Abstract
Purpose
There is increasing evidence that critical illness and treatment in an intensive care unit (ICU) may result in significant long-term morbidity. The purpose of this systematic review was to summarize the current literature on long-term cognitive impairment in ICU survivors.
Methods
PubMed/MEDLINE, CINAHL, Cochrane Library, PsycINFO and Embase were searched from January 1980 until July 2012 for relevant articles evaluating cognitive functioning after ICU admission. Publications with an adult population and a follow-up duration of at least 2 months were eligible for inclusion in the review. Studies in cardiac surgery patients or subjects with brain injury or cardiac arrest prior to ICU admission were excluded. The main outcome measure was cognitive functioning.
Results
The search strategy identified 1,128 unique studies, of which 19 met the selection criteria and were included. Only one article compared neuropsychological test performance before and after ICU admission. The 19 studies that were selected reported a wide range of cognitive impairment in 4–62 % of the patients after a follow-up of 2–156 months.
Conclusion
The results of most studies of the studies reviewed suggest that critical illness and ICU treatment are associated with long-term cognitive impairment. Due to the complexity of defining cognitive impairment, it is difficult to standardize definitions and to reach consensus on how to categorize neurocognitive dysfunction. Therefore, the magnitude of the problem is uncertain.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The utilization of intensive care units (ICUs) has expanded rapidly over the past decades, with a concomitant increase in the proportion of patients surviving an episode of critical illness. This has resulted in a growing number of ICU survivors [1]. Results from previous studies suggest that ICU survivors may suffer from significant long-term morbidity [2]. An important long-term complication of critical illness and ICU treatment is cognitive impairment. Cognitive impairment is associated with a reduced quality of life, and it is a major determinant of societal healthcare costs and caregiving needs [3–5]. A large proportion of ICU patients consist of elderly people, and especially this population is prone to develop cognitive impairment [6]. However, it appears that younger, relatively healthy patients are also at risk for cognitive impairment following critical illness. Cognitive impairment often becomes apparent after ICU discharge, and intensivists may therefore not be aware of the occurrence of this complication. In the last 2 years, a number of high-quality studies on this topic have been published [1, 5]. The aim of this systematic review was to summarize current evidence for long-term cognitive impairment in ICU survivors.
Methods
This systematic review was performed in accordance with the recent standards for systematic reviews published by the Institute of Medicine in March 2011 [7].
Search strategy
We conducted a search of PubMed/MEDLINE, CINAHL, Cochrane Library, PsycINFO and Embase from January 1980 through July 2012 using relevant search terms relating to cognition and ICU admission. The exact search strategy is described in Table 1. The reference lists from the selected articles were screened to identify additional articles. To assess the comprehensiveness of the search strategy, we tested the search-string with eight studies that we already had on file and which we considered relevant for this systematic review.
Study selection
Studies on cognitive functioning after ICU admission in adults as the primary or secondary endpoint were included in our review. The following studies/articles were excluded:
-
reviews, case studies and animal studies, as well as articles published in languages other than English, Dutch, German or French;
-
investigations with a follow-up duration on cognitive functioning shorter than 2 months;
-
studies on patients undergoing heart surgery and on those with cardiac arrest or brain injury prior to ICU admission;
-
articles describing the same or an overlapping patient sample as that described in an article already included in the review; in this case, we only used the most recent article, which described both the new data and the data reported earlier.
The eligibility of each article that was found was independently evaluated on title, abstract and, if necessary, full text, by two reviewers using the above-mentioned selection criteria (AEW and AWvdK). If the two reviewers disagreed about the eligibility of an article, a third reviewer (AJCS) was consulted.
Data extraction
Both reviewers independently assessed the articles that were selected using a standardized data collection form to record the required data [Electronic Supplementary Material (ESM) 1]. The following characteristics were recorded: first author, year of publication, study design, study population with in- and exclusion criteria, number of enrolled participants and age at baseline, number of deceased subjects and loss-to-follow-up, measurement of baseline cognition and the neuropsychological tests used and the test results. Study quality was assessed based on four criteria: (1) availability of data on cognitive functioning at baseline; (2) use of neuropsychological tests to assess cognition; (3) description of inclusion and exclusion criteria; (4) adjustment for predictors which could interfere with the cognitive outcome, such as age and gender. These quality criteria were chosen because these are universally applicable (item 3 and 4) and specific for studies evaluating neurocognitive outcome (criteria 1 and 2).
Statistical analysis
The data of the included studies were not pooled because we expected considerable methodological differences between studies, especially with respect to the selection of neuropsychological tests, timing of assessment and definitions of cognitive impairment.
Some authors hypothesize that the risk of neurocognitive impairment is higher in patients with acute respiratory distress syndrome (ARDS) than in the general ICU population [4, 8]. Elderly ICU patients may also have an increased risk of cognitive impairment [6]. In the presentation of the selected studies, we therefore, distinguished studies with focus on ARDS and studies with focus on elderly patients. The other three ICU-population categories were: surgical, medical and general.
Results
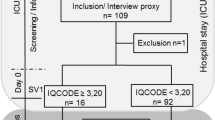
The search-string (Table 1) yielded a total of 1,664 publications, of which 1,128 were unique. The defined search strategy did identify all eight studies that we already had on file and which we considered relevant for this systematic review. We excluded 1,094 articles based on title or abstract and evaluated 34 full-text articles (Fig. 1). There was disagreement on the eligibility of one article between the first two reviewers [5]. The study was of a high quality, especially because of the presence of baseline neuropsychological data, but the patient cohort did not exclusively comprise an ICU population. In consultation with the third reviewer, consensus was reached to exclude this study from the systematic review but to mention its results in the Discussion. Eventually, 19 articles met the selection criteria and were included. No extra titles were identified after screening the reference lists.
The included studies are shown in Tables 2 and 3. Table 2 summarizes the data of the 14 studies which extensively used neuropsychological testing to measure cognitive functioning, and Table 3 outlines five additional studies which used questionnaires or screening test data to assess cognitive performance. The number of subjects per study varied between 30 and 1,822. Most studies consisted of young, relatively healthy ICU survivors. Eleven studies had a study population with a mean age of 54 years or less. Four studies focused on the elderly or very elderly (>65, >75 and >80 years, respectively) [1, 9–11]. The patient populations of seven comprised ARDS patients. The studies had a follow-up duration varying from 2 months up to 13 years after ICU discharge.
Only one of the 19 articles met all four quality criteria, with the inclusion of a neuropsychological assessment prior to ICU admission [1]. Seven other investigations took an estimated premorbid cognitive functioning into account [8, 10–15]. Fourteen studies met the second quality criterion, which was the use of neuropsychological testing to assess cognitive functioning (Table 2) [1, 8, 12–23]. All 19 articles reported in- and exclusion criteria. The fourth quality criterion, i.e. adjustment for predictors (co-variables) which could interfere with the cognitive outcome, was met by 16 studies which compared the post-ICU test performance to normative age- and gender-matched population data [1, 8, 11–24]. One study used age- and gender-matched data from a population with long-standing illness for comparison [3]. In some studies a correction was made for educational level [8, 11–15, 17–19], 11 studies made an adjustment for severity of illness during ICU admission [8, 9, 12–17, 21, 23, 24] and nine studies took the length of ICU admission into account [3, 9, 12, 15, 16, 19, 21, 23, 24].
Of the 19 articles reviewed, four reported a relatively good cognitive status amongst ICU survivors, which was defined as ≤10 % of patients with cognitive impairment [10, 16, 22] or a p value of >0.05 [11]. Absence of cognitive impairment was reported more often in studies with screening tests (2/5, 40 %; Table 3) than in investigations based on neuropsychological tests (2/13, 15 %; Table 2). In addition, in one of the studies which used neuropsychological tests half of the patients (N = 27) were excluded because they could not complete the cognitive testing [16]; if all these 27 patients had cognitive impairments, the rate of impairment would have been close to 100 %. The other 15 studies reported at least “mild” cognitive impairment in a larger proportion of ICU survivors. The studies with the screening test data reported impairment in 11–56 % of the population [3, 9, 24]. The investigations with neuropsychological testing showed impairment in 11–62 % of the examined population [1, 8, 12–15, 17–21]. Although the range of cognitive impairment was comparable, in general the studies with extensive neuropsychological testing reported a higher incidence of cognitive impairment than those with screening test data.
The incidence of cognitive impairment of ARDS survivors ranged from 4 to 56 % [8, 12, 15, 19, 22–24]. Within the general, medical and surgical ICU survivors the incidence of cognitive impairment ranged from 4 to 62 % [3, 13, 14, 16–18, 21]. Four studies assessed cognitive impairment in the elderly [1, 9–11], two of which, both based on screening test data, did not find significant cognitive impairment among their elderly subjects [10, 11]. The other two studies in elderly patients reported cognitive impairment varying from 17 to 56 % [1, 9].
The tested cognitive domains per article are shown in Table 4. Of the included studies, 14 tested for ‘memory,’ which was therefore the most tested domain. The domains of memory, attention, verbal fluency and executive functioning were most frequently impaired [12, 18–21, 24]. Two studies reported an association between a higher estimated premorbid IQ and less cognitive impairment [8, 13].
Seven studies measured cognitive functioning at multiple points in time after ICU admission [8, 12, 17, 21, 23, 24]. However, one study only reported the proportion of patients with cognitive impairment at the final assessment [23]. Two studies found no improvement of cognitive function during 1 to 2 years of follow-up [8, 12]. One article reported no improvement, even after 5 years of follow-up [24]. However, another study reported a return towards normal cognitive functioning by 9 months [21], and one study reported a decrease in severe impairment after 1 year [17].
Discussion
In this review, we systematically assessed publications on cognitive impairment after admission to a general ICU. The 19 studies that met the selection criteria reported a wide range of cognitive impairment in 4–62 % of the patients after a follow-up of 2–156 months. Compared to studies which used neuropsychological testing, lower percentages of patients with cognitive impairment were reported in studies which only used screening test data. We found no difference in the risk of cognitive impairment between studies involving only ARDS patients and those which also included other ICU patients. In addition, we did not find a higher risk of cognitive impairment in studies in elderly patients, although three of the studies assessed only used screening test data.
The pathophysiology of cognitive impairment after ICU admission is believed to be multifactorial [13, 21]. The most frequently reported explanation for an abrupt decrease in cognitive functioning after ICU admission is that patients with multi-organ failure may also develop brain damage [13, 25]. Severe sepsis can lead to a neuro-inflammatory response, resulting in increased levels of cytokines in the brain [25, 26]. Elevated cytokine levels are associated with impaired memory in healthy volunteers [27], and neuro-inflammation is associated with the development of Alzheimer’s disease [28]. Long-term cognitive impairment in patients may therefore represent a maladaptive version of cytokine-induced disease [26]. Other possible causes are hypoxemia and hypotension, which have been related to cognitive impairment in numerous investigations [12, 13]. Sedatives and analgesics are used extensively in the ICU, and some studies suggest that this may also play a causal role in the development of long-term cognitive impairment [13]. Both hyperglycemia and hypoglycaemia as well as fluctuations in blood glucose are also associated with poor cognitive outcomes [18, 29]. An association between delirium and long-term cognitive impairment has been reported, but the underlying cause remains to be elucidated [17, 30].
The focus of this review was on long-term cognitive impairment. We excluded those studies with a follow-up duration of less than 2 months. An early cognitive assessment may reflect residual pain, the effects of analgesic and sedative drugs and/or residual delirium [12, 16]. The results of studies that measured cognition immediately after ICU admission and also at various time points during a long-term follow-up indicate that the incidence of cognitive impairment is high after ICU discharge but improves during the first few months after discharge [12].
Even with the use of strict selection criteria, it was difficult to compare the reviewed studies and, therefore, it was impossible to present pooled data. Among the reviewed studies which reported the results of neuropsychological testing, there was a substantial variation in the definition of impairment, sample size and timing of assessment. In addition, medical practices in the ICU have substantially changed during the past decade, and these practical changes may also affect cognitive outcomes. However, we were unable to observe such an effect over time because all studies included in this review were published in the last 10 years.
A major limitation of most of the studies reviewed is that a baseline assessment of cognitive status before ICU admission is lacking. Ideally, cognition should be measured before and after ICU admission because the real interest is not the absolute level of cognitive performance but rather the change in cognitive functioning. ICU admissions, however, are often not elective and, consequently, a baseline assessment is usually not available. Some studies estimated the baseline cognitive performance after ICU admission rather than testing it in advance. Adjustments were made for patients who showed signs of pre-existing cognitive impairment [8, 12–15]. Remarkably, there are two recent population-based studies with premorbid cognitive data [1, 5]. The first is a population-based longitudinal study of aging and dementia, designed to establish the incidence of both cognitive impairment and risk factors for cognitive decline [1]. Of the 2,929 subjects who underwent repeated neuropsychological testing, 41 were admitted to an ICU. The authors of this study concluded that those who were hospitalized for a critical illness had a greater likelihood of cognitive impairment, even after adjusting for premorbid cognitive screening scores and comorbidity. The rate of cognitive decline did not change after admission to the ICU compared with the normal rate of decline. Therefore, the authors suggested that critical illness may cause an abrupt loss of cognitive function rather than accelerate the decline in cognitive functioning [1]. The second study with premorbid cognitive data was conducted among patients who survived severe sepsis [5]. Baseline cognitive assessments were performed in 9,223 respondents, of whom 516 survived severe sepsis. This study was not included in the Results of this review because the study did not require that patients be treated in an ICU. Consultation with the authors of this study revealed that 43 % of the sepsis survivors were admitted to the ICU but that no subanalysis data on the ICU patients were available. The authors measured an increase from moderate to severe cognitive impairment among sepsis survivors. Before sepsis, 6.1 % of the eventual survivors showed moderate to severe cognitive impairment [5]; after severe sepsis, the prevalence increased to 16.7 %. These results led the authors to conclude that severe sepsis was independently associated with new cognitive impairment, which appeared to be substantial and persistent [5]. In the subgroup of the ICU patients, the risk of cognitive impairment was comparable to that of the whole study population (TJ Iwashyna, personal communication).
The effects of severity of illness on the risk for developing long-term cognitive impairment remain uncertain. Due to the small size of the patient groups, the availability of analyses in patient subgroups is limited. It is even more relevant to evaluate the effect of interventions that may reduce the risk of cognitive impairment. A possible intervention that could be evaluated in a randomized study is early mobilization [31]. Early mobilization has a positive effect on length of stay in the ICU and on physical independence after discharge [31, 32]; it also reduces depression in survivors of critical illness [32].
It remains uncertain whether a low performance on neuropsychological tests reflects an impairment in cognitive functioning related to critical illness and ICU admission, or whether it is perhaps merely a marker of patients with poor health and an increased risk of ICU admission. However, the two studies with premorbid cognitive data show that at least part of the measured cognitive impairment is related to the ICU admission and critical illness [1, 5]. There are similarities between recent studies on cognitive impairment after critical illness and ICU treatment and the slightly older studies on cognitive impairment after cardiac surgery [33–35]. It has become apparent in the field of cardiac surgery that it is extremely difficult to distinguish normal variation in test performance from true cognitive impairment [36, 37]. Consequently, in cardiac surgery, it is now accepted that the incidence of cognitive injury has long been overestimated because normal variations in test performance were formerly not always recognized [35, 38, 39]. However, cardiac surgical patients clearly differ from general ICU patients, and a comparison with the post-cardiac surgery literature might therefore be misleading. Additional research is still required to establish a reliable incidence of cognitive decline following ICU admission.
In conclusion, most of the studies reviewed here suggest that critical illness and ICU treatment are associated with long-term cognitive impairment. Due to the complexity of defining cognitive impairment, both the magnitude and severity of the problem are uncertain. It is therefore crucial that the definition of neurocognitive dysfunction is standardized. The pathophysiology of cognitive impairment after ICU admission is believed to be multi-factorial, and more research is needed to identify key risk factors. Previously identified risk factors for neurocognitive dysfunction are severity of illness, hypoxemia, hypotension, the use of sedatives and analgesics, hyper- and hypoglycaemia and the presence of a delirium. The aim of future studies should be to adjust for cognitive functioning before ICU admission, psychological co-morbidities and other possible confounders. Eventually these investigations may lead to improved long-term outcome after ICU admission.
References
Ehlenbach WJ, Hough CL, Crane PK, Haneuse SJ, Carson SS, Curtis JR, Larson EB (2010) Association between acute care and critical illness hospitalization and cognitive function in older adults. JAMA 303(8):763–770. doi:10.1001/jama.2010.167
Desai SV, Law TJ, Needham DM (2011) Long-term complications of critical care. Crit Care Med 39(2):371–379. doi:10.1097/CCM.0b013e3181fd66e5
Timmers TK, Verhofstad MHJ, Moons KGM, Van Beeck EF, Leenen LPH (2011) Long-term quality of life after surgical intensive care admission. Arch Surg 146(4):412–418. doi:10.1001/archsurg.2010.279
Davidson TA, Caldwell ES, Curtis JR, Hudson LD, Steinberg KP (1999) Reduced quality of life in survivors of acute respiratory distress syndrome compared with critically ill control patients. JAMA 281(4):354–360. doi:10.1001/jama.281.4.354
Iwashyna TJ, Ely EW, Smith DM, Langa KM (2010) Long-term cognitive impairment and functional disability among survivors of severe sepsis. JAMA 304(16):1787–1794. doi:10.1001/jama.2010.1553
Boumendil A, Somme D, Garrouste-Orgeas M, Guidet B (2007) Should elderly patients be admitted to the intensive care unit? Intensive Care Med 33(7):1252–1262. doi:10.1007/s00134-007-0621-3
Board on Health Care Services (2011) Finding what works in health care, Standards for systematic reviews. Available at: www.iom.edu/srstandards. Accessed 1 Feb 2012
Larson MJ, Weaver LK, Hopkins RO (2007) Cognitive sequelae in acute respiratory distress syndrome patients with and without recall of the intensive care unit. J Int Neuropsychol Soc 13(4):595–605. doi:10.1017/S1355617707070749
de Rooij SE, Govers AC, Korevaar JC, Giesbers AW, Levi M, de Jonge E (2008) Cognitive, functional, and quality-of-life outcomes of patients aged 80 and older who survived at least 1 year after planned or unplanned surgery or medical intensive care treatment. J Am Geriatr Soc 56(5):816–822. doi:10.1111/j.1532-5415.2008.01671.x
Sacanella E, Perez-Castejon JM, Nicolas JM, Masanes F, Navarro M, Castro P, Lopez-Soto A (2011) Functional status and quality of life 12 months after discharge from a medical ICU in healthy elderly patients: a prospective observational study. Crit Care 15(2):R105. doi:10.1186/cc10121
Daubin C, Chevalier S, Seguin A et al (2011) Predictors of mortality and short-term physical and cognitive dependence in critically ill persons 75 years and older: a prospective cohort study. Health Qual Life Outcomes 9:35. doi:10.1186/1477-7525-9-35
Hopkins RO, Weaver LK, Collingridge D, Parkinson RB, Chan KJ, Orme JF Jr (2005) Two-year cognitive, emotional, and quality-of-life outcomes in acute respiratory distress syndrome. Am J Respir Crit Care Med 171(4):340–347. doi:10.1164/rccm.200406-763OC
Jackson JC, Hart RP, Gordon SM, Shintani A, Truman B, May L, Ely EW (2003) Six-month neuropsychological outcome of medical intensive care unit patients. Crit Care Med 31(4):1226–1234. doi:10.1097/01.CCM.0000059996.30263.94
Jackson JC, Obremskey W, Bauer R, Greevy R, Cotton BA, Anderson V, Song Y, Ely EW (2007) Longterm cognitive, emotional, and functional outcomes in trauma intensive care unit survivors without intracranial hemorrhage. J Trauma 62(1):80–88. doi:10.1097/TA.0b013e31802ce9bd
Rothenhausler H-, Ehrentraut S, Stoll C, Schelling G, Kapfhammer HP (2001) The relationship between cognitive performance and employment and health status in long-term survivors of the acute respiratory distress syndrome: results of an exploratory study. Gen Hosp Psychiatry 23(2):90–96. doi:10.1016/S0163-8343(01)00123-2
Torgersen J, Hole JF, Kvale R, Wentzel-Larsen T, Flaatten H (2011) Cognitive impairments after critical illness. Acta Anaesthesiol Scand 55(9):1044–1051. doi:10.1111/j.1399-6576.2011.02500.x
Girard TD, Jackson JC, Pandharipande PP, Pun BT, Thompson JL, Shintani AK, Gordon SM, Canonico AE, Dittus RS, Bernard GR, Ely EW (2010) Delirium as a predictor of long-term cognitive impairment in survivors of critical illness. Crit Care Med 38(7):1513–1520. doi:10.1097/CCM.0b013e3181e47be1
Duning T, van den Heuvel I, Dickmann A, Volkert T, Wempe C, Reinholz J, Lohmann H, Freise H, Ellger B (2010) Hypoglycemia aggravates critical illness-induced neurocognitive dysfunction. Diabetes Care 33(3):639–644. doi:10.2337/dc09-1740
Mikkelsen ME, Shull WH, Biester RC, Taichman DB, Lynch S, Demissie E, Hansen-Flaschen J, Christie JD (2009) Cognitive, mood and quality of life impairments in a select population of ARDS survivors. Respirology 14(1):76–82. doi:10.1111/j.1440-1843.2008.01419.x
Jones C, Griffiths RD, Slater T, Benjamin KS, Wilson S (2006) Significant cognitive dysfunction in nondelirious patients identified during and persisting following critical illness. Intensive Care Med 32(6):923–926. doi:10.1007/s00134-006-0112-y
Sukantarat KT, Burgess PW, Williamson RC, Brett SJ (2005) Prolonged cognitive dysfunction in survivors of critical illness. Anaesthesia 60(9):847–853. doi:10.1111/j.1365-2044.2005.04148.x
Kapfhammer HP, Rothenhausler HB, Krauseneck T, Stoll C, Schelling G (2004) Posttraumatic stress disorder and health-related quality of life in long-term survivors of acute respiratory distress syndrome. Am J Psychiatry 161(1):45–52. doi:10.1176/appi.ajp.161.1.45
Mikkelsen ME, Christie JD, Lanken PN et al (2012) The adult respiratory distress syndrome cognitive outcomes study: long-term neuropsychological function in survivors of acute lung injury. Am J Respir Crit Care Med 185(12):1307–1315. doi:10.1164/rccm.201111-2025OC
Adhikari NK, Tansey CM, McAndrews MP, Matté A, Pinto R, Cheung AM, Diaz-Granados N, Herridge MS (2011) Self-reported depressive symptoms ands memory complaints in survivors five years after ARDS. Chest 140(6):1484–1493. doi:10.1378/chest.11-1667
Hopkins RO, Weaver LK, Chan KJ, Orme JF Jr (2004) Quality of life, emotional, and cognitive function following acute respiratory distress syndrome. J Int Neuropsychol Soc 10(7):1005–1017. doi:10.1017/S135561770410711X
Dantzer R, O’Connor JC, Freund GG, Johnson RW, Kelley KW (2008) From inflammation to sickness and depression: when the immune system subjugates the brain. Nat Rev Neurosci 9(1):46–56. doi:10.1038/nrn2297
Reichenberg A, Yirmiya R, Schuld A, Kraus T, Haack M, Morag A, Pollmacher T (2001) Cytokine associated emotional and cognitive disturbances in humans. Arch Gen Psychiatry 58(5):445–452. doi:10.1001/archpsyc.58.5.445
Anastasio TJ (2011) Data-driven modeling of Alzheimer disease pathogenesis. J Theor Biol 290C:60–72. doi:10.1016/j.jtbi.2011.08.038
Hopkins RO, Key CW, Suchyta MR, Weaver LK, Orme JF Jr (2010) Risk factors for depression and anxiety in survivors of acute respiratory distress syndrome. Gen Hosp Psychiatry 32(2):147–155. doi:10.1016/j.genhosppsych.2009.11.003
van den Boogaard M, Schoonhoven L, Evers AW, van der Hoeven JG, van Achterberg T, Pickkers P (2012) Delirium in critically ill patients: impact on long-term health-related quality of life and cognitive functioning. Crit Care Med 40(1):112–118. doi:10.1097/CCM.0b013e31822e9fc9
Schweickert WD, Kress JP (2011) Implementing early mobilization interventions in mechanically ventilated patients in the ICU. Chest 140(6):1612–1617. doi:10.1378/chest.10-2829
Jones C, Skirrow P, Griffiths RD, Humphris GH, Ingleby S, Eddleston J, Waldmann C, Gager M (2003) Rehabilitation after critical illness: a randomized, controlled trial. Crit Care Med 31(10):2456–2461. doi:10.1097/01.CCM.0000089938.56725.33
van Dijk D, Keizer AM, Diephuis JC, Durand C, Vos LJ, Hijman R (2000) Neurocognitive dysfunction after coronary artery bypass surgery: a systematic review. J Thorac Cardiovasc Surg 120(4):632–639. doi:10.1067/mtc.2000.108901
Newman MF, Kirchner JL, Phillips-Bute B, Gaver V, Grocott H, Jones RH, Mark DB, Reves JG, Blumenthal JA (2001) Longitudinal assessment of neurocognitive function after coronary-artery bypass surgery. N Engl J Med 344(6):395. doi:10.1056/NEJM200102083440601
Selnes OA, Gottesman RF, Grega MA, Baumgartner WA, Zeger SL, McKhann GM (2012) Cognitive and neurologic outcomes after coronary-artery bypass surgery. N Engl J Med 366(3):250–257. doi:10.1056/NEJMra1100109
Keizer AM, Hijman R, Kalkman CJ, Kahn RS, Van Dijk D, Octopus Study Group (2005) The incidence of cognitive decline after (not) undergoing coronary artery bypass grafting: the impact of a controlled definition. Acta Anaesthesiol Scand 49(9):1232–1235. doi:10.1111/j.1399-6576.2005.00835.x
Selnes OA, Pham L, Zeger S, McKhann GM (2006) Defining cognitive change after CABG: decline versus normal variability. Ann Thorac Surg 82(2):388–390. doi:10.1016/j.athoracsur.2006.02.060
van Dijk D, Moons KG, Nathoe HM, van Aarnhem EH, Borst C, Keizer AM, Kalkman CJ, Hijman R, Octopus Study Group (2008) Cognitive outcomes five years after not undergoing coronary artery bypass graft surgery. Ann Thorac Surg 85(1):60–64. doi:10.1016/j.athoracsur.2007.08.068
Stroobant N, van Nooten G, De Bacquer D, Van Belleghem Y, Vingerhoets G (2008) Neuropsychological functioning 3–5 years after coronary artery bypass grafting: does the pump make a difference? Eur J Cardiothorac Surg 34(2):396–401. doi:10.1016/j.ejcts.2008.05.001
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is discussed in the editorial available at: doi:10.1007/s00134-012-2789-4.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Wolters, A.E., Slooter, A.J.C., van der Kooi, A.W. et al. Cognitive impairment after intensive care unit admission: a systematic review. Intensive Care Med 39, 376–386 (2013). https://doi.org/10.1007/s00134-012-2784-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-012-2784-9