by ECMO, 29% had only bleeding events, 16% only thrombotic events and 20% both bleeding and thrombosis. Cannulation site (18% of patients), ear nose and throat (12%), pulmonary bleeding (9%) and intracranial hemorrhage (8%) were the most frequent bleeding types. Device-related thrombosis and pulmonary embolism/thrombosis accounted for most of thrombotic events. In-hospital mortality was 55.7%. Bleeding events were associated with in-hospital mortality (adjusted odds ratio (adjOR) = 2.91[1.94–4.4]) but not thrombotic events (adjOR = 1.02[0.68–1.53]). Intracranial hemorrhage was strongly associated with in-hospital mortality (adjOR = 13.5[4.4–41.5]). Ventilation duration before ECMO ≥ 7 days and length of ECMO support were associated with bleeding. Thrombosis-associated factors were fibrinogen ≥ 6 g/L and length of ECMO support.
Conclusions
In a nationwide cohort of COVID-19 patients supported by ECMO, bleeding incidence was high and associated with mortality. Intracranial hemorrhage incidence was higher than reported for non-COVID patients and carried the highest risk of death. Thrombotic events were less frequent and not associated with mortality. Length of ECMO support was associated with a higher risk of both bleeding and thrombosis, supporting the development of strategies to minimize ECMO duration.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
In patients affected by coronavirus disease 2019 (COVID-19) supported by extracorporeal membrane oxygenation (ECMO), bleeding incidence was high and associated with mortality, with intracranial hemorrhage carrying the highest risk of death. Thrombotic events were less frequent and not associated with mortality. Length of ECMO support was associated with a higher risk of both bleeding and thrombosis. |
Introduction
Veno-venous (VV) and veno-arterial (VA) extracorporeal membrane oxygenation (ECMO) are increasingly used in the management of refractory respiratory and circulatory failure [1,2,3,4]. However, ECMO complication rates remain high. Bleeding and thrombosis on ECMO are particularly frequent and carry a high risk of both morbidity and mortality [5,6,7,8,9,10,11,12,13]. They occur as a result of a complex interplay between the underlying critical illness, blood exposure to shear stress and non-biological surfaces and antithrombotic strategies.
Since the beginning of the SARS-CoV-2 pandemic, ECMO has been widely used for acute respiratory distress syndrome (ARDS) related to coronavirus disease 2019 (COVID-19) and, to a lesser extent, for COVID-19-associated circulatory failure [14,15,16,17,18]. Immunothrombosis is thought to be a key mechanism contributing to the pathogenesis of severe COVID-19 and to its high reported thrombotic risk [19,20,21]. This putative relationship has led to an ongoing research effort to evaluate optimal antithrombotic strategies and, frequently, to an intensification of anticoagulant dosing for COVID-19 patients in the intensive care unit (ICU) [22,23,24,25,26]. Although the rates and mechanisms of bleeding and thrombosis in COVID-19 patients have been extensively studied, relatively little is known about bleeding and thrombosis risks of COVID-19 patients on ECMO. The existing data are limited to small single-center series and one multicenter study [27,28,29,30,31,32,33,34,35,36,37].
Therefore, the goals of this prospective multicenter cohort study were: (1) to report bleeding and thrombotic events in patients receiving ECMO for severe COVID-19; (2) to evaluate their impact on in-hospital mortality; and (3) to identity factors associated with their occurrence. We hypothesized that bleeding and thrombotic events would be frequent and associated with worse outcomes.
Materials and methods
Data collection
The French national ECMOSARS registry (ClinicalTrials.gov Identifier: NCT04397588) was launched in April 2020 and is still currently recruiting COVID-19 patients supported by ECMO (VV or VA). The registry has been approved by the Rennes University Hospital ethics committee (n° 20.43). According to the French legislation, written consent was waived because of the observational design of the study. The data collection methodology has previously been described in the first report of the registry [17]. Briefly, data were collected by research assistants using an electronic case report form, and consistency tests were performed by data managers. Collected data included patient characteristics and comorbidities, management of COVID-related ARDS before ECMO cannulation, patient characteristics at ECMO cannulation and the day after, therapeutics, complications and patient outcomes on ECMO (see Supplementary Table S1 for the definition of the main variables). Patient and ECMO management, including anticoagulation, screening for bleeding/thrombosis complications and weaning protocol, was at the discretion of each center.
Study design and population
For the present study, we analyzed all consecutive patients included in the registry from the first patient included on February 25, 2020 up to March 31, 2022 without missing data regarding bleeding and thrombotic events. The analysis followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines (Supplementary Table S2).
Outcomes and variables
Our primary outcome was the incidence of thrombotic and bleeding events. Secondary outcomes were in-hospital mortality, mortality at day 28, mortality at day 90, ICU length of stay and hospitalization duration.
The ECMOSARS registry captures all clinically relevant bleeding and thrombotic events, irrespective of their assumed severity (see Supplementary Table S1 for the definition of bleeding and thrombotic events). No systematic screening was performed for both bleeding and thrombosis complications. Bleeding events included: intracranial bleeding, upper or lower gastrointestinal hemorrhage, peripheral cannulation site bleeding, retroperitoneal bleeding and pulmonary hemorrhage. Thrombotic events included: ischemic stroke, deep vein thrombosis, pulmonary embolism (or pulmonary thrombosis), acute mesenteric ischemia, acute limb ischemia, macroscopic thrombus of circuit and/or membrane without needing to change the circuit or the oxygenator, oxygenator failure requiring change due to clot formation, acute circuit thrombosis requiring change. In addition, the following variables were included in the present study: pre-ECMO patient-related variables (baseline demographics and comorbidities), pre-ECMO hospitalization related variables (center, Simplified Acute Physiology Score (SAPS) II, non-invasive ventilation, high-flow oxygen therapy, neuromuscular blocking agents, prone position, antiviral therapy, antibiotic therapy), variables at ECMO cannulation (ventilation duration, Sequential Organ Failure Assessment (SOFA) score, ARDS, vasoactive and inotropic drugs, lactatemia, pH, PaO2/FiO2 ratio, PaCO2 change within 24 h after ECMO initiation, renal replacement therapy, anticoagulation, platelet count, prothrombin time (PT) expressed as percentage of standard value, fibrinogen), cannulation-related variables (retrieval and transport, type of ECMO), on-ECMO variables (antiplatelet agent, anticoagulation-related variables, antithrombin monitoring, length of ECMO support, transfusion requirements, vasoactive and inotropic drugs, acute kidney injury, infectious complications).
Statistical analysis
Patient characteristics are expressed as number (percentage) for categorical variables and median with interquartile range for continuous variables. For comparison between bleeding and thrombotic complications, a χ2 test or a Fisher’s exact test were used for categorical variables and a Kruskal–Wallis test for continuous variables. For comparison between VV and VA-ECMO and between epidemic waves, a χ2 test or a Fisher’s exact test were used.
A statistical analysis plan was made prior to accessing the data. No a priori statistical power calculation was conducted. Only pre-ECMO variables and variables at ECMO cannulation were included in the following multivariable analyses to prevent competing risk bias.
A directed acyclic graph was used to describe our model of causal associations between bleeding and thrombotic events (exposure variables), patient-related confounders, pre-ECMO hospitalization-related confounders, at ECMO cannulation confounders and in-hospital mortality, using DAGitty software (Supplementary Figure S1) [38]. No variables were analyzed as effect modifiers. The set of potential confounders sufficient for adjustment was: age, body mass index (BMI), center, PT at cannulation, type of ECMO (VV or VA), renal replacement therapy before ECMO, ventilation duration before ECMO and PaO2/FiO2 at cannulation. A multivariable logistic regression model was then used to estimate odd ratios between bleeding and thrombotic events (exposure variables) and in-hospital mortality. Confounders entered in the model were defined a priori using the directed acyclic graph. Centers were included in analysis as stratification factor. Patients who were still hospitalized at the time of database lock were not included in this analysis. Mortality at day 90 was also evaluated for any bleeding, any thrombosis and intracranial hemorrhage using the same model, as a post-hoc secondary analysis.
Multivariable logistic regression models were also used to identify variables independently associated with bleeding and thrombotic events. Variables entered in the models were defined a priori, based on published ECMO and COVID-19 literature [9, 10, 21, 27, 36, 37, 39,40,41,42,43,44,45,46]. No further variable selection was done. The set of variables entered in the model for bleeding events was: age, body mass index, type of ECMO, ventilation duration before ECMO, anticoagulation before ECMO, PT at cannulation, platelet count < 100 G/L at cannulation, fibrinogen < 1.5 g/L at cannulation, pH ≥ 7.25 at cannulation, PaO2/FiO2 ratio at cannulation, renal replacement therapy at cannulation, PaCO2 change within 24 h after ECMO initiation and length of ECMO support. The set of variables entered in the model for thrombotic events was: age, body mass index, type of ECMO, ventilation duration before ECMO, anticoagulation before ECMO, PT at cannulation, platelet count ≥ 350 G/L at cannulation, fibrinogen ≥ 6 g/L at cannulation, pH ≥ 7.25 at cannulation, PaO2/FiO2 ratio at cannulation, renal replacement therapy at cannulation, PaCO2 change within 24 h after ECMO initiation, length of ECMO support and history of venous thromboembolism. A sensitivity analysis was performed by removing from the multivariable models, the variables imputed with more than 30% of missing data (PT and fibrinogen).
Linearity of continuous independent variables and log-odds was checked. If not, those variables were transformed into categorical variables in accordance with previously published works [3, 9, 10, 17, 46].
Multiple imputation was used to account for missing values in variables. We used fully specified chained equations in the SAS MI procedure. For continuous variables, the regression method was used to impute missing values and discriminant function methods were used for binary and categorical variables. Passive imputation was used for the derived variables (BMI), meaning that each variable needed for the calculation was imputed prior to the calculation of the derived variable. Fifty imputed data sets were created and combined using standard between/within-variance techniques.
To describe the clinical management and outcomes over the course of the pandemic, a post-hoc analysis was performed by splitting the cohort between the first epidemic wave (up to July 1, 2020 [47]), and the next waves (from July 1, 2020 to March 31, 2022). Indeed, substantive changes were made regarding ICU management of COVID-19 patients in France after the first wave, including improved healthcare organization at a national scale, widespread use of Dexamethasone [48], increased use of non-invasive ventilation [49] and SARS-CoV-2 vaccination (starting January 2021).
All tests used two-tailed hypothesis. Statistical significance was achieved for p < 0.05. Statistical analyses were performed with SAS version 9.4 software (SAS Institute, Cary, North Carolina, USA).
Results
Study population
Among the 701 patients included in the ECMOSARS registry at the time of database lock, 81 had missing data regarding bleeding and thrombotic events, leaving 620 patients included in the present study (Fig. 1). Five hundred sixty-eight patients were supported by VV-ECMO, and 52 by VA-ECMO. Median age was 55 (47–61) years, 22.9% were females, and had a median body mass index of 30 (27–34) kg/m2 (Table 1). Median SAPS II was 42 (31–57). ICU management before ECMO cannulation included non-invasive ventilation (32.5%), high-flow oxygen therapy (51.6%), neuromuscular blocking agents (94.8%), prone positioning (90.4%), antiviral therapy (49.2%) and antibiotics (90.1%). At the time of ECMO cannulation, 96% met Berlin criteria for ARDS with a median PaO2/FiO2 ratio of 68 (57–85) mmHg, and 11.9% were on renal replacement therapy.
Coagulation management
At ECMO cannulation, 90.1% (430/477) of patients had received anticoagulation (therapeutic-dose 45.3%, prophylactic-dose 44.9%). Median fibrinogen level was 7.4 (5.6–8.7) g/L, median PT was 73 (64–82)% and median platelet count was 255 (184–345) G/L (Table 2).
During ECMO support, the majority of patients received systemic anticoagulation (95.3%) and the preferred anticoagulant was unfractionated heparin (98.1%; n = 468). Unfractionated heparin was monitored using anti-factor Xa activity (91.6%), activated partial thromboplastin time (7.4%) and activated clotting time (ACT) (0.9%; n = 431). Median time to achieve anticoagulation target defined by centers for each patient was 9 (4–44) h. The anti-factor Xa activity target was ≥ 0.3 IU/mL in 86.2% of patients (n = 354; Supplementary Tables S3 and S4). Antithrombin (AT) levels were monitored for 27.3% of patients (n = 476), for whom the lowest AT level was 62 (50–73) %. Forty patients (8.5%) received AT supplementation (n = 471). Anticoagulation management was not significantly modified over the course of the pandemic (Supplementary Table S4).
Incidence of bleeding and thrombosis
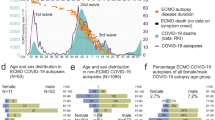
Overall, 406 (65.5%) patients suffered from bleeding or thrombosis during ECMO support (306 with bleeding and 225 with thrombosis), of whom 181 (29%) had only bleeding events, 100 (16%) only thrombotic events and 125 (20%) both bleeding and thrombotic events (Table 3; Fig. 1). Of 725 total events, 382 (53%) were bleeding events (Fig. 2A). Cannulation site (114 events, 18.4% of patients) and ear nose and throat (76 events, 12.3% of patients) were the most frequent bleeding types. Intracranial hemorrhage accounted for 6.8% of total events (49 events, 8% of patients). Ten percent of bleeding events (40 events) were associated with a massive transfusion (> 10U PRBCS/24 h). Device-related thrombosis accounted for most thrombotic events with 82 circuit changes due to acute thrombosis (13.2% of patients), 59 oxygenator failures (9.5% of patients) and 72 macroscopic thrombi of circuit or membrane without needing to change circuit or oxygenator (11.6% of patients). Pulmonary embolism/thrombosis was diagnosed in 9.4% of patients (58 events). No significant difference was observed between VV and VA-ECMO regarding overall incidence of bleeding and thrombosis (Supplementary Tables S5, S10 and S11). VA-ECMO support, however, was associated with a significant increase in gastrointestinal bleedings (15.4% vs 6.5%, p = 0.043), leg ischemia (13.5% vs 1.1%, p < 0.001) and ischemic stroke (9.6% vs 0.9%, p < 0.001). While thrombosis incidence remained stable over the course of the pandemic (32.7% vs 37.6%, p = 0.267, Supplementary Table S6), overall bleeding increased after the first epidemic wave (58.2% vs 46.2%, p = 0.008, Supplementary Table S6).
Incidence and impact of bleeding and thrombotic events during ECMO support for severe COVID-19. A. Distribution of bleeding and thrombotic events on ECMO, expressed as percentage of total events (n = 725). Bleeding events are represented in red, thrombotic events in blue. B. Independent association of main bleeding and thrombotic events with in-hospital mortality. GI, gastrointestinal; ENT, ear nose and throat; AdjOR, adjusted odds ratio; CI, confidence interval
Outcomes and bleeding/thrombosis events
In-hospital mortality was 55.7% (336/603) with a median follow-up of 51 (34–78) days for survivors and 17 (8–28) days for deceased patients. Mortality at day 90 was 62.6% (330/527). Bleeding events were associated with higher in-hospital mortality with 71.8% for bleeding only, 69.4% for bleeding and thrombosis, 42.4% for thrombosis only and 40.3% for no bleeding or thrombosis (p < 0.001; Table 4). On multivariable analysis, overall bleeding was independently associated with in-hospital mortality (adjusted odds ratio (adjOR) = 2.91 [1.94–4.4]; Fig. 2B, Supplementary Table S7), unlike overall thrombosis which was not associated with increased in-hospital mortality (adjOR = 1.02 [0.68–1.53]; Fig. 2B, Supplementary Table S8). Likewise, mortality at day 90 was increased in patients with bleeding complications (adjOR = 3.21[2.03–5.1]; Supplementary Table S7). Among bleeding types, intracranial hemorrhage was independently associated with in-hospital mortality (adjOR = 13.5 [4.4–41.5]; Fig. 2B, Supplementary Table S9) and mortality at day 90 (adjOR = 23.9 [4.6–124.8]; Supplementary Table S9). Pulmonary bleedings were also independently associated higher in-hospital mortality (adjOR = 2.67 [1.27–5.6]; Fig. 2B). Successive bleeding events in a patient were associated with higher mortality rates with adjusted odd-ratios of 1.87 [1.19–2.96] for one event, 3.84 [2.05–7.2] for two events and 3.63 [1.80–7.3] for three or more events. On univariate analysis, bleedings complications were associated with transfusion requirements on ECMO (packed red blood cells, fresh frozen plasmas and platelet concentrates) and acute kidney injury (Table 4).
Factors associated with the occurrence of bleeding and thrombotic events
Factors independently associated with the occurrence of all bleeding events were ventilation duration before ECMO ≥ 7 days (adjOR = 1.62 [1.09–2.41]) and length of ECMO support (per 5 days increase, adjOR = 1.08 [1.01–1.15]; Supplementary Table S10). Factors independently associated with the occurrence of all thrombosis events were fibrinogen ≥ 6 g/L at cannulation (adjOR = 1.94 [1.00–3.75]) and length of ECMO support (per 5 days increase, adjOR = 1.17 [1.09–1.26]; Supplementary Table S11). Sensitivity analyses removing PT and fibrinogen, imputed with more than 30% of missing data, from the variable selection did not change these results (Supplementary Tables S10 and S11).
Discussion
Our study reports bleeding and thrombotic events at a nationwide level in a large multicenter cohort of COVID-19 patients supported by ECMO. The main findings were as follows. First, bleeding complications were common, occurring in 49% of patients, and were independently associated with in-hospital mortality and mortality at day 90. Second, thrombotic events, while also common (36%), were associated with a fibrinogen ≥ 6 g/L at cannulation but not with mortality. Third, duration of ECMO support was associated with a higher risk of both bleeding and thrombosis. Fourth, intracranial hemorrhage was frequent (8%) and associated with high mortality rates (in-hospital and at day 90). And finally, the vast majority of the patients (95.3%) received a systemic anticoagulation with unfractionated heparin as the drug of choice (98.1%), mainly monitored by anti-factor Xa activity.
The incidence of bleeding complications in our study was high, with almost half of patients experiencing at least one bleeding event, which was higher than previously published studies on both COVID-19 and non-COVID patients supported by ECMO. This might, however, be explained by the fact that the ECMOSARS registry captures all bleeding events, irrespective of their assumed severity (unlike Extracorporeal Life Support Organization (ELSO) registry or International Society on Thrombosis and Haemostasis (ISTH) major bleeding criteria) [3, 11,12,13, 16, 27, 28]. Overall, bleeding was independently associated with in-hospital mortality with a cumulative effect of bleeding recurrence, as already reported [11,12,13, 27]. In addition, our study demonstrates a sustained impact of bleeding on mortality at day 90. Finally, bleeding incidence seemed to increase over the course of the pandemic, which might be compared with the increased mortality previously reported [14, 47, 50, 51]. However, these findings will need to be confirmed in larger and more extensive studies.
Intracranial hemorrhage (ICH) incidence was higher than previously reported for both VV and VA-ECMO in non-COVID patients [3, 9, 11,12,13]. This seems, however, in line with recent data suggesting a higher incidence of ICH for COVID-19 patients supported by VV-ECMO [12,13,14, 16, 29,30,31, 34]. Notably, non-severe COVID-19 seems to be associated with a small but significant increase in the incidence of ICH [52, 53]. Unfortunately, many of these studies suffer from bias and heterogeneity in the diagnosis and reporting of intracranial hemorrhage, limiting their interpretation. The cause of the comparatively higher ICH incidence in COVID-19 patients on ECMO compared to other ECMO patients is not clear, but may be explained in part by the SARS-CoV-2 neurotropism hypothesis, or possibly by the intensification of anticoagulation in COVID-19 patients on ECMO [22, 26]. However, evidence for the link between anticoagulant dosing and bleeding remains limited for non-COVID patients on ECMO [11, 54], and therapeutic anticoagulation seems to be associated with only a non-significant trend for higher bleeding in COVID-19 patients [23,24,25, 55]. Finally, ICH was independently associated with mortality, in line with earlier studies on both COVID and non-COVID patients [12, 13, 27].
In addition to ICH, cannulation-related bleeding and ear nose and throat (ENT) bleeding accounted for more than a quarter of total events, but did not have a significant impact on in-hospital mortality. Compared to cannulation-related bleeds [12, 13], ENT bleeds, which are not included in the ELSO registry, have been rarely reported and their impact on mortality is largely unknown [11]. Moreover, the impact of the return cannula in a jugular position on the risk of ENT bleeding deserves further evaluation. In line with published data in non-COVID patients, pulmonary bleedings were frequent and independently associated with mortality [12, 13, 56]. Unlike previous reports, gastrointestinal bleeds, despite a trend towards higher mortality, did not reach statistical significance in multivariable analysis [12, 13].
Thrombosis incidence was lower than bleeding in our cohort, which contrasts with the recent ELSO report on VV-ECMO [12], even though our study included deep vein thrombosis and pulmonary embolism/thrombosis which are not recorded in the ELSO registry. Our results also differ from the high rates of thrombosis in early reports of COVID-19 patients on VV-ECMO [27, 28, 34]. Two factors might have influenced these results. First, as previously highlighted, intensification of anticoagulant dosing during the COVID-19 pandemic may have reduced thrombosis incidence, in particular circuit clotting and oxygenator failure [57]. Second, thrombosis reporting is highly dependent on clinical and radiological screening protocols. Systematic ultrasound or computed-tomography assessment of thrombosis on ECMO is likely accountable for the discrepancy between our results and recently published COVID-19 reports, especially regarding pulmonary embolism/thrombosis [27, 28, 34].
Unlike bleeding, neither overall thrombosis nor any thrombosis subtypes were significantly associated with in-hospital mortality. These results are partially in line with recent findings on COVID-19 ECMO patients [27] but differ from large multicenter studies in non-COVID ECMO patients which reported a significant impact of thrombosis on in-hospital survival, although weaker than bleeding [12, 13]. Two factors might explain these results. First, the use of a causal approach for model building using a directed acyclic graph (DAG) may have enabled a better control of confounding variables [38, 58]. Second, the smaller number of patients and events in our report might have underpowered the analysis.
We identified specific variables independently associated with the occurrence of bleeding or thrombosis. As already reported from the ELSO registry, the length of ECMO run was independently associated with both bleeding and thrombosis, supporting strategies aiming at minimizing ECMO duration, including daily assessment of readiness to liberate from ECMO [12, 13]. Longer duration of mechanical ventilation (MV) prior to ECMO (≥ 7 days) was also independently associated with increased risk of bleeding. This may reflect a higher disease severity, nutritional deficiencies, increased inflammation and endothelial activation. This may also help to explain the reported association between survival and duration of MV before ECMO in both COVID and non-COVID patients [17, 18, 46]. Finally, a high fibrinogen level (≥ 6 g/L) was associated with greater odds of thrombosis. Elevated fibrinogen levels have been associated with thrombosis risk in the general population [59, 60] but the evidence in ECMO patients remains scarce [61]. While fibrinogen, as inflammatory marker, is associated with COVID-19 severity and mortality [62], its ability to predict thrombosis appears low [39]. To date, only one single-center study, though limited in size, reported an association between high fibrinogen levels and thrombosis in COVID-19 patients supported by VV-ECMO [63].
Finally, we reported anticoagulation management practice during ECMO support at a nationwide level. As previously reported in an international survey [64], and in accordance with current international guidelines [65], the vast majority of the patients received a systemic anticoagulation, with unfractionated heparin being the drug of choice. Heparin was essentially monitored using anti-factor Xa activity, which contrasts with the international practice in adult ECMO [64]. Antithrombin monitoring and supplementation, though significant, was lower than previously published [64], which might reflect the negative results of a recent randomized control trial [66].
Our study has several strengths. First, we report bleeding and thrombosis for the first time in a large multicenter sample of COVID-19 patients, at a nationwide level. The excellent adherence to recommended medical interventions in ARDS patient management during the pre-ECMO period supports the generalizability of our results. Second, our registry captured data regarding ENT bleeding, venous thromboembolism and anticoagulation management practice that are not collected by the ELSO registry. Third, the use of a causal approach for multivariable model building and the sustained effect of bleeding on mortality up to day 90 strengthens confidence in our results.
Although the multicenter nature of this study prevented us from collecting high frequency clinical and biological data on ECMO, we were able to report important data regarding coagulation management, hitherto unpublished. These data highlight the considerable heterogeneity of practices and underline (1) the need for harmonization of procedures and practices across centers regarding hemostasis management on ECMO and (2) the crucial need for prospective interventional studies of anticoagulation management during both VA and VV-ECMO. To this extent, we believe our study reports valuable data that might help setting up prospective interventional studies.
Limitations
Our study has several limitations. The observational nature of this study prevented us from inferring causality. The timing of bleeding and thrombotic events occurrence was not available and sequential assessment of anticoagulation, ECMO parameters and biological markers on ECMO was not collected, precluding any time-to-event analysis. In addition, D-dimer levels, though described as markers of disease severity and thrombotic risk, were not available. Finally, the absence of systematic screening protocols for both bleeding and thrombosis before and during ECMO might have led to under-reporting of these events.
Conclusions
In a large nationwide cohort of patients supported by ECMO for severe COVID-19, bleeding incidence was high and associated with mortality. Besides, intracranial hemorrhage carried the highest risk of death. Thrombotic events were less frequent and were not associated with mortality. Length of ECMO support was associated with a higher risk of both bleeding and thrombosis, supporting the development and use of strategies to minimize ECMO duration. Our results highlight the need for harmonization of practices across centers regarding hemostasis management on ECMO and for prospective studies to evaluate anticoagulation strategies during ECMO support.
References
Quintel M, Bartlett RH, Grocott MPW et al (2020) Extracorporeal membrane oxygenation for respiratory failure. Anesthesiology 132:1257–1276. https://doi.org/10.1097/aln.0000000000003221
Guglin M, Zucker MJ, Bazan VM et al (2019) Venoarterial ECMO for adults JACC scientific expert panel. J Am Coll Cardiol 73:698–716. https://doi.org/10.1016/j.jacc.2018.11.038
Combes A, Hajage D, Capellier G et al (2018) Extracorporeal membrane oxygenation for severe acute respiratory distress syndrome. New Engl J Med 378:1965–1975. https://doi.org/10.1056/nejmoa1800385
Combes A, Schmidt M, Hodgson CL et al (2020) Extracorporeal life support for adults with acute respiratory distress syndrome. Intens Care Med 46:2464–2476. https://doi.org/10.1007/s00134-020-06290-1
Chlebowski MM, Baltagi S, Carlson M et al (2020) Clinical controversies in anticoagulation monitoring and antithrombin supplementation for ECMO. Crit Care Lond Engl 24:19. https://doi.org/10.1186/s13054-020-2726-9
Melehy A, Ning Y, Kurlansky P et al (2021) Bleeding and thrombotic events during extracorporeal membrane oxygenation for postcardiotomy shock. Ann Thorac Surg. https://doi.org/10.1016/j.athoracsur.2021.02.008
Ellouze O, Abbad X, Constandache T et al (2021) Risk factors of bleeding in patients undergoing venoarterial extracorporeal membrane oxygenation. Ann Thorac Surg 111:623–628. https://doi.org/10.1016/j.athoracsur.2020.02.012
Bidar F, Lancelot A, Lebreton G et al (2021) Venous or arterial thromboses after venoarterial extracorporeal membrane oxygenation support: frequency and risk factors. J Hear Lung Transplant 40:307–315. https://doi.org/10.1016/j.healun.2020.12.007
Guennec LL, Cholet C, Huang F et al (2018) Ischemic and hemorrhagic brain injury during venoarterial-extracorporeal membrane oxygenation. Ann Intensive Care 8:129. https://doi.org/10.1186/s13613-018-0475-6
Luyt C-E, Bréchot N, Demondion P et al (2016) Brain injury during venovenous extracorporeal membrane oxygenation. Intens Care Med 42:897–907. https://doi.org/10.1007/s00134-016-4318-3
Aubron C, DePuydt J, Belon F et al (2016) Predictive factors of bleeding events in adults undergoing extracorporeal membrane oxygenation. Ann Intensive Care 6:97. https://doi.org/10.1186/s13613-016-0196-7
Nunez JI, Gosling AF, O’Gara B et al (2021) Bleeding and thrombotic events in adults supported with venovenous extracorporeal membrane oxygenation: an ELSO registry analysis. Intens Care Med. https://doi.org/10.1007/s00134-021-06593-x
Chung M, Cabezas FR, Nunez JI et al (2020) Hemocompatibility-related adverse events and survival on venoarterial extracorporeal life support an ELSO registry analysis. JACC Hear Fail 8:892–902. https://doi.org/10.1016/j.jchf.2020.09.004
Barbaro RP, MacLaren G, Boonstra PS et al (2021) Extracorporeal membrane oxygenation for COVID-19: evolving outcomes from the international Extracorporeal Life Support Organization Registry. Lancet Lond Engl 398:1230–1238. https://doi.org/10.1016/s0140-6736(21)01960-7
Lorusso R, Combes A, Coco VL et al (2021) ECMO for COVID-19 patients in Europe and Israel. Intens Care Med 47:344–348. https://doi.org/10.1007/s00134-020-06272-3
Shaefi S, Brenner SK, Gupta S et al (2021) Extracorporeal membrane oxygenation in patients with severe respiratory failure from COVID-19. Intens Care Med 47:208–221. https://doi.org/10.1007/s00134-020-06331-9
Nesseler N, Fadel G, Mansour A et al (2022) Extracorporeal membrane oxygenation for respiratory failure related to COVID-19: a nationwide cohort study. Anesthesiology 136:732–748. https://doi.org/10.1097/aln.0000000000004168
Urner M, Barnett AG, Bassi GL et al (2022) Venovenous extracorporeal membrane oxygenation in patients with acute covid-19 associated respiratory failure: comparative effectiveness study. Bmj 2022:e068723. https://doi.org/10.1136/bmj-2021-068723
Gorog DA, Storey RF, Gurbel PA et al (2022) Current and novel biomarkers of thrombotic risk in COVID-19: a consensus statement from the international COVID-19 thrombosis biomarkers colloquium. Nat Rev Cardiol. https://doi.org/10.1038/s41569-021-00665-7
Bonaventura A, Vecchié A, Dagna L et al (2021) Endothelial dysfunction and immunothrombosis as key pathogenic mechanisms in COVID-19. Nat Rev Immunol 21:319–329. https://doi.org/10.1038/s41577-021-00536-9
Xiong X, Chi J, Gao Q (2021) Prevalence and risk factors of thrombotic events on patients with COVID-19: a systematic review and meta-analysis. Thrombosis J 19:32. https://doi.org/10.1186/s12959-021-00284-9
Susen S, Tacquard CA, Godon A et al (2020) Prevention of thrombotic risk in hospitalized patients with COVID-19 and hemostasis monitoring. Crit Care Lond Engl 24:364. https://doi.org/10.1186/s13054-020-03000-7
Sholzberg M, Tang GH, Rahhal H et al (2021) Effectiveness of therapeutic heparin versus prophylactic heparin on death, mechanical ventilation, or intensive care unit admission in moderately ill patients with covid-19 admitted to hospital: RAPID randomised clinical trial. BMJ 375:n2400. https://doi.org/10.1136/bmj.n2400
Spyropoulos AC, Goldin M, Giannis D et al (2021) Efficacy and safety of therapeutic-dose heparin vs standard prophylactic or intermediate-dose heparins for thromboprophylaxis in high-risk hospitalized patients with COVID-19: the HEP-COVID randomized clinical trial. Jama Intern Med 181:1612–1620. https://doi.org/10.1001/jamainternmed.2021.6203
Investigators A, Investigators A-4a, Investigators R-C et al (2021) Therapeutic anticoagulation with heparin in noncritically Ill patients with Covid-19. New Engl J Med 385:790–802. https://doi.org/10.1056/nejmoa2105911
Shekar K, Badulak J, Peek G et al (2020) Extracorporeal life support organization COVID-19 interim Guidelines. Asaio J Am Soc Artif Intern Organs 1992 66:707–721. https://doi.org/10.1097/mat.0000000000001193
Arachchillage DJ, Rajakaruna I, Scott I et al (2022) Impact of major bleeding and thrombosis on 180-day survival in patients with severe COVID-19 supported with veno-venous extracorporeal membrane oxygenation in the United Kingdom: a multicentre observational study. Brit J Haematol 196:566–576. https://doi.org/10.1111/bjh.17870
Weatherill A, Laffan M, Gasper M et al (2021) Impact of thrombosis and bleeding in patients with severe COVID-19 versus other viral pneumonias in the context of extracorporeal membrane oxygenation. Semin Thromb Hemost. https://doi.org/10.1055/s-0041-1732371
Bermea RS, Raz Y, Sertic F et al (2021) Increased intracranial hemorrhage amid elevated inflammatory markers in those with COVID-19 supported with extracorporeal membrane oxygenation. Shock 56:206–214. https://doi.org/10.1097/shk.0000000000001730
Doyle AJ, Hunt BJ, Sanderson B, et al (2021) A comparison of thrombosis and hemorrhage rates in patients with severe respiratory failure due to coronavirus disease 2019 and influenza requiring extracorporeal membrane oxygenation. Crit Care Med Publish 2021:e663–e672. https://doi.org/10.1097/ccm.0000000000004971
Pantel T, Roedl K, Jarczak D et al (2021) Association of COVID-19 with intracranial hemorrhage during extracorporeal membrane oxygenation for acute respiratory distress syndrome: a 10-year retrospective observational study. J Clin Med 11:28. https://doi.org/10.3390/jcm11010028
Ripoll B, Rubino A, Besser M et al (2021) Observational study of thrombosis and bleeding in COVID-19 VV ECMO patients. Int J Artif Organs. https://doi.org/10.1177/0391398821989065
Durak K, Kersten A, Grottke O et al (2021) Thromboembolic and bleeding events in COVID-19 patients receiving extracorporeal membrane oxygenation. Thorac Cardiovasc Surg 69:526–536. https://doi.org/10.1055/s-0041-1725180
Weir-McCall JR, Galea G, Mak SM et al (2021) Vascular thrombosis in severe Coronavirus Disease 2019 requiring extracorporeal membrane oxygenation: a multicenter study. Crit Care Med Publish. https://doi.org/10.1097/ccm.0000000000005322
Seeliger B, Doebler M, Hofmaenner DA et al (2022) Intracranial Hemorrhages on extracorporeal membrane oxygenation: differences between COVID-19 and other viral acute respiratory distress syndrome. Crit Care Med. https://doi.org/10.1097/ccm.0000000000005441
Al-Samkari H, Leaf RSK, Dzik WH et al (2020) COVID-19 and coagulation: bleeding and thrombotic manifestations of SARS-CoV-2 infection. Blood 136:489–500. https://doi.org/10.1182/blood.2020006520
Demelo-Rodriguez P, Farfán-Sedano AI, Pedrajas JM et al (2021) Bleeding risk in hospitalized patients with COVID-19 receiving intermediate- or therapeutic doses of thromboprophylaxis. J Thrombosis Haemostasis Jth 19:1981–1989. https://doi.org/10.1111/jth.15400
Gaskell AL, Sleigh JW (2020) An introduction to causal diagrams for anesthesiology research. Anesthesiology 132:951–967. https://doi.org/10.1097/aln.0000000000003193
Tacquard C, Mansour A, Godon A et al (2021) Impact of high-dose prophylactic anticoagulation in critically ill patients with COVID-19 pneumonia. Chest 159:2417–2427. https://doi.org/10.1016/j.chest.2021.01.017
Halaby R, Cuker A, Yui J et al (2021) Bleeding risk by intensity of anticoagulation in critically ill patients with COVID-19: a retrospective cohort study. J Thromb Haemost 19:1533–1545. https://doi.org/10.1111/jth.15310
Dalton HJ, Reeder R, Garcia-Filion P et al (2017) Factors associated with bleeding and thrombosis in children receiving extracorporeal membrane oxygenation. Am J Resp Crit Care 196:762–771. https://doi.org/10.1164/rccm.201609-1945oc
Lorusso R, Gelsomino S, Parise O et al (2017) Neurologic injury in adults supported with veno-venous extracorporeal membrane oxygenation for respiratory failure. Crit Care Med 45:1389–1397. https://doi.org/10.1097/ccm.0000000000002502
Fisser C, Reichenbächer C, Müller T et al (2019) Incidence and risk factors for cannula-related venous thrombosis after venovenous extracorporeal membrane oxygenation in adult patients with acute respiratory failure. Crit Care Med 47:332. https://doi.org/10.1097/CCM.0000000000003650
Parzy G, Daviet F, Persico N et al (2020) Prevalence and risk factors for thrombotic complications following venovenous extracorporeal membrane oxygenation: a CT scan study*. Crit Care Med 48:192–199. https://doi.org/10.1097/ccm.0000000000004129
Gómez CA, Sun C-K, Tsai I-T et al (2021) Mortality and risk factors associated with pulmonary embolism in coronavirus disease 2019 patients: a systematic review and meta-analysis. Sci Rep-UK 11:16025. https://doi.org/10.1038/s41598-021-95512-7
Schmidt M, Bailey M, Sheldrake J et al (2014) Predicting survival after extracorporeal membrane oxygenation for severe acute respiratory failure. The Respiratory Extracorporeal Membrane Oxygenation Survival Prediction (RESP) score. Am J Respir Crit Care Med 189:1374–1382. https://doi.org/10.1164/rccm.201311-2023oc
Schmidt M, Langouet E, Hajage D et al (2021) Evolving outcomes of extracorporeal membrane oxygenation support for severe COVID-19 ARDS in Sorbonne hospitals. Paris Crit Care Lond Engl 25:355. https://doi.org/10.1186/s13054-021-03780-6
Horby P, Lim WS, Emberson JR et al (2021) Dexamethasone in hospitalized patients with Covid-19. New Engl J Med 384:693–704. https://doi.org/10.1056/nejmoa2021436
Karagiannidis C, Hentschker C, Westhoff M et al (2022) Observational study of changes in utilization and outcomes in mechanical ventilation in COVID-19. PLoS ONE 17:e0262315. https://doi.org/10.1371/journal.pone.0262315
Friedrichson B, Kloka JA, Neef V et al (2022) Extracorporeal membrane oxygenation in coronavirus disease 2019: a nationwide cohort analysis of 4279 runs from Germany. Eur J Anaesth 39:445–451. https://doi.org/10.1097/eja.0000000000001670
Karagiannidis C, Slutsky AS, Bein T et al (2021) Complete countrywide mortality in COVID patients receiving ECMO in Germany throughout the first three waves of the pandemic. Crit Care Lond Engl 25:413. https://doi.org/10.1186/s13054-021-03831-y
Piroth L, Cottenet J, Mariet A-S et al (2021) Comparison of the characteristics, morbidity, and mortality of COVID-19 and seasonal influenza: a nationwide, population-based retrospective cohort study. Lancet Respir Med 9:251–259. https://doi.org/10.1016/s2213-2600(20)30527-0
Schmidbauer ML, Ferse C, Salih F et al (2022) COVID-19 and intracranial hemorrhage: a multicenter case series, systematic review and pooled analysis. J Clin Med 11:605. https://doi.org/10.3390/jcm11030605
Lansink-Hartgring AO, de Vries AJ, Droogh JM, van den Bergh WM (2019) Hemorrhagic complications during extracorporeal membrane oxygenation—the role of anticoagulation and platelets. J Crit Care 54:239–243. https://doi.org/10.1016/j.jcrc.2019.09.013
Melmed KR, Cao M, Dogra S et al (2021) Risk factors for intracerebral hemorrhage in patients with COVID-19. J Thromb Thrombolys 51:953–960. https://doi.org/10.1007/s11239-020-02288-0
Ried M, Sommerauer L, Lubnow M et al (2018) Thoracic bleeding complications in patients with venovenous extracorporeal membrane oxygenation. Ann Thorac Surg 106:1668–1674. https://doi.org/10.1016/j.athoracsur.2018.07.020
Seeliger B, Döbler M, Friedrich R et al (2020) Comparison of anticoagulation strategies for veno-venous ECMO support in acute respiratory failure. Crit Care 24:701. https://doi.org/10.1186/s13054-020-03348-w
Heinze G, Dunkler D (2017) Five myths about variable selection. Transplant Int 30:6–10. https://doi.org/10.1111/tri.12895
Klovaite J, Nordestgaard BG, Tybjærg-Hansen A, Benn M (2013) Elevated fibrinogen levels are associated with risk of pulmonary embolism, but not with deep venous thrombosis. Am J Resp Crit Care 187:286–293. https://doi.org/10.1164/rccm.201207-1232oc
Vlieg AVH, Rosendaal FR (2003) High levels of fibrinogen are associated with the risk of deep venous thrombosis mainly in the elderly. J Thromb Haemost 1:2677–2678. https://doi.org/10.1111/j.1538-7836.2003.0543b.x
Roth S, Jansen C, M’Pembele R et al (2021) Fibrinogen–Albumin-Ratio is an independent predictor of thromboembolic complications in patients undergoing VA-ECMO. Sci Rep-UK 11:16648. https://doi.org/10.1038/s41598-021-95689-x
Leentjens J, van Haaps TF, Wessels PF et al (2021) COVID-19-associated coagulopathy and antithrombotic agents—lessons after 1 year. Lancet Haematol 8:e524–e533. https://doi.org/10.1016/s2352-3026(21)00105-8
Chandel A, Patolia S, Looby M et al (2021) Association of D-dimer and fibrinogen with hypercoagulability in COVID-19 requiring extracorporeal membrane oxygenation. J Intensive Care Med 36:689–695. https://doi.org/10.1177/0885066621997039
Protti A, Iapichino GE, Nardo MD et al (2020) Anticoagulation management and antithrombin supplementation practice during veno-venous extracorporeal membrane oxygenation: a worldwide survey. Anesthesiology 132:562–570. https://doi.org/10.1097/aln.0000000000003044
McMichael ABV, Ryerson LM, Ratano D et al (2022) 2021 ELSO adult and pediatric anticoagulation guidelines. Asaio J Publish. https://doi.org/10.1097/mat.0000000000001652
Panigada M, Cucino A, Spinelli E et al (2020) A randomized controlled trial of antithrombin supplementation during extracorporeal membrane oxygenation. Crit Care Med 48:1636–1644. https://doi.org/10.1097/ccm.0000000000004590
Acknowledgements
The authors thank Sebastien Rosier for assistance during the preparation of the manuscript. The authors thank the French society of thoracic and cardio-vascular surgery (Société Française de Chirurgie Thoracique et Cardio-Vasculaire, SFCTCV), the French society of thoracic and cardio-vascular critical care and anesthesia (Anesthésie-Réanimation Coeur-Thorax-Vaisseaux, ARCOTHOVA) and the French society of anesthesiology and critical care medicine (Société Française d’Anesthésie-Réanimation, SFAR) research network for endorsing the ECMOSARS registry. ECMOSARS Investigators (list of collaborators): Marc PIERROT, M.D., University Hospital of Angers, collected data, provided and cared for study patients. Sidney CHOCRON, M.D., Ph.D., University Hospital of Besançon, Professor,collected data, provided and cared for study patients. Guillaume FLICOTEAUX, M.D., University Hospital of Besançon, collected data, provided and cared for study patients. Philippe MAURIAT, M.D., University Hospital of Bordeaux, critically reviewed the study proposal. Alexandre OUATTARA, M.D., Ph.D., University Hospital of Bordeaux, collected data, provided and cared for study patients. Hadrien ROZE, M.D., University Hospital of Bordeaux, collected data, provided and cared for study patients. Olivier HUET, M.D., Ph.D., University Hospital of Brest, Professor, collected data, provided and cared for study patients. Marc-Olivier FISCHER, M.D., Ph.D., University Hospital of Caen, Professor, collected data, provided and cared for study patients. Claire ALESSANDRI, M.D., APHP University Hospital Henri Mondor, Créteil provided and cared for study patients. Raphel BELLAÏCHE M.D., APHP University Hospital Henri Mondor, Créteil provided and cared for study patients. Ophélie CONSTANT, M.D., APHP University Hospital Henri Mondor, Créteil provided and cared for study patients. Quentin DE ROUX, M.D., APHP University Hospital Henri Mondor, Créteil provided and cared for study patients. André LY, M.D., APHP University Hospital Henri Mondor, Créteil provided and cared for study patients. Arnaud MEFFERT, M.D., APHP University Hospital Henri Mondor, Créteil provided and cared for study patients. Jean-Claude MERLE, M.D., APHP University Hospital Henri Mondor, Créteil provided and cared for study patients. Nicolas MONGARDON, M.D., Ph.D., APHP University Hospital Henri Mondor, Créteil provided and cared for study patients. Lucile PICARD, M.D., APHP University Hospital Henri Mondor, Créteil provided and cared for study patients. Elena SKRIPKINA, M.D, APHP University Hospital Henri Mondor, Créteil provided and cared for study patients. Thierry FOLLIGUET, M.D., Ph.D., APHP University Hospital Henri Mondor, Créteil, Professor, provided and cared for study patients. Antonio FIORE, M.D., APHP University Hospital Henri Mondor, Créteil provided and cared for study patients. . Nicolas D'OSTREVY, M.D., University Hospital of Clermont-Ferrand, collected data, provided and cared for study patients. Marie-Catherine MORGAN, M.D., University Hospital of Dijon, collected data, provided and cared for study patients. Pierre-Grégoire GUINOT, M.D., Ph.D., University Hospital of Dijon, collected data, provided and cared for study patients. Maxime NGUYEN, M.D., University Hospital of Dijon, collected data, provided and cared for study patients. Lucie GAIDE-CHEVRONNAY, M.D., University Hospital of Grenoble, collected data, provided and cared for study patients. Nicolas TERZI, M.D., Ph.D., University Hospital of Grenoble, Professor, collected data, provided and cared for study patients. Dr Gwenhaël COLIN, Vendée Hospital, La Roche-sur-Yon, collected data, provided and cared for study patients. Dr Olivier FABRE, Hospital of Lens, collected data, provided and cared for study patients. Arash ASTANEH, M.D., Marie-Lannelongue Hospital, Le Plessis-Robinson ollected data, provided and cared for study patients. Justin ISSARD, M.D., Marie-Lannelongue Hospital, Le Plessis-Robin son collected data, provided and cared for study patients. Elie FADEL, M.D., Ph.D., Marie-Lannelongue Hospital, Le Plessis-Robinson, Professor, collected data, provided and cared for study patients. Dominique FABRE, M.D., Marie-Lannelongue Hospital, Le Plessis-Robinson collected data, provided and cared for study patients. Antoine GIRAULT, M.D., Marie-Lannelongue Hospital, Le Plessis-Robinson collected data, provided and cared for study patients. Julien GUIHAIRE, M.D., Ph.D., Marie-Lannelongue Hospital, Le Plessis-Robinson collected data, provided and cared for study patients. Iolande ION, M.D., Marie-Lannelongue Hospital, Le Plessis-Robinson collected data, provided and cared for study patients. Jean Baptiste MENAGER, M.D., Marie-Lannelongue Hospital, Le Plessis-Robinson collected data, provided and cared for study patients. Delphine MITILIAN, M.D., Marie-Lannelongue Hospital, Le Plessis-Robinson collected data, provided and cared for study patients. Olaf MERCIER, M.D., Ph.D., Marie-Lannelongue Hospital, Le Plessis-Robinson, Professor, collected data, provided and cared for study patients. . François STEPHAN, M.D., Marie-Lannelongue Hospital, Le Plessis-Robinson, Professor, ollected data, provided and cared for study patients. Jacques THES, M.D., Marie-Lannelongue Hospital, Le Plessis-Robinson collected data, provided and cared for study patients. Jerôme JOUAN, M.D., University Hospital of Limoges, collected data, provided and cared for study patients. Thibault DUBURCQ, M.D., University Hospital of Lille collected data, provided and cared for study patients. Valentin LOOBUYCK, M.D., University Hospital of Lille collected data, provided and cared for study patients. Mouhammed MOUSSA, M.D., University Hospital of Lille collected data, provided and cared for study patients. Agnes MUGNIER, M.D., University Hospital of Lille collected data, provided and cared for study patients. Natacha ROUSSE, M.D., University Hospital of Lille collected data, provided and cared for study patients. Olivier DESEBBE, M.D., Clinique de la Sauvegarde, Lyon collected data, provided and cared for study patients. Jean-Luc FELLAHI, M.D., Ph.D., Hospices civils de Lyon, Professor, critically reviewed the study proposal, provided and cared for study patients. Roland HENAINE, M.D., Ph.D., Hospices civils de Lyon, Professor, critically reviewed the study proposal, provided and cared for study patients. Matteo POZZI, M.D, Hospices civils de Lyon collected data, provided and cared for study patients. Jean-Christophe RICHARD, M.D., Ph.D., Hospices civils de Lyon, Professor, collected data, provided and cared for study patients. Zakaria RIAD, M.D., Hospices civils de Lyon collected data, provided and cared for study patients. Christophe GUERVILLY, M.D., North Hospital, APHM, Marseille, collected data, provided and cared for study patients. Sami HRAIECH, M.D., North Hospital, APHM, Marseille, collected data, provided and cared for study patients. Laurent PAPAZIAN, M.D., Ph.D., North Hospital, APHM, Marseille, Professor, collected data, provided and cared for study patients. Matthias CASTANIER, M.D., European Hospital, Marseille collected data, provided and cared for study patients. Charles CHANAVAZ, M.D., Clairval Hospital, Marseille collected data, provided and cared for study patients. Cyril CADOZ, M.D., Regional Hospital of Metz-Thionville provided and cared for study patients. Sebastien GETTE, M.D., Regional Hospital of Metz-Thionville provided and cared for study patients. Guillaume LOUIS, M.D., Regional Hospital of Metz-Thionville provided and cared for study patients. Erick PORTOCARRERO, M.D., Regional Hospital of Metz-Thionville provided and cared for study patients. Philippe GAUDARD, M.D., Ph.D, Univeristy Hospiyal of Montpellier collected data, provided and cared for study patients. Kais BRINI, M.D., Institut Mutualiste Montsouris, Paris collected data, provided and cared for study patients. Nicolas BISCHOFF, M.D., Emile Muller Hospital, Mulhouse collected data, provided and cared for study patients. Antoine KIMMOUN, M.D., Ph.D., University Hospital of Nancy, Professor, collected data, provided and cared for study patients. Mathieu MATTEI, M.D., University Hospital of Nancy, collected data, provided and cared for study patients. Pierre PEREZ, M.D., University Hospital of Nancy, collected data, provided and cared for study patients. Alexandre BOURDIOL, M.D., University Hospital of Nantes, collected data, provided and cared for study patients. Yannick HOURMANT, M.D., University Hospital of Nantes, collected data, provided and cared for study patients. Pierre-Joachim MAHÉ, M.D., University Hospital of Nantes, collected data, provided and cared for study patients. Mickaël VOURC’H, M.D., University Hospital of Nantes, collected data, provided and cared for study patients. Stéphane AUBERT, M.D., Ambroise Paré Hospital, Neuilly-sur-Seine collected data, provided and cared for study patients. Florian BAZALGETTE, M.D., University hospital of Nîmes collected data, provided and cared for study patients. Claire ROGER, M.D., University hospital of Nîmes collected data, provided and cared for study patients. Pierre JAQUET, M.D., APHP, Hôpital Bichat-Claude Bernard, Paris University Hospital provided and cared for study patients. Brice LORTAT-JACOB, M.D., APHP, Hôpital Bichat-Claude Bernard, Paris University Hospital provided and cared for study patients. Pierre MORDANT, M.D., Ph.D., APHP, Hôpital Bichat-Claude Bernard, Paris University Hospital, Professor, provided and cared for study patients. Patrick NATAF, M.D., Ph.D., APHP, Hôpital Bichat-Claude Bernard, Paris University Hospital, Professor, provided and cared for study patients. Juliette PATRIER, M.D., Hôpital Bichat-Claude Bernard, Paris University Hospital provided and cared for study patients. Sophie PROVENCHÈRE, M.D., Ph.D., Hôpital Bichat-Claude Bernard, Paris University Hospital provided and cared for study patients. Morgan ROUÉ, M.D., APHP, Hôpital Bichat-Claude Bernard, Paris University Hospital provided and cared for study patients. Romain SONNEVILLE, M.D., Ph.D., APHP, Hôpital Bichat-Claude Bernard, Paris University Hospital, Professor, provided and cared for study patients. Alexy TRAN-DINH, M.D., Hôpital Bichat-Claude Bernard, Paris University Hospital provided and cared for study patients. Paul-Henri WICKY, M.D., APHP, Hôpital Bichat-Claude Bernard, Paris University Hospital provided and cared for study patients. Charles AL ZREIBI, M.D., APHP Hôpital Européen Georges Pompidou - Paris University Hospital collected data, provided and cared for study patients. Bernard CHOLLEY, M.D., Ph.D., APHP Hôpital Européen Georges Pompidou - Paris University Hospital, Professor, collected data, provided and cared for study patients. Yannis GUYONVARCh, M.D., APHP Hôpital Européen Georges Pompidou - Paris University Hospital collected data, provided and cared for study patients. Sophie HAMADA, M.D., APHP Hôpital Européen Georges Pompidou - Paris University Hospital collected data, provided and cared for study patients. Claudio BARBANTI, M.D., APHP Necker, Paris University Hospital collected data, provided and cared for study patients. Astrid BERTIER, M.D., APHP Le Kremlin-Bicêtre, Paris University Hospital collected data, provided and cared for study patients. Anatole HARROIS, M.D., APHP Le Kremlin-Bicêtre, Paris University Hospital collected data, provided and cared for study patients. Jordi MATIELLO, M.D., APHP Le Kremlin-Bicêtre, Paris University Hospital collected data, provided and cared for study patients. Thomas KERFORNE, M.D., University Hospital of Poitiers collected data, provided and cared for study patients. Corentin LACROIX, M.D., University Hospital of Poitiers collected data, provided and cared for study patients. Nicolas BRECHOT, M.D., APHP, Sorbonne Université, Hôpital Pitié–Salpêtrière, Paris, France collected data, provided and cared for study patients. Alain COMBES, M.D., Ph.D., APHP, Sorbonne Université, Hôpital Pitié–Salpêtrière, Paris, France, Professor, collected data, provided and cared for study patients. Juliette CHOMMELOUX, M.D., APHP, Sorbonne Université, Hôpital Pitié–Salpêtrière, Paris, France, collected data, provided and cared for study patients. Jean Michel CONSTANTIN, M.D., Ph.D., APHP, Sorbonne Université, Hôpital Pitié–Salpêtrière, Paris, France, Professor, collected data, provided and cared for study patients. Cosimo D’ALESSANDRO, M.D., APHP, Sorbonne Université, Hôpital Pitié–Salpêtrière, Paris, France collected data, provided and cared for study patients. Pierre DEMONDION, M.D., APHP, Sorbonne Université, Hôpital Pitié–Salpêtrière, Paris, France collected data, provided and cared for study patients. Alexandre DEMOULE, M.D., APHP, Sorbonne Université, Hôpital Pitié–Salpêtrière, Paris, France collected data, provided and cared for study patients. Martin DRES, M.D., APHP, Sorbonne Université, Hôpital Pitié–Salpêtrière, Paris, France collected data, provided and cared for study patients. Guillaume FADEL, M.D., APHP, Sorbonne Université, Hôpital Pitié–Salpêtrière, Paris, France collected data, provided and cared for study patients. Muriel FARTOUKH, M.D., APHP, Sorbonne Université, Hôpital Pitié–Salpêtrière, Paris, France collected data, provided and cared for study patients. Guillaume HEKIMIAN, M.D., APHP, Sorbonne Université, Hôpital Pitié–Salpêtrière, Paris, France collected data, provided and cared for study patients. Charles JUVIN, M.D., APHP, Sorbonne Université, Hôpital Pitié–Salpêtrière, Paris, France collected data, provided and cared for study patients. Pascal LEPRINCE, M.D., Ph.D., APHP, Sorbonne Université, Hôpital Pitié–Salpêtrière, Paris, France, Professor, collected data, provided and cared for study patients. David LEVY, M.D., APHP, Sorbonne Université, Hôpital Pitié–Salpêtrière, Paris, France collected data, provided and cared for study patients. Charles Edouard LUYT, M.D., Ph.D., APHP, Sorbonne Université, Hôpital Pitié–Salpêtrière, Paris, France, Professor, collected data, provided and cared for study patients. Marc PINETON DE CHAMBRUn, M.D., APHP, Sorbonne Université, Hôpital Pitié–Salpêtrière, Paris, France collected data, provided and cared for study patients. Thibaut SCHOELL, M.D., APHP, Sorbonne Université, Hôpital Pitié–Salpêtrière, Paris, France collected data, provided and cared for study patients. Pierre FILLÂTRE, M.D., Ph.D., Hospital of Saint-Brieuc Collected data, provided and cared for study patients. Nicolas MASSART, M.D., Hospital of Saint-Brieuc Collected data, provided and cared for study patients. Roxane NICOLAS, M.D., University Hospital of Saint-Etienne collected data, provided and cared for study patients. Maud JONAS, M.D., Saint-Nazaire Hospital collected data, provided and cared for study patients. Charles VIDAL, M.D., University Hospital of Saint-Denis, La Réunion collected data, provided and cared for study patients. Nicolas ALLOU, M.D., University Hospital of Saint-Denis, La Réunion collected data, provided and cared for study patients. Salvatore MUCCIO, M.D., University Hospital of Reims collected data, provided and cared for study patients. Dario DI PERNA, M.D., University Hospital of Reims collected data, provided and cared for study patients. Vito-Giovanni RUGGIERI, M.D., Ph.D., University Hospital of Reims collected data, provided and cared for study patients. Bruno MOURVILLIER, M.D., Ph.D., University Hospital of Reims, Professor, collected data, provided and cared for study patients. Amedeo ANSELMI, M.D., Ph.D., University Hospital of Rennes provided and cared for study patients. Karl BOUNADER, M.D., University Hospital of Rennes provided and cared for study patients. Yoann LAUNEY, M.D., Ph.D., University Hospital of Rennes provided and cared for study patients. Thomas LEBOUVIER, M.D., University Hospital of Rennes provided and cared for study patients. Alessandro PARASIDO, University Hospital of Rennes provided and cared for study patients. Florian REIZINE, M.D., University Hospital of Rennes provided and cared for study patients. Philippe SEGUIN, M.D., Ph.D., University Hospital of Rennes, Professor, provided and cared for study patients. Emmanuel BESNIER, M.D., University Hospital of Rouen, collected data, provided and cared for study patients. Dorothée CARPENTIER, M.D., University Hospital of Rouen, collected data, provided and cared for study patients. Thomas CLAVIER, M.D., University Hospital of Rouen, collected data, provided and cared for study patients. Pierre-Emmanuel FALCOZ, M.D., Ph.D., University Hospital of Strasbourg, Professor, collected data, provided and cared for study patients. Anne OLLAND, M.D., Ph.D., University Hospital of Strasbourg, Professor, collected data, provided and cared for study patients. Marion VILLARD, M.D., University Hospital of Strasbourg, collected data, provided and cared for study patients. Fanny BOUNES, M.D., University Hospital of Toulouse, collected data, provided and cared for study patients. François LABASTE, M.D., Ph.D., University Hospital of Toulouse, Professor, collected data, provided and cared for study patients. Vincent MINVILLE, M.D., Ph.D., University Hospital of Toulouse, Professor, collected data, provided and cared for study patients. Antoine GUILLON, M.D., University Hospital of Tours, collected data, provided and cared for study patients. Yannick FEDUN, M.D., Bretagne Atlantique Hospital, Vannes, collected data, provided and cared for study patients.
Funding
This work was supported by a grant from the university hospital of Rennes (Appel à projets CFTR2) and by a grant from the French society of thoracic and cardio-vascular surgery (Société française de chirurgie thoracique et cardio-vasculaire, Bourse Marc Laskar).
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflicts of interest
AM received payments made to his institution from i-SEP for consulting fees, and LFB for lecture fees. EF declares no competing interests. MS received consultancy fees from Getinge, Xenios FMC and Drager. BR declares no competing interests. IG-T declares no competing interests. ME declares no competing interests. CF declares no competing interests. BL received personal fees from Abiomed, Gettinge, Baxter, Novartis, Sanofi, Amomed, and Orion. AP declares no competing interests. JTR declares no competing interests. MP declares no competing interests. SM declares no competing interests. GL reports lecture fees from Livanova and Abiomed. AV declares no competing interests. NN declares no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The ECMOSARS Investigators Collaborators members are listed in the Acknowledgement section.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Mansour, A., Flecher, E., Schmidt, M. et al. Bleeding and thrombotic events in patients with severe COVID-19 supported with extracorporeal membrane oxygenation: a nationwide cohort study. Intensive Care Med 48, 1039–1052 (2022). https://doi.org/10.1007/s00134-022-06794-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-022-06794-y