Abstract
Purpose
To assess the impact of lung ultrasound (LU) on clinical decision making in mechanically ventilated critically ill patients.
Methods
One hundred and eighty-nine patients took part in this prospective study. The patients were enrolled in the study when LU was requested by the primary physician for (1) unexplained deterioration of arterial blood gases and (2) a suspected pathologic entity [pneumothorax, significant pleural effusion (including parapneumonic effusion, empyema, or hemothorax), unilateral atelectasis (lobar or total), pneumonia and diffuse interstitial syndrome (pulmonary edema)].
Results
Two hundred and fifty-three LU examinations were performed; 108 studies (42.7 %) were performed for unexplained deterioration of arterial blood gases, and 145 (57.3 %) for a suspected pathologic entity (60 for pneumothorax, 34 for significant pleural effusion, 22 for diffuse interstitial syndrome, 15 for unilateral lobar or total lung atelectasis, and 14 for pneumonia). The net reclassification index was 85.6 %, indicating that LU significantly influenced the decision-making process. The management was changed directly as a result of information provided by the LU in 119 out of 253 cases (47 %). In 81 cases, the change in patient management involved invasive interventions (chest tube, bronchoscopy, diagnostic thoracentesis/fluid drainage, continuous venous–venous hemofiltration, abdominal decompression, tracheotomy), and in 38 cases, non-invasive (PEEP change/titration, recruitment maneuver, diuretics, physiotherapy, change in bed position, antibiotics initiation/change). In 53 out of 253 cases (21 %), LU revealed findings which supported diagnoses not suspected by the primary physician (7 cases of pneumothorax, 9 of significant pleural effusion, 9 of pneumonia, 16 of unilateral atelectasis, and 12 of diffuse interstitial syndrome).
Conclusion
Our study shows that LU has a significant impact on decision making and therapeutic management.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Lung ultrasound (LU) has emerged in recent years as a powerful diagnostic tool, and as such it is increasingly used in patients managed in intensive care units (ICUs). As a bedside non-invasive test with an excellent safety profile, LU can be performed repeatedly. Thus, it is an attractive alternative imaging technique for patients on whom thoracic computed tomography (CT) cannot be performed on a routine basis or where chest X-ray presents serious limitations in terms of sensitivity and specificity of identifying lung pathologies [1, 2].
We have shown recently that in a mixed surgical–medical ICU population of mechanically ventilated critically ill patients, LU identifies (with high diagnostic accuracy) the most common pathological abnormalities of the respiratory system encountered in these patients. Indeed, this technique has a diagnostic accuracy of 92–100 % in identifying pneumothorax, consolidation, interstitial syndrome, and pleural effusion, and may therefore be considered an alternative to thoracic CT for critically ill patients [2]. In addition, it has been shown that on appropriate clinical grounds, LU may be of help in the diagnosis of pneumonia and to follow its course [3–5]. Nevertheless, the impact of LU on decision making, in the process of addressing specific clinical questions related to these pathologic entities, is not entirely clear. The aim of this study was to examine the impact of performing LU on clinical decision making in mechanically ventilated critically ill patients.
Methods
This study was conducted in a medical–surgical ICU. The hospital ethics committee approved the study and waived the requirement for informed consent.
One hundred and eighty-nine mechanically ventilated patients were involved in this prospective study. The patients were enrolled in the study when (a) LU was requested by the primary physician to address five questions related to corresponding suspected pathologic entities and (b) a single LU operator (NX) was available. The following questions were posed: (1) Does the patient have LU findings compatible with the diagnosis of pneumothorax (Q1)? (2) Is significant pleural effusion (including parapneumonic effusion, empyema, or hemothorax) present (Q2)? (3) Does this patient have LU findings compatible with the diagnosis of unilateral major consolidation/atelectasis (lobar or total lung) (Q3)? (4) Does this patient have LU findings compatible with the diagnosis of pneumonia (Q4)? (5) Does this patient have LU findings compatible with diffuse pulmonary edema of cardiogenic or non-cardiogenic origin (Q5, interstitial syndrome)? These five questions, as judged by the primary physician, and based on clinical and laboratory grounds, were linked to the patient’s current status. In addition, since all these pathologies may cause derangement of arterial blood gases, LU was also requested by the primary physician for unexplained and persistent deterioration of arterial blood gases (hypoxemia and/or hypercapnia, QABG). The LU operator presented the information to the primary physician and was not involved in the decision-making process.
Lung ultrasound
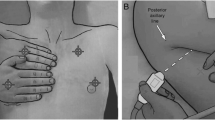
Visualization of the lungs was performed using a microconvex 5–9 MHz transducer, appropriate for transthoracic examination (Hitachi EUB 8500), as described previously [2]. Access to standardized images (seashore sign, stratosphere sign) was possible. LU was performed with the patient in the supine and semi-lateral position, using a specific previously validated protocol [2]. The normal lung generates lung sliding and A lines (repetition lines parallel to the pleural line) [6–8].
Pneumothorax was diagnosed when the A line sign (only A lines visible) was associated with the stratosphere sign (complete abolition of lung sliding; the lung sliding in M-mode results in a sandy pattern, arising exactly from the pleural line). Local lung sliding, or B lines, exclude the diagnosis [9, 10]. The lung point sign [the fleeting appearance of a lung pattern (lung sliding or pathologic comet-tail artifacts) replacing a pneumothorax pattern (absent lung sliding plus exclusive horizontal lines) in a particular location of the chest wall], specific for pneumothorax, was additionally used [11]. LU findings of lung overdistension, which may be misclassified as compatible with pneumothorax, included the absence of lung point and predominance of A line static profile associated with lung sliding and remarkable diaphragmatic depression.
Pleural effusion was determined as a hypoechoic or echoic structure. The power Doppler and quad sign (the pleural effusion is delineated by the pleural line, the shadow of the ribs, and mostly the lung line) and sinusoid sign (on M mode the lung line moves toward the pleural line) on inspiration were used for pleural effusion differentiation. For hemothorax, the plankton sign was additionally used (multiple echoes, mobile and whirling in real-time in pleural space) [2, 6, 12].
Consolidation/atelectasis was defined as an isoechoic tissue-like structure which is caused by the loss of lung aeration [13]. The following signs were used to characterize a specific lung area as atelectatic: lung sliding abolition; abolition of dynamic diaphragm movement and its elevation (more than 2 cm); the presence of a static air bronchogram within the consolidation; heart sign, and the presence of small pleural effusion. The lung pulse sign (the association of absent lung sliding with the perception of heart activity at the pleural line) was also used in the cases of complete total lung atelectasis (i.e., due to right or left main bronchus intubation) [14, 15]. A static air bronchogram was defined as hyperechoic punctiform images produced by trapped air, no longer aerated, inside a lung area. Posterolateral alveolar consolidation and/or pleural effusion was defined as PLAPS [3].
Pneumonia was characterized by (1) the presence of a bilateral or local B line pattern with or without lung sliding, (2) irregular boundaries created by the adjacent aerated lung (provided that an entire lobe was not affected), (3) vascular flow seen as a branching pattern in color or power Doppler imaging, and (4) the presence of anterior lung consolidation with hyperechoic punctiform images within a lung area (dynamic air bronchogram) [3–5]. The dynamic air bronchogram (punctiform or linear hyperechoic artifacts) is characterized by the presence of dynamic lung movement during the respiratory cycle. This sign is usually associated with a non-retractile consolidation (i.e., not atelectasis) and indicates that this consolidation is pneumonia [16].
Interstitial syndrome was defined as the presence of multiple B lines in a specific lung area. B lines are well-defined hyperechoic comet-tail artifacts, arising from the pleural line and spreading up indefinitely, erasing A lines and moving with the lung sliding when lung sliding is present. The B lines, 7 ± 1 mm apart, indicate thickening of the interlobular septa (B7 lines) and 3 ± 1 mm apart indicate ground glass areas (B3 lines), as previously described. White lung was defined as completely white echographic lung fields with coalescent B lines and no horizontal reverberation [7, 8, 17–19].
Data analysis
The yield of LU was defined in each clinical problem as the percentage of studies that either had positive findings with diagnostic implications or confidently excluded the suspected diagnosis. The findings from the LU were classified as either expected or unexpected by the primary physician. The net reclassification improvement (NRI) was used to assess the impact of LU on clinical decision making [20, 21]. In this calculation we defined an event or non-event as the agreement or disagreement between LU findings and clinical diagnosis of the primary physician, respectively. Further analysis was based on the influence [which included therapeutic or non-therapeutic (no action) interventions] and non-influence of LU on the decision-making process. NRI (expressed as %) was calculated as follows:
where P up events is the number of event cases in which LU influenced the decision-making process/number of event cases. P down events is the number of event cases in which LU did not influence the decision-making process/number of events cases. P up nonevent is the number of non-event cases in which LU influenced the decision-making process/number of non-event cases. P down nonevent is the number of non-event cases in which LU did not influence the decision-making process/number of non-event cases.
Results
Two hundred and fifty-three LU studies were performed in 189 mechanically ventilated patients (see Electronic Supplementary Material for demographics and clinical characteristics of the patients). In all but one LU study, pathologic findings were observed. These findings were mainly compatible with consolidation (n = 223), pleural effusion (n = 221), and interstitial syndrome (n = 189). A general flow chart of the study is shown in Fig. 1.
Study flow chart. Lung ultrasound (LU). Q 1 Does this patient have LU findings compatible with the diagnosis of pneumothorax? Q 2 Is significant pleural effusion (including parapneumonic effusion, empyema, or hemothorax) present? Q 3 Does this patient have LU findings compatible with the diagnosis of unilateral major consolidation/atelectasis (lobar or total lung)? Q 4 Does this patient have LU findings compatible with the diagnosis of pneumonia? Q 5 Does this patient have LU findings compatible with diffuse pulmonary edema of cardiogenic or non-cardiogenic origin (interstitial syndrome)? Q ABG LU examination for unexplained and persistent deterioration of arterial blood gases. See text for explanation of net reclassification index
NRI was 85.6 %, indicating that LU had a high impact on the decision-making process. Figures 2, 3, 4, 5, 6, and 7, as well as figure legends, show in detail the results of LU in addressing each of the six prespecified clinical questions. Overall, 108 studies (42.7 %) were performed for unexplained deterioration of arterial blood gases (QABG) and 145 (57.3 %) for a suspected pathological entity (Q1–Q5). When LU was performed for a suspected pathologic entity, the LU findings were compatible with the primary physician’s clinical suspicion in 69.7 % of cases, while ten cases (6.9 %) supported something other than the suspected entity (Figs. 2, 3, 4, 5, 6). In the remaining 34 cases (23.4 %), the LU findings did not categorically support any of these pathologies and reflected the LU abnormalities usually encountered in mechanically ventilated critically ill patients (i.e., bilateral consolidation of dependent lung zone, bilateral pleural effusion, diffuse B lines).
Lung ultrasound (LU) performed for question Q1. Seven additional cases of pneumothorax were diagnosed when LU was performed for questions other than Q1 (all from QABG group). a Stratosphere sign (arrow). b Lung point—the fleeting appearance of a lung pattern (lung sliding or pathologic comet-tail artifacts) replacing a pneumothorax pattern (absent lung sliding plus exclusive horizontal lines) in a particular location of the chest wall (arrow)
Lung ultrasound (LU) performed for question Q2. Nine additional cases of significant pleural effusion (PE) were diagnosed when LU was performed for questions other than Q2. Invasive interventions included chest tube placement in 7 cases (4 for hemothorax, 3 for empyema) and diagnostic thoracentesis and/or fluid drainage in 34 patients. a Complicated PE. b Abundant PE with floating lung. Tissue debris and diaphragms within pleura, the diaphragm, the consolidated lower lobe, PE, and floating lung are indicated by corresponding arrows
Lung ultrasound (LU) performed for question Q3. Sixteen additional cases of atelectasis were diagnosed when LU was performed for questions other than Q3. Seven out of 15 patients underwent therapeutic bronchoscopy. In eight patients, non-invasive therapy was applied (tight physiotherapy, changes in endotracheal tube position, and/or changes in bed position). a Right lower lobe atelectasis (black arrows), associated with small pleural effusion (white arrow). Note the presence of pleural fluid within the interlobular fissure (black arrow). The patient underwent successful bronchoscopy due to arterial blood gases derangement. b Left lower lobe atelectasis in another patient. Note the air bronchogram (punctiform or linear hyperechoic artifacts) within consolidation (arrows)
Lung ultrasound (LU) performed for question Q4. Nine additional cases of pneumonia were diagnosed when LU was performed for questions other than Q4. Invasive interventions included bronchoscopy with directed bronchoalveolar lavage (BAL) sampling and antibiotic modification (1 patient) and diagnostic thoracentesis for parapneumonic effusion evaluation (1 patient). Non-invasive interventions consisted of modification (step-up) or initiation of antibiotics. a Pneumonia with irregular boundaries and air bronchogram (black arrows) in right upper field. b Necrotic pneumonia with diaphragms and tissue within pleura (white arrow)
Lung ultrasound (LU) performed for question Q5. Twelve additional cases of diffuse pulmonary edema were diagnosed when LU was performed for questions other than Q5 (all from QABG group). Changes in medical treatment, consisting of higher PEEP application and aggressive diuretic therapy, were performed in seven patients with pulmonary edema due to congestive heart failure. Continuous venous–venous hemofiltration (CVVH) was applied in three patients with ultrasound findings of lung congestion, due to overload. PEEP was titrated at higher levels in four patients with acute respiratory distress syndrome (ARDS)/white lung and was decreased in one patient with ultrasound findings of overdistension at non-dependent lung zones, and massive atelectasis at dependent zones, due to abdominal compartment syndrome. The latter patient underwent successful abdominal decompression by colonoscopy. a, b LU findings in two patients suffering from severe ARDS. Note the white lung pattern—completely white echographic lung fields, with coalescent B lines and no horizontal reverberation (white arrows). Black arrows show the pleural line
Lung ultrasound (LU) performed for QABG. LU provided critical information about the clinical status in 43 patients, and resulted in change in patient management. Note that in 65 out of 108 examinations, the main finding was bilateral posterolateral consolidation associated with pleural effusion. a Bilateral posterolateral consolidation (black arrows) associated with pleural effusion (PLAPS). Thick black arrow indicates the diaphragm. b Diffuse bilateral B lines—well-defined hyperechoic comet-tail artifacts, arising from pleural line and spreading up indefinitely, erasing A lines and moving with the lung sliding when lung sliding is present (white arrow), in a patient with severe acute respiratory distress syndrome (ARDS). In this patient, PEEP was increased to 20 cmH2O after LU
When LU was performed for QABG, pathologic findings were observed in all cases, with bilateral lower lobe consolidation, accompanied by pleural effusion, being the most common. In 43 cases (39.8 %), the LU findings were consistent with one of the five pathologic entities (as described above) and had an impact on patient management (Fig. 7).
Overall, the management was changed directly as a result of information provided by the LU operator in 119 cases (47 %) (Fig. 1). In 81 cases, the change in patient management involved invasive interventions (i.e., chest tube, bronchoscopy, diagnostic thoracentesis/fluid drainage, continuous venous–venous hemofiltration, abdominal decompression, tracheotomy), and in 38 cases, non-invasive (i.e., PEEP change/titration, recruitment maneuver, diuretics, physiotherapy, change in bed position, antibiotics initiation/change). In 53 cases (21 %), LU revealed findings which supported diagnoses not suspected by the primary physician. These included 7 cases of pneumothorax, 9 of significant pleural effusion, 9 of pneumonia, 16 of unilateral atelectasis (lobar or total), and 12 of diffuse interstitial syndrome (white lung).
In 7 out of 253 cases, the primary physician ordered a thoracic CT scan to assist the decision-making process. In all cases CT confirmed the LU findings. In three cases, a thoracic CT was performed because pulmonary embolism was suspected, in two for further investigation of ARDS, in one for multiloculated parapneumonic effusion, and one for multiple trauma and esophageal rupture. In none of these cases was a bedside chest X-ray ordered. No further action was applied as a result of CT findings.
Discussion
The main finding of this study was that in mechanically ventilated critically ill patients, LU has significant therapeutic impact by influencing the decision-making process, as indicated by the high NRI (85.6 %). The information provided by the LU study directly changed the management of these patients in 47 % of the reported cases. In the majority of the cases, the change in patient management involved invasive interventions. Furthermore, in one-fifth of the studies, LU revealed findings compatible with diagnoses not suspected by the primary physician.
In our study, we examined the value of LU in addressing predefined clinical problems. We chose this study design because we, and others, have shown that LU may be used as an alternative to CT in critically ill patients (the gold standard for lung imaging in these patients) in identifying specific common lung pathologies, such as atelectasis, interstitial syndrome, pneumothorax, pleural effusion, and pneumonia [1, 2, 22]. For this reason, LU was performed when the primary physician suspected one of these pathologies. In addition, since these pathologies may lead to inefficient gas exchange, unexplained deterioration of arterial blood gases (unexplained persistent hypoxemia and/or hypercapnia) was also a reason for requesting LU study. An omission of this study design is that it does not permit an examination of the value of routine performance of LU in critically ill patients.
LU was performed by a single operator (NX) with extensive experience of this imaging technique. Although LU can be performed by almost all attending physicians in our unit, we decided, for the purpose of a uniform interpretation of the findings, to involve a single operator in our LU studies. This should also minimize the influence of the variability of operator bias on the results, as the operator simply presented the findings to the primary physician and was not responsible for further patient management. However, the results of this study may not be applicable when LU is performed by less experienced operators.
In all but one LU study, pathologic findings were observed. In the majority of the cases, these findings were compatible with consolidation, pleural effusion, and interstitial syndrome. This observation has been reported previously and reflects the critically ill population we studied [3]. The fact that almost all mechanically ventilated critically ill patients had pathologic findings in LU indicates that performing this imaging technique unselectively in these patients may not be helpful when planning the patients’ management. On the other hand, as our study has shown, ordering an LU examination on the basis of specific clinical problems may have a great impact on clinical decision making.
In several cases (42.7 %) LU study was ordered for unexplained deterioration of gas exchange. This was not an unexpected finding. Mechanically ventilated patients very often exhibit derangement in gas exchange for several reasons related to pulmonary and extrapulmonary factors. In these patients acute hypoxia and/or hypercapnia may be due to increased V′/Q′ inequalities, right to left shunt, and hypoventilation. It has been shown that LU can be used to diagnose most of the pathologic entities that can cause acute impairment in gas exchange, such as atelectasis, pneumothorax, and interstitial syndrome [2]. Therefore it is not surprising that in almost half of the cases LU was ordered for unexplained deterioration of gas exchange. Although in all cases LU revealed findings that could explain the blood gas abnormalities, in 38.9 % of cases the findings were compatible with a specific predefined diagnosis and appropriate action was taken.
In the majority of cases (57.3 %), LU was performed for a suspected specific pathology. We should mention that in almost 50 % of these cases, LU was performed because pneumothorax was suspected. This high percentage is most likely due to the specific population studied and to the study’s design. Several of our patients suffered from multiple trauma and/or ARDS necessitating the application of high PEEP. These patients have increased risk of pneumothorax, and in several cases, this forced the primary physician to order an LU study to address the issue of pneumothorax. The suspicion of pneumothorax was confirmed only in 28 out of 60 cases (46.7 %). It is of interest to note that when LU was performed for deterioration of arterial blood gases, an additional seven cases of non-suspected pneumothoraces were diagnosed. This emphasizes the value of LU in the investigation of acute impairments of ABGs.
Previous studies have also supported the value of LU in the diagnosis of respiratory system diseases and, indirectly, on the patients’ management. Yu et al. [22], in a small population of patients (n = 41), 19 of whom were managed in an ICU, performed LU when portable radiographs were difficult to interpret and showed that this technique was helpful in diagnosis (in 66 % of cases) and treatment planning (in 41 % of patients). Lichtenstein and Meziere [3], in an observational study, performed LU on consecutive patients admitted to the ICU with acute respiratory failure. These authors compared the LU results on initial presentation with the final diagnosis by the ICU team and demonstrated that LU findings immediately provided diagnosis of acute respiratory failure in 90.5 % of cases. Our study showed that in a large population of mechanically ventilated critically ill patients, whose clinical status necessitated a diagnostic procedure and therapeutic intervention, LU information provided to the primary physician changed the patients’ management in almost half of the cases. Furthermore, in one-fifth of the studies, LU revealed findings compatible with specific diagnoses not suspected by the primary physician. It follows that in the process of addressing specific questions, the LU has significant impact on decision making. To our knowledge, this is the first prospective study that clearly demonstrates the value of LU in the therapeutic management of ICU patients receiving mechanical ventilation.
The aim of this prospective study was to examine the impact of LU on decision making and therapeutic management. Neither the decision-making process nor the therapeutic management was controlled. The primary physician was fully responsible for the patients’ management. Since LU findings were present in several primary physicians and there were no predefined, protocol-driven management guidelines, the patients were not followed prospectively to examine if the changes in their management due to LU findings were appropriate or successful. However, in several cases, the change in patient management was obviously appropriate, particularly when the change involved invasive interventions (i.e., chest tube insertion for pneumothorax. See also Electronic Supplementary Material for comments on the appropriateness of therapeutic interventions). A study of different design may examine the influence of LU on the outcome of patients.
This study follows a previous one from the same department which showed that in an unselected general ICU population, LU, compared to chest X-ray, has a high diagnostic performance for the diagnosis of common pathologic conditions and may be used as an alternative to thoracic CT [2]. As a result, chest X-rays are not performed on a routine daily basis in our unit. It is likely that the impact of LU on decision making in this study was influenced by the results of our previous study (because LU operations were performed by the same operator) causing the primary physicians to rely on the LU findings to support their decision-making processes. We believe that this represents a major limitation of the study and may make it difficult to replicate in other ICUs.
In conclusion, our study has shown that in mechanically ventilated critically ill patients, in the process of addressing specific clinical questions, LU has had a significant impact on decision making. Notwithstanding its limitations (i.e., operator dependence), LU is a powerful, non-invasive diagnostic tool in critically ill patients.
References
Lichtenstein D, Goldstein I, Mourgeon E, Cluzel P, Grenier P, Rouby JJ (2004) Comparative diagnostic performances of auscultation, chest radiography, and lung ultrasonography in acute respiratory distress syndrome. Anesthesiology 100:9–15
Xirouchaki N, Magkanas E, Vaporidi K, Kondili E, Plataki M, Patrianakos A, Akoumianaki E, Georgopoulos D (2011) Lung ultrasound in critically ill patients: comparison with bedside chest radiography. Intensive Care Med 37:1488–1493
Lichtenstein DA, Meziere GA (2008) Relevance of lung ultrasound in the diagnosis of acute respiratory failure: the BLUE protocol. Chest 134:117–125
Bouhemad B, Liu ZH, Arbelot C, Zhang M, Ferarri F, Le-Guen M, Girard M, Lu Q, Rouby JJ (2010) Ultrasound assessment of antibiotic-induced pulmonary reaeration in ventilator-associated pneumonia. Crit Care Med 38:84–92
Blaivas M (2012) Lung ultrasound in evaluation of pneumonia. J Ultrasound Med 31:823–826
Lichtenstein DA (2009) Ultrasound examination of the lungs in the intensive care unit. Pediatr Crit Care Med 10:693–698
Bouhemad B, Zhang M, Lu Q, Rouby JJ (2007) Clinical review: bedside lung ultrasound in critical care practice. Crit Care 11:205
Volpicelli G, Elbarbary M, Blaivas M, Lichtenstein DA, Mathis G, Kirkpatrick AW, Melniker L, Gargani L, Noble VE, Via G, Dean A, Tsung JW, Soldati G, Copetti R, Bouhemad B, Reissig A, Agricola E, Rouby JJ, Arbelot C, Liteplo A, Sargsyan A, Silva F, Hoppmann R, Breitkreutz R, Seibel A, Neri L, Storti E, Petrovic T (2012) International evidence-based recommendations for point-of-care lung ultrasound. Intensive Care Med 38:577–591
Lichtenstein DA, Meziere G, Lascols N, Biderman P, Courret JP, Gepner A, Goldstein I, Tenoudji-Cohen M (2005) Ultrasound diagnosis of occult pneumothorax. Crit Care Med 33:1231–1238
Volpicelli G (2011) Sonographic diagnosis of pneumothorax. Intensive Care Med 37(2):224–232
Lichtenstein D, Meziere G, Biderman P, Gepner A (2000) The “lung point”: an ultrasound sign specific to pneumothorax. Intensive Care Med 26:1434–1440
Maslove DM, Chen BT, Wang H, Kuschner WG (2012) The diagnosis and management of pleural effusions in the ICU. J Intensive Care Med 28:24–36
Lichtenstein DA, Lascols N, Meziere G, Gepner A (2004) Ultrasound diagnosis of alveolar consolidation in the critically ill. Intensive Care Med 30:276–281
Lichtenstein D (2005) Ultrasound diagnosis of atelectasis. Int J Intensive Care 12:88–93
Lichtenstein DA, Lascols N, Prin S, Meziere G (2003) The “lung pulse”: an early ultrasound sign of complete atelectasis. Intensive Care Med 29:2187–2192
Lichtenstein D, Meziere G, Seitz J (2009) The dynamic air bronchogram. A lung ultrasound sign of alveolar consolidation ruling out atelectasis. Chest 135:1421–1425
Lichtenstein D, Meziere G, Biderman P, Gepner A, Barre O (1997) The comet-tail artifact. An ultrasound sign of alveolar-interstitial syndrome. Am J Respir Crit Care Med 156:1640–1646
Mallamaci F, Benedetto FA, Tripepi R, Rastelli S, Castellino P, Tripepi G, Picano E, Zoccali C (2010) Detection of pulmonary congestion by chest ultrasound in dialysis patients. JACC Cardiovasc Imaging 3:586–594
Lichtenstein D (2012) Fluid administration limited by lung sonography: the place of lung ultrasound in assessment of acute circulatory failure (the FALLS-protocol). Expert Rev Respir Med 6:155–162
Pencina MJ, D’Agostino RB, Vasan RS (2010) Statistical methods for assessment of added usefulness of new biomarkers. Clin Chem Lab Med 48:1703–1711
Steyerberg EW, Vickers AJ, Cook NR, Gerds T, Gonen M, Obuchowski N, Pencina MJ, Kattan MW (2010) Assessing the performance of prediction models: a framework for traditional and novel measures. Epidemiology 21:128–138
Yu CJ, Yang PC, Chang DB, Luh KT (1992) Diagnostic and therapeutic use of chest sonography: value in critically ill patients. AJR Am J Roentgenol 159:695–701
Acknowledgments
The authors would like to acknowledge G. Chlouverakis, Associate Professor of Biostatistics, for his contribution to the statistical analysis.
Conflicts of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Take-home message: In mechanically ventilated critically ill patients lung ultrasound has a significant impact on clinical decision making and therapeutic management.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Xirouchaki, N., Kondili, E., Prinianakis, G. et al. Impact of lung ultrasound on clinical decision making in critically ill patients. Intensive Care Med 40, 57–65 (2014). https://doi.org/10.1007/s00134-013-3133-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-013-3133-3