Abstract
Purpose
Assessment of the cost utility (CU) of acute renal replacement therapy (RRT) from a societal perspective during a 5-year follow-up.
Methods
This was a cross-sectional cohort study in a medical-surgical intensive care unit and an acute RRT unit of 410 consecutive patients treated with acute RRT in Helsinki University Hospital in 2000–2002. Five-year survival and health-related quality of life (HRQoL) were assessed and used to calculate quality-adjusted life years (QALYs) in two ways. They were first calculated for the 5-year follow-up period and, second, estimated for the expected lifetime. HRQoL was assessed by the EuroQol (EQ-5D) in 2003. The cost analysis included hospital costs during index hospitalization along with hospital and societal costs for the following 5 years. The CU ratio was determined as total costs divided by gained QALYs.
Results
Median survival time for all patients was 0.20 years and the EQ-5D index score was 0.68, 0.18 lower than that of the age- and gender-matched general population. All RRT-treated patients gained 0.10 QALYs/patient and hospital survivors 2.54 QALYs in 5 years. Overall the CU ratio was poor [5 year median 271,116 (29,782–2,177,581) €/QALY]. However, it was acceptable (less than 50,000 €/QALY) in patients who survived for more than a year and did not need chronic RRT. Cost utility decreased with increasing age exceeding 1.0 million €/QALY in the older groups.
Conclusions
In general, the CU ratio of acute RRT is poor. However, it is acceptable in patients with renal recovery who survive for more than 1 year.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The incidence of acute kidney injury (AKI) varies from 8 to 19 cases/100,000 population [1–3] to as many as 500 cases/100,000 population [4]. The incidence of AKI seems to increase over time [5]. In hospitalized patients, the incidence of AKI is approximately 18 % [6] and in intensive care units (ICUs) from 5 to 25 % of the patients [3, 7–10], and a significant number of these need renal replacement therapy (RRT). Approximately 4–6 % of all critically ill patients receive RRT during their ICU stay [3, 10].
The mortality and morbidity rates for AKI patients are high. Recently, a large multicenter study with 24,000 patients reported the hospital mortality rate of RRT patients to be around 35 % in Finland [3]. Another multinational study with 29,269 critically ill patients has reported a hospital mortality rate of 60 % among patients with AKI [10]. Even a small acute decrease in kidney function increases the mortality rate significantly, and increasing disease severity increases the mortality rate considerably [11, 12]. Long-term mortality and morbidity are also increased [1, 13–18]. Surviving patients show a diverse quality of life (QoL) after RRT. Some studies have shown reduced QoL after RRT [14, 19–21], while some studies have reported no difference in long-term QoL between RRT and non-RRT patients [3, 22]. QoL in these studies is frequently reported as health-related quality of life (HRQoL), which covers three main aspects: physical, psychological and social aspects. In cost-effectiveness calculations HRQoL can be used to calculate gained quality-adjusted life years (QALYs) by multiplying the patient’s HRQoL with the life years gained.
The costs of care for AKI and RRT patients are high. Few studies [14, 23, 24] have evaluated the cost-effectiveness of treating patients with acute RRT. No study has included a societal perspective and a long follow-up with estimation of quality-adjusted life years (QALY) for the expected lifetime.
Accordingly, in this study we aimed to assess all medical and societal costs per one QALY in patients after acute RRT using a lifetime scale.
Methods
Patients
This study was a secondary analysis of a retrospective cohort of patients treated with acute RRT in 1998–2002. The study population has been described in detail previously [14]. Briefly, the original study population comprised 703 patients receiving acute RRT in Helsinki University Hospital in 1998–2002. The majority of the patients were treated in the ICUs (324 of 410, 79 %). The remaining 86 patients were treated in the acute dialysis unit; 97 % of the patients had AKI and 3 % received RRT for severe rhabdomyolysis. Patients who were dialyzed solely for intoxication were excluded. Due to changes in data, warehouse cost data on hospitalization costs could not be obtained for the years 1998–1999. Hence, patients treated after 2000 were included in the study.
Data collection
In 2010 the local ethics committee approved the study protocol and waived the need for further informed consent. Statistics Finland supplied mortality dates for patients in the beginning of 2010. The clinical patient-level costing and analyzer system (Ecomed, Datawell, Espoo, Finland) provided data of hospital costs for the index hospitalization and for subsequent hospital readmissions during the following 5 years. The Social Insurance Institution of Finland provided data of societal costs and costs for the patient. Demographic data were retrieved from hospital records.
HRQoL was assessed in 2003 by the validated Finnish version of EuroQol (EQ-5D) instrument, which includes five dimensions (mobility, self-care, usual activities, pain or discomfort, anxiety or depression) evaluated on a 1–3 scale [25]. It uses a set of population-based preference weights to calculate a single index score representing the overall HRQoL, which facilitates comparison with the age- and gender-matched general population. It also includes a visual analog scale (VAS) for self-rating of patients’ health.
Cost-utility calculations
Our analysis included direct and indirect hospital costs for the provider, societal costs for the provider (sickness allowances, new disability pensions, private medical examination and physician fees, and reimbursements for the cost of medication), and available costs for the patients (private medical examination and physician fees, and cost of medication) during the 5-year follow-up. Neither readmission hospital costs for hospital survivors living outside the capital area of Helsinki (18/210 patients) nor primary health care costs were available. Additional costs for the patient (some income losses, cost of home care, etc.) were not available.
Total costs for index hospitalization and for subsequent readmissions to hospitals in the Helsinki area during the next 5 years were obtained individually for each patient from the year 2000 on. Indirect hospitalization costs (for example, hospital management and maintenance costs) were included in the total costs. Direct medical costs concerning long-term RRT during the 5-year follow-up period were obtained from the hospital costing system. Direct costs concerning acute RRT during index hospitalization were either obtained from hospital billing records (intermittent RRT) or calculated separately (continuous RRT) and have been reported earlier.
We calculated gained QALYs in two ways. For the 5-year follow-up period we multiplied the EQ-5D index score in 2003 by the 5-year survival time with an assumption that the EQ-5D represented the follow-up period. The HRQoL of patients who perished before 2003 or did not return the HRQoL questionnaire was assumed to be lower than that of the respondents. For those patients the median EQ-5D index score of the respondents was multiplied by 0.75 to calculate QALYs. For the lifetime scale calculation, we estimated the remaining life years for the surviving patients using the predicted life expectancy for the age- and gender-matched Finnish population in 2007. We estimated that the QOL does not remain constant throughout the patient's lifetime and therefore subtracted an annual discount of 3 % from the measured EQ-5D index from the year 2004 on, as has been previously recommended [15]. Predicted lifetime QALYs were then calculated as a sum of yearly QALYs. Finally, we calculated CU as total costs per gained QALYs. We did not use any discount for costs after the 5-year follow-up.
Statistical analysis
Hospital, 1- and 5-year mortality rates were calculated. Cost per patient and cost per QALY according to survival time, age group, severity of disease and the need for chronic RRT were compared by the Mann-Whitney U-test and Kruskal-Wallis test. The sensitivity of the CU ratio was assessed by univariate analyses, first by excluding groups of patients: (1) all patients over 65 years old (n = 170), (2) all patients with chronic renal disease before hospitalization (n = 50), (3) all patients treated in the intensive care unit (n = 324), (5) all patients treated in the hospital wards (n = 86), and (6) all patients with Acute Physiology And Chronic Health Evaluation (APACHE) II scores over 20 (n = 92). Second, the costs after hospital discharge were increased by 50 % to consider those medical downstream costs that were not available. Finally, we conducted three subanalyses: one including only ICU patients, another on hospital survivors with renal recovery, and a third one including only those patients, who returned the EQ-5D questionnaire. A p value of 0.05 or less was considered significant except in multiple comparisons where a p value of 0.012–0.017 or less was considered significant according to Bonferroni’s correction. The results are presented as medians and interquartile ranges (IQR). Statistical analysis was performed using the Statistical Package for the Social Sciences (SPSS), version 19.0 for Windows (SPSS, Chicago, IL, USA).
Results
Patients
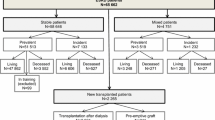
All 410 patients from 2000–2002 were included in the analysis (Fig. 1); 269 patients (66 %) were initially treated with intermittent RRT, 63 patients (15 %) with continuous RRT (CRRT) and 78 patients (19 %) with both. One patient needed chronic RRT before hospitalization, but was included in the study because he required acute RRT for severe rhabdomyolysis. Demographic data for the study population are presented in Table 1.
Mortality and renal recovery
Of 410 patients, 200 (49 %) died in the hospital, 235 (57 %) in 1 year and 271 (66 %) in 5 years. Median (IQR) survival time for all patients was 0.20 (0.02–5.00) years [74 (8–1,825) days]. During the 5 years after initial hospital treatment, 21 of 210 (10 %) hospital survivors needed chronic RRT. Thirteen of them were treated with chronic intermittent hemodialysis, five with peritoneal dialysis and two with both modalities. In five patients, the modality of chronic RRT could not be retrieved from the hospital records. Five patients (2 % of 210) received a renal transplant.
Costs
Median total costs during the 5-year follow-up were 40,923 (17,591–89,306) € per patient, 30,699 (15,091–71,818) € for patients treated in the hospital wards, 43,359 (19,411–91,896) € for patients treated in the ICU and 64,285 (31,428–113,266) € per hospital survivor. Cost for the index hospitalization was 28,527 (11,317–60,879) € per patient, 11,588 (7,335–23, 065) € for patients treated in the hospital wards and 34,063 (15,170–66,665) € for patients treated in the ICU. It did not significantly differ between hospital survivors [30,040 (12,888–67,222) €] versus non-survivors [27,293 (10,607–56,672) €; p = 0.180]. Societal costs and hospital costs after initial hospital treatment among all hospital survivors during the next 5 years were 19,168 (5,803–46,593) €. Total costs of chronic RRT for those 21 patients needing it were 25,802 (11,500–111,257) € during the 5-year follow-up. These patients received a median of 93 (50–427) renal replacement treatments. Distribution of costs is presented in Table 2.
Quality of life
We received HRQoL from 107 of 152 patients (70.4 % of possible respondents) in 2003. Five-year gained QALYs for these 107 patients were 3.38 (2.38–4.01). The median EQ-5D index score of the respondents was 0.68 (0.53–0.85), 0.18 lower than that of the age- and gender-matched general population. The QOL in patient subgroups is presented in Table 3.
Cost utility
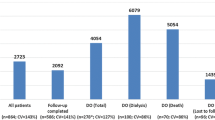
The 5-year total costs per 5-year QALYs were 22,796 (13,719–43,161) €/QALY for those 107 patients whose HRQoL was attained in 2003. The estimated lifetime CU in these patients was 7,918 (4,083–19,547) €/QALY. For all RRT patients 5-year total costs per 5-year QALYs were 271,116 (29,782–2,177,581) €/QALY. Cost utility of acute RRT depending on survival time, age of the patient, severity of disease, RRT modality and chronic renal disease before or after hospitalization is presented in Table 4. CU was significantly better for hospital survivors with renal recovery than for patients who needed chronic RRT afterward [28,684 (14,655–72,286) vs. 98,606 (54,170–152,643) €/QALY; p < 0.001]. In sensitivity analysis cost utility increased when all patients with APACHE II scores over 20 were excluded [149,536 (25,402–1,795,012) €/QALY], when all patients over 65 years old were excluded [95,687 (23,481–1,966,824) €/QALY] and when all patients treated in the intensive care unit were excluded [97,614 (17,239–477,776) €/QALY]. In contrast, cost utility decreased when all patients treated in the hospital wards were excluded [607,993 (33,934–2,562,062) €/QALY]. Excluding all patients with chronic renal disease before hospitalization or increasing post-hospital costs by 50 % did not have a major effect on overall cost utility [315,049 (27,003–2,332,220) and 316,648 (34,41–2,177,581) €/QALY]. The results of the subanalysis on ICU patients are presented in Table 4. Five-year CU was best in hospital survivors with renal recovery [survival time <1 year: 307,254 (91,305–851,742), 1–5 years: 37,172 (16,199–113,037), >5 years: 21,670 (12,551–36,679) €/QALY].
Discussion
We studied the 5-year cost utility of acute RRT in 410 patients treated in 2000–2002 at Helsinki University Hospital. The cost utility of acute RRT was 270,000 €/QALY for all patients and 34,000 €/QALY for hospital survivors. Total hospital and societal costs were 41,000 € per patient in 5 years, and median survival time for our patients was 0.2 years.
The overall outcome of our cohort was poor, but in agreement with other studies of RRT-treated acute kidney injury patients [3, 10]. Approximately half of our patients died during initial hospitalization, and the median survival of the cohort was only 0.2 years. In general, the prognosis of AKI patients differs regarding to co-morbidities and severity of illness. Recently, high mortality rates have been observed in AKI patients with septic shock [26] and in patients who develop severe AKI after cardiac surgery [22, 27, 28]. Long-term prognosis after acute RRT, however, has been shown to be fairly good, both in cardiac surgery patients [22, 29] and in heterogenic patient populations [1, 13, 16, 30, 31]. In our study the mortality also stabilized over time, resulting in 5-year mortality of 66 %.
In this study total hospital and societal costs for the 5-year follow-up period were approximately 41,000 € per patient and 64,000 € per hospital survivor. Presumably because hospital non-survivors were more severely ill than survivors, the cost of the index hospitalization did not differ between hospital survivors and non-survivors although the length of hospital stay was three times longer for hospital survivors. Previous results on the subject are diverse. Gopal et al. [13] described direct ICU costs to be around 44,000$/year in survivors of severe AKI. On the other hand, others have presented higher costs [1, 28]. In the study by Dasta et al. [28], 258 cardiac surgery patients with AKI generated a cost of 18.3$ million (around 71,000$/patient) during the index hospitalization, and Korkeila et al. [1] reported direct ICU costs to be around 80,000$ per 6-month survivor.
We found that the overall cost utility of acute RRT was poor, exceeding 50,000 €/QALY, a threshold suggested in the literature [15]. Although the overall CU ratio was approximately 270,000 €/QALY, there were patient subpopulations in which the CU was acceptable or good. In patients who survived for more than 1 year, the 5-year CU ratio was around 45,000 €/QALY and in 5-year survivors around 20,000 €/QALY. Cost utility of acute RRT was better for younger patients, with 5-year CU 74,000 €/QALY for patients under 50 years old. However, CU exceeded 750,000 €/QALY for patients over 65 years (Fig. 2). Comparable results have been reported from the SUPPORT study, with a CE ratio of around 128,200$/QALY [23]. However, they found that the CE was poor in all survival groups [23]. Cox and colleagues have previously reported that patient age was the most important factor in determining CE in patients with prolonged mechanical ventilation [32].
We previously estimated that the CU in these patients would be approximately 200,000 €/QALY using a median follow-up time of 2.4 years and only hospital costs [14]. The present study was a secondary analysis of the same cohort with a 5-year follow-up and used a societal perspective including out-of-hospital costs up to 5 years. In this study using a different approach, the estimated CU for the whole patient population was approximately of the same magnitude. Due to the short median survival time of these patients, the initial hospital treatment seems to be the most important factor determining cost utility.
Studies on cost-effectiveness of acute RRT are limited [14, 23, 24]. The SUPPORT study studied the outcome and cost-effectiveness of acute RRT in 490 patients undergoing either hemodialysis or peritoneal dialysis [23]. They included hospital costs for initial hospital treatment and all readmissions to the same hospital up to 6 months and reported that costs/QALY exceeded 50,000$/QALY in all patient groups. Others have reported CE for daily dialysis to be 5,000$/QALY [24]. However, neither study considered societal costs. We found that cost utility of acute RRT was good in patients who had no chronic renal disease before hospitalization and whose renal function recovered (26,000 €/QALY). In general, this was the first study on cost utility of acute RRT to include health-related societal costs into the analysis.
Some limitations of our study should be addressed. This was a single-center study. Therefore, the generalizability is limited since the cost of RRT varies between centers and is affected by the nursing ratio per patient, the choice of anticoagulation and replacement fluids used [33]. Indications for acute RRT vary across centers, affecting the outcome of the patient and the length and cost of hospital treatment, and costs vary depending on the financing of the health-care system. In Finland the health-care system is based on public funding by taxes. In addition, patients may choose to use private health care, which the patients pay for themselves. In that case, the Social Insurance Institution of Finland (which is also covered by taxes) compensates for some of the costs. It also compensates in part for the cost of medication and the loss of income in case of disablement. In our study all post-hospital costs were not available, but increasing post-hospital costs by 50 % in sensitivity analysis did not affect overall CU. Also, we did not try to estimate the incremental costs of RRT. Instead, we assumed that discontinuing RRT would in most cases result in the patient’s death, and thus we used total costs in the CU analysis. Additionally, HRQoL in this study was measured once, in 2003, although several HRQoL measurements over time would have been optimal. However, in a previous study we were unable to show that the length of the follow-up period affected HRQoL, and therefore we believe that a wide time range (6 months–3.5 years) between hospital admission and HRQoL measurement was not a disadvantage. With increasing age, the HRQoL tends to decrease, and we tried to take that into account by considering a yearly discount of 3 % to predict changes over a lifetime. As a result we believe that this study gives a reasonably good estimation of the lifelong cost utility of acute RRT.
In conclusion, based on a cost-utility analysis of acute RRT from a societal perspective, 5-year follow-up and lifetime scale, we found that in general the cost utility of acute RRT is poor. However, the cost utility of acute RRT seems to be good in patients who do not need chronic RRT and who survive for more than a year.
References
Korkeila M, Ruokonen E, Takala J (2000) Costs of care, long-term prognosis and quality-of-life in patients requiring renal replacement therapy during intensive care. Intensive Care Med 26:1824–1831
Bagshaw SM, Laupland KB, Doig CJ, Mortis G, Fick GH, Mucenski M, Godinez-Luna T, Svenson LW, Rosenal T (2005) Prognosis for long-term survival and renal recovery in critically ill patients with severe acute renal failure: a population-based study. Crit Care 9:R700–R709
Vaara ST, Pettilä V, Reinikainen M, Kaukonen K-M (2012) Population-based incidence, mortality and quality of life in critically ill patients treated with renal replacement therapy: a nationwide retrospective cohort study in Finnish ICUs. Crit Care 16:R13
Hsu CY, McCulloch CE, Fan D, Ordonez JD, Chertow GM, Go AS (2007) Community-based incidence of acute renal failure. Kidney Int 27:208–212
Bagshaw SM, George C, Bellomo R, ANZICS Database Management Committee (2007) Changes in the incidence and outcome for early acute kidney injury in a cohort of Australian intensive care units. Crit Care 11:R68
Uchino S, Bellomo R, Goldsmith D, Bates S, Ronco C (2006) An assessment of the RIFLE criteria for acute renal failure in hospitalized patients. Crit Care Med 34:1913–1917
Groeneveld AB, Tran DD, van der Meulen J, Nauta JJ, Thijs LG (1991) Acute renal failure in the medical intensive care unit: predisposing, complicating factors and outcome. Nephron 59:602–610
Brivet FG, Kleinknecht DJ, Loirat P, Landais PJ (1996) Acute renal failure in intensive care units—causes, outcome and prognostic factors of hospital mortality; a prospective, multicenter study. French Study Group on Acute Renal Failure. Crit Care Med 24:192–198
De Mendonca A, Vincent JL, Suter PM, Moreno R, Dearden NM, Antonelli M, Takala J, Sprung C, Cantraine F (2000) Acute renal failure in the ICU: risk factors and outcome evaluated by the SOFA score. Intensive Care Med 26:915–921
Uchino S, Kellum JA, Bellomo R, Doig GS, Morimatsu H, Morgera S, Schetz M, Tan I, Bouman C, Macedo E, Gibney N, Tolwani A, Ronco C (2005) Acute renal failure in critically ill patients: a multinational, multicenter study. JAMA 294:813–818
Åhlström A, Kuitunen A, Peltonen S, Hynninen M, Tallgren M, Aaltonen J, Pettilä V (2006) Comparison of 2 acute renal failure severity scores to general scoring systems in the critically ill. Am J Kidney Dis 48:262–268
Ricci Z, Cruz D, Ronco C (2008) The RIFLE criteria and mortality in acute kidney injury. A systematic review. Kidney Int 73:538–546
Gopal I, Bhonagiri S, Ronco C, Bellomo R (1997) Out of hospital outcome and quality of life in survivors of combined acute multiple organ and renal failure treated with continuous venovenous hemofiltration/hemodiafiltration. Intensive Care Med 23:766–772
Åhlström A, Tallgren M, Peltonen S, Räsänen P, Pettilä V (2005) Survival and quality of life of patients requiring acute renal replacement therapy. Intensive Care Med 31:1222–1228
Hirth RA, Chernew ME, Miller E, Fendrick AM, Weissert WG (2000) Willingness to pay for a quality-adjusted life year: in search of a standard. Med Decis Making 20:332
Morgera S, Kraft AK, Siebert G, Luft FC, Neumayer H–H (2002) Long-term outcomes in acute renal failure patients treated with continuous renal replacement therapies. Am J Kidney Dis 40:275–279
Rimes-Stigare C, Awad A, Mårtensson J, Martling C-R, Bell M (2012) Long-term outcome after acute renal replacement therapy: a narrative review. Acta Anaesth Scand 56:138–146
Wald R, Quinn RR, Luo J, Li P, Scales DC, Mamdani MM, Ray JG, University of Toronto Acute Kidney Injury Research Group (2009) Chronic dialysis and death among survivors of acute kidney injury requiring dialysis. JAMA 302:1179–1185
Delannoy B, Floccard B, Thiolliere F, Kaaki M, Badet M, Rosselli S, Ber CE, Saez A, Flandreau G, Guerin C (2009) Six-month outcome in acute kidney injury requiring renal replacement therapy in the ICU: a multicentre prospective study. Intensive Care Med 35:1907
Johansen KL, Smith MW, Unruh ML, Siroka AM, O’Connor TZ, Palevsky PM, VA/NIH Acute Renal Failure Trial Network (2010) Predictors of health utility among 60-day survivors of acute kidney injury in the Veterans Affairs/National Institutes of Health Acute Renal Failure Trial Network Study. Clin J Am Soc Nephrol 5:1366–1372
Morsch C, Thome FS, Balbinotto A, Guimaraes JF, Barros EG (2011) Health-related quality of life and dialysis dependence in critically ill patient survivors of acute kidney injury. Ren Fail 33:949–956
Landoni G, Zangrillo A, Franco A, Aletti G, Roberti A, Calabrò MG, Slaviero G, Bignami E, Marino G (2006) Long-term outcome of patients who require renal replacement therapy after cardiac surgery. Eur J Anaesthesiol 23:17–22
Hamel MB, Phillips RS, Davis RB, Desbiens N, Connors AF, Teno JM, Wenger N, Lynn J, Wu AW, Fulkerson W, Tsevat J, for the SUPPORT Investigators, (1997) Outcomes and cost-effectiveness of initiating and continuing aggressive care in seriously ill hospitalized adults. Ann Intern Med 127:195–202
Desai A, Baras J, Berk BB, Nakajima A, Garber A, Owens D, Chertow G (2008) Management of acute kidney injury in the intensive care unit. A cost-effectiveness analysis of daily vs alternate-day hemodialysis. Arch Intern Med 168:1761–1767
Brooks R, with the EuroQol Group (1996) EuroQol: the current state of play. Health Policy 37:53–72
Bagshaw SM, Lapinsky S, Dial S, Arabi Y, Dodek P, Wood G, Ellis P, Guzman J, Marshall J, Parrillo JE, Skrobik Y, Kumar A (2009) Acute kidney injury in septic shock: clinical outcomes and impact of duration of hypotension prior to initiation of antimicrobial therapy. Intensive Care Med 35:871–881
Kuitunen A, Vento A, Suojaranta-Ylinen R, Pettilä V (2006) Acute renal failure after cardiac surgery: evaluation of the RIFLE classification. Ann Thorac Surg 81:542–546
Dasta JF, Kane-Gill SL, Durtschi AJ, Pathak DS, Kellum JA (2008) Costs and outcomes of acute kidney injury (AKI) following cardiac surgery. Nephrol Dial Transpl 23:1970–1974
Luckraz H, Gravenor MB, George R, Taylor S, Williams A, Ashraf S, Argano V, Youhana A (2005) Long and short-term outcomes in patients requiring continuous renal replacement therapy post cardiopulmonary bypass. Eur J Cardiothorac Surg 27:906–909
Coxa SG, Yusuf B, Shlipak MG, Garg AX, Parikh CR (2009) Long-term risk of mortality and other adverse outcomes after acute kidney injury: a systematic review and meta-analysis. Am J Kidney Dis 53:961–973
Van Berendoncks AM, Elseviers MM, Lins RL, for the SHARF Study Group (2010) Outcome of acute kidney injury with different treatment options: long-term follow-up. Clin J Am Soc Nephrol 5:1755–1762
Cox CE, Carson SS, Govert JA, Chelluri L, Sanders GD (2007) An economic evaluation of prolonged mechanical ventilation. Crit Care Med 35:1918–1927
Srisawat N, Lawsin L, Uchino S, Bellomo R, Kellum JA, BEST Kidney Investigators (2010) Cost of acute renal replacement therapy in the intensive care unit: results from The Beginning and Ending Supportive Therapy for the Kidney (BEST Kidney) Study. Crit Care 14:R46
Acknowledgments
We thank Prof. Seppo Sarna for his help in the statistical analysis.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Laukkanen, A., Emaus, L., Pettilä, V. et al. Five-year cost-utility analysis of acute renal replacement therapy: a societal perspective. Intensive Care Med 39, 406–413 (2013). https://doi.org/10.1007/s00134-012-2760-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-012-2760-4