Abstract
Purpose
Patients undergoing cardiac surgery often require transfusions of red blood cells, plasma and platelets. These components differ widely in both indications for use and composition. However, from a statistical point of view there is a significant colinearity between the components. This study explores the relation between the transfusion of different blood components and long-term mortality.
Methods
A retrospective single-centre study was performed including 5,261 coronary artery bypass grafting patients, excluding patients receiving more than eight units of red blood cells, those suffering early death (7 days) and emergency cases. Patients were followed up for a period of up to 7.5 years. A broad spectrum of potential risk factors was analysed using Cox proportional hazards survival regression. Non-significant risk factors were removed by step-wise elimination, and transfusion of red blood cells, plasma and platelets was forced to remain in the model.
Results
The transfusion of red blood cells was not associated with decreased long-term mortality (HR = 1.007, p = 0.775), whereas the transfusion of plasma was associated with decreased long-term survival (HR = 1.060, p < 0.001), and the transfusion of platelets was associated with increased long-term survival (HR = 0.817, p = 0.011). The risk associated with transfusion of plasma was mainly attributed to patients receiving large amounts of plasma. All hazard ratios are per unit of blood product transfused.
Conclusions
No association was found between the transfusion of red blood cells and mortality during the study period. However, transfusion of plasma was associated with increased mortality while transfusion of platelets was associated with decreased mortality during the study period.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The benefits and risks of blood transfusions during and after cardiac surgery are the subject of considerable debate in both academic and clinical setting. Associations between blood transfusion and decreased long-term survival have been reported in several retrospective studies [1–8], while other studies have revealed conflicting results [9]. Furthermore, in a previous study, we found that the risk associated with RBC transfusion was almost completely eliminated by introducing preoperative haemoglobin levels and renal function into the model [10].
In most of the publications mentioned above only red blood cell (RBC) transfusion was studied, whereas in reality many patients also receive transfusions of plasma and platelets as well. From a clinical and statistical point of view, there is significant colinearity between these different types of transfusions, but from an immunological standpoint, these different blood components differ in many ways [11]. Few studies have been carried out on the effects of the transfusion of different blood components other than RBCs. Koch et al. reported platelet transfusion to have a beneficial effect [3, 12], while Ranucci et al. reported that platelet transfusion was associated with increased in-hospital mortality and that plasma transfusion had a negative effect [3, 12].
The aim of the present study was to evaluate the effects of the transfusion of different blood components on long-term mortality. Our goal was to create a more robust model by including additional risk factors and all types of transfusions.
Methods
Study design
The study protocol was approved by the local ethics committee. The patients included in this study had undergone cardiac surgery at the Department of Thoracic Surgery at the University Hospital in Lund, Sweden, from 1 January 2002 to 31 December 2008. Data were collected from four principal sources. Clinical data were retrieved from the in-house clinical database in which relevant clinical information is collected on perioperative care during the patients’ hospital stay. The databases of the hospital’s clinical chemistry laboratory and blood bank served as the second and third sources of data. Time of death was obtained from the Swedish tax authority in May 2009, defining the follow-up period of 0.5–7.5 years. When data were missing or extreme outliers were identified, patient records were read in a first attempt to complete the data.
Patient inclusion and exclusion
Data were gathered on all patients who had undergone coronary artery bypass grafting (CABG) as their sole cardiac procedure (n = 5,922). Patients who had undergone emergency surgery, defined as surgery within 1 h of the decision to operate, were excluded (n = 121), as were those who died during the first 7 days following surgery (n = 34) and those who had received 8 or more units of RBCs (n = 506). Eight units was chosen since, together with plasma, this represents more than half the blood volume in most adult patients and indicates massive bleeding, in which case the transfusion was life-saving. A total of 5,261 patients were finally included in the analysis.
Completeness and reliability of the data
Perioperative information was entered into the in-house clinical database by each surgeon (100 % completion rate). Information on deaths was obtained from the Swedish tax authority, which lacks data only in exceptional cases such as emigration. The emigration rate for all Swedes in this age category is approximately 0.1 % per year [14]. Preoperative creatinine values were missing from the chemistry laboratory data for 104 patients and were imputed based on levels on the first postoperative day [10]. Preoperative haemoglobin concentrations were not available for 21 patients, and a standard mean value substitution method was employed.
The postoperative renal function of the patients was categorised using the RIFLE criteria (Risk-Injury-Failure-Loss-End Stage) based on the preoperative creatinine level and the maximum creatinine level during the hospital stay [15]. Renal function was also expressed as the estimated glomerular filtration rate (eGFR) and calculated according to the MDRD formula (Modification of Diet in Renal Disease) [16]:
where eGRF is expressed as (ml/min/1.73 m2), serum creatinine in μmol/l and age in years.
Surgery and postoperative care
Surgery was performed in a standardised manner. The use of aprotinin and tranexamic acid was left to the discretion of the individual surgeon. During the patient’s stay in the intensive care unit (ICU), extra aprotinin, protamine, tranexamic acid or desmopressin was administered based on coagulation analyses or clinical assessment. No pre-defined limits for RBC transfusion or reoperation for bleeding were used during the period, and indications for transfusion of blood products were determined by the physician in charge of the ICU or the ward after clinical judgement.
Selection of outcome variables and statistical analysis
The variables used for survival analysis were based on frequently found predictors for decreased survival in recent survival studies focusing on renal function or RBC transfusion in cardiac surgery [1–4, 9, 17–19]. In addition, we included other potential risk factors and preoperative laboratory parameters that could reflect the preoperative morbidity of importance for long-term survival. The following variables were entered as dichotomous variables: gender, diabetes, chronic obstructive pulmonary disease (COPD), history of cerebrovascular disease, peripheral vascular disease, left ventricular ejection fraction (LVEF) 30–50 %, LVEF <30 %, recent myocardial infarction, known pulmonary hypertension (systolic pressure >60 mmHg), acute coronary symptoms, previous CABG, previous percutaneous coronary intervention (PCI), use of cardiopulmonary bypass, intra-aortic balloon pump (IABP) before surgery, IABP after surgery, postoperative sepsis, postoperative stroke, postoperative atrial fibrillation, perioperative myocardial infarction, and re-operation for bleeding or mediastinitis. Perfusion time, age, time on the ventilator in the ICU and BMI were entered as continuous variables. Renal function (expressed as preoperative eGFR), haemoglobin, plasma C-reactive protein, plasma alanine aminotransferase, plasma leukocyte count and platelet count were entered as continuous variables. For the 195 patients who underwent off-pump surgery, the perfusion time used in the analysis was the mean value for the other 5,066 patients. Transfusion of blood products was defined as a transfusion during surgery or during the postoperative stay and was entered as a continuous variable representing units of blood products transfused.
The Cox proportional hazard model was used to determine which factors affected long-term survival, and the Wald test was used to determine the strength of the relation. For missing data, mean substitution was used. A backward stepwise elimination procedure was used starting with the above-mentioned variables. Variables with p < 0.05 were retained in the model together with transfusion of blood products regardless of their level of significance. Variables with p > 0.05 were removed in order of strength as defined by the level of significance. After all non-significant variables had been removed, they were entered one at the time to confirm that they were not relevant to the model. To check the linearity of the risk associated with plasma transfusion, plasma was categorised in four different categories and four new variables were created (no plasma transfusion, 1–2, 3–4, 5–6 or more that 6 units of plasma transfused) and entered into the model instead of plasma as continuous variable. The interaction between different types of transfusion was evaluated by creating eight variables (RBC transfusion yes/no, plasma transfusion yes/no and platelet transfusion yes/no). These variables were then entered in the final model, and the continuous variables for units of blood products were removed from the model. Student’s t test was used for group comparisons, where numbers were large and the distributions not strongly skewed; otherwise the Wilcoxon-Mann-Whitney test was performed. Unless otherwise stated, the results are presented as the mean ± 1 SD. The R-project software (version 2.13.0) with the survival package was used to test the proportional hazards assumption for a Cox regression model fit. All other statistical calculations were performed using Statistica, version 8 (StatSoft inc, Tulsa, OK, USA).
Results
Study population
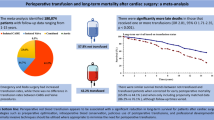
Patients were followed for between 152 and 2,706 days (mean 1,423 days). During follow-up there were 503 deaths. Among the patients, 2,618 (49.8 %) received RBC transfusion, 1,533 (29.1 %) received plasma transfusion and 418 (7.9 %) received platelets (Fig. 1). Patient characteristics are described in Table 1.
Analysis of patients receiving plasma transfusions
Patients who received plasma showed more preoperative comorbidity (Table 1) and more postoperative complications (Table 2) than patients not receiving plasma. The patients given plasma received on average 4.2 ± 4.0 units of plasma, and 80.7 % also received an average of 3.0 ± 2.1 units of RBCs.
Cox analysis
Stepwise elimination of non-significant variables in the Cox proportional hazards ratio analysis left 16 variables in the model: age (per year), COPD, diabetes, history of cerebrovascular disease, peripheral vascular disease, female gender, previous myocardial infarction, LVEF <30 %, previous CABG, perfusion time (per min), permanent stroke, preoperative haemoglobin (per g/l), preoperative eGFR (per ml/min/1.73 m2), transfusion of RBC (per unit), transfusion of plasma (per unit) and transfusion of platelets (per unit). Transfusion of the three different blood products was forced to remain in the model. RBC transfusion gave a hazard ratio (HR) of 1.007 (95 % CI 0.96–1.06, p = 0.775), transfusion of plasma gave a HR of 1.060 (95 % CI 1.04–1.09, p < 0.001) and transfusion of platelets gave a HR of 0.817 (95 % CI 0.70–0.96, p = 0.011) for each unit transfused (Table 3).
When plasma was entered in the analysis as a categorical variable, the HR for 1–2 plasma transfusions became 1.18 (95 % CI 0.91–1.54, p = 0.212), the HR for 3–4 plasma transfusions became 1.28 (95 % CI 0.95–1.75, p = 0.107), the HR for 5–6 plasma transfusions became 1.142 (95 % CI 0.70–1.87, p = 0.599), and the HR for 7 or more plasma transfusions became 1.710 (95 % CI 1.21–2.42, p = 0.003, Fig. 2).
The result of the interaction analysis only revealed one significant interaction, and it was the group that received RBC and plasma transfusion, but not platelet transfusion, with a HR of 1.52 (95 % CI 1.20–1.95, p = <0.001). The group that received only RBC transfusion had a HR of 1.15 (95 % CI 0.89–1.48, p = 0.266). None of the other groups were significant (Table 4).
Discussion
Two principal findings were made in this study. First, we found an association between plasma transfusion and increased long-term mortality. Secondly, we found no association between RBC transfusion and long-term survival. These findings challenge the current view on transfusion after cardiac surgery.
The finding that there was no significant correlation between RBC transfusion and long-term survival is in contrast to the results of the majority of studies published to date. Previous studies have reported hazards ratios for long-term mortality between 1.03 and 2.4, depending on the study design and whether transfusion was entered as a dichotomous variable or continuous variable [1, 2, 4, 6–8, 10, 20, 21]. In a previous study on the same cohort, we found a hazard ratio of 1.10 when using a model similar to that in other studies, but when we included preoperative eGFR and haemoglobin levels the hazard ratio decreased to 1.05 and was no longer significant [10]. By increasing the number of potential risk factors and including all types of transfusion, the present study revealed a hazard ratio of 1.007 for RBC transfusion with a confidence interval of 0.96–1.06, thereby further diminishing any risk associated with RBC transfusion. From a statistical point of view, it appears that RBC transfusion and plasma transfusion interact strongly. When including plasma transfusion in the model, the risk associated with RBC transfusion was further decreased, since our model revealed that the associated risk from RBC transfusion actually belonged to plasma transfusion. In an editorial, Engoren commented on our previous article and concluded that just showing that transfusion of RBC is not dangerous may not be enough [10, 22]. Instead, we should try to find improved outcomes of transfusions in these patients. The findings of this study take at least one step in that direction.
The results of the present study indicate that plasma transfusion in cardiac surgery is associated with decreased long-term survival and that this risk is found in patients receiving many plasma transfusions. Similar findings that plasma transfusion is associated with worse outcome have been reported in a few studies on patient populations mostly receiving massive transfusions. A study based on the trauma-associated severe haemorrhage (TASH) score [23], which was used to objectively determine which patients would benefit or exhibit increased complications as a result of a high plasma:RBC ratio after severe trauma, demonstrated that the outcome was indeed dependent on the TASH score, where a high plasma:RBC ratio was associated with an adverse outcome [24]. However, in a recent meta-analysis, plasma transfusion was associated with a reduction in the risk of death and multiorgan failure in patients undergoing massive transfusions. The results were based on studies judged to have “very-low-quality” evidence [13]. Plasma transfusion also significantly reduced the risk of multiorgan failure, but increased the risk of acute lung injury [13]. In patients undergoing cardiac surgery without the need for massive transfusions, plasma transfusion was found to markedly increase short-term mortality [12, 25]. Our finding that plasma transfusion is associated with decreased long-term survival seems to be in agreement with the reports of other authors on short-term outcome. However, no one has yet been able to ascertain whether it is the plasma per se or the need for plasma transfusion that carries the risk. Significant risk were only found in patients receiving seven or more units of plasma, and in these patients the high rate of plasma transfusion might be explained by a comorbidity and not a bleeding. Therefore, we should be careful in drawing any far-reaching conclusions from this finding.
Platelet transfusion was found to be associated with decreased mortality, although previous studies have reported conflicting results [3, 12, 26]. The clinical indication for platelet transfusion intra- and postoperatively in cardiac surgery is mainly bleeding, and platelets are often administered together with plasma and/or RBC transfusion, which makes the situation more complex. It was recently reported that fresh frozen plasma and platelet transfusion carry a higher risk of short-term mortality than transfusions of packed red blood cells [12]. Morphological, biochemical and functional changes occur in platelets during storage [27]. However, platelet storage time was not found to be associated with adverse short-term outcomes, decreased long-term survival or infections after cardiac surgery [28]. Our finding that platelet transfusion may be associated with better outcome is difficult to explain based on the information available from our studies and those of others, and could be a coincidental finding of little clinical relevance. However, one explanation could be that platelet transfusion is a surrogate marker for reduced or impaired platelet function, which may be pharmacologically induced or naturally low. The assumption that the need for platelet transfusion is related to lower platelet function and consequently associated with a lower incidence of future thromboembolic events, thereby increasing the chances of longer life, is, with the present knowledge, theoretical. In addition, we did not have access to information on preoperative antiplatelet therapy, further precluding any potential relation from being revealed.
This study has some limitations. First of all, a larger sample size would have been preferable to more accurately determine the relationship between transfusion and outcome. Secondly, some concern has been expressed about the storage time of RBCs and plasma and the effect on outcome after cardiac surgery. For example, van Straten et al. [29] have shown that a longer plasma storage time is a risk factor for early but not late mortality in CABG patients, while Koch found that the age of RBCs affected long-term survival negatively [30]. Unfortunately, we did not have access to the age of the blood products given. Thirdly, we did not distinguish between fresh frozen plasma, fresh plasma or leukocyte-depleted blood products in this study. The use of leukocyte-depleted blood products has been routine for several years in patients undergoing cardiac surgery at our clinic, but we cannot guarantee that some patients were given non-leukocyte-depleted transfusions. It could also be argued that by excluding patients receiving eight or more units of RBCs, we excluded the patients exposed to the largest transfusions, thereby missing relevant information. We therefore included the patients receiving more than eight units in a post hoc analysis, and while the hazard ratio for RBC transfusion remained virtually the same (1.005, 95 % CI 0.98–1.03), the value for plasma decreased from 1.060 (95 % CI 1.04–1.09) to 1.028 (95 % CI 1.02–1.04). However, we still believe that in this study it is not relevant to analyse the potential risks of transfusion in patients requiring a transfusion to survive. The aim of the present study was to investigate the long-term effects of blood product transfusion in cardiac surgery patients, and we therefore excluded patients who died within 7 days of surgery. In a post hoc analysis, the patients who died during the first week were included, and it did not change the results regarding transfusion and outcome. Moreover, patients dying during the first week are a heterogeneous group, often representing outliers in several ways, and may jeopardise the proportional hazard assumption. The relevant clinical question is whether a different transfusion regimen could have prevented any of the patients from dying within 7 days and changed the outcome of the analysis. This is a limitation in retrospective studies such as this. To shed some light on the issue, a separate analysis should be performed on this subgroup. On the other hand, one strength of the study is the completeness of the database, where important variables have a more than 99.5 % completion rate.
The results of this study emphasise the fundamental differences between different blood products by showing that long-term outcome differs depending on the type of transfusion given. Reliable and accurate data on the long-term risks of transfusions are paramount in making valid transfusion recommendations, and our findings may serve as a step in that direction as long as firmer evidence in form of randomised trials is lacking.
References
Engoren MC, Habib RH, Zacharias A, Schwann TA, Riordan CJ, Durham SJ (2002) Effect of blood transfusion on long-term survival after cardiac operation. Ann Thorac Surg 74:1180–1186
Koch CG, Li L, Duncan AI, Mihaljevic T, Cosgrove DM, Loop FD, Starr NJ, Blackstone EH (2006) Morbidity and mortality risk associated with red blood cell and blood-component transfusion in isolated coronary artery bypass grafting. Crit Care Med 34:1608–1616
Koch CG, Li L, Duncan AI, Mihaljevic T, Loop FD, Starr NJ, Blackstone EH (2006) Transfusion in coronary artery bypass grafting is associated with reduced long-term survival. Ann Thorac Surg 81:1650–1657
Kuduvalli M, Oo AY, Newall N, Grayson AD, Jackson M, Desmond MJ, Fabri BM, Rashid A (2005) Effect of peri-operative red blood cell transfusion on 30-day and 1-year mortality following coronary artery bypass surgery. Eur J Cardiothorac Surg 27:592–598
Spiess BD (2004) Transfusion of blood products affects outcome in cardiac surgery. Semin Cardiothorac Vasc Anesth 8:267–281
Murphy GJ, Reeves BC, Rogers CA, Rizvi SI, Culliford L, Angelini GD (2007) Increased mortality, postoperative morbidity, and cost after red blood cell transfusion in patients having cardiac surgery. Circulation 116:2544–2552
Surgenor SD, Kramer RS, Olmstead EM, Ross CS, Sellke FW, Likosky DS, Marrin CA, Helm RE Jr, Leavitt BJ, Morton JR, Charlesworth DC, Clough RA, Hernandez F, Frumiento C, Benak A, DioData C, O’Connor GT (2009) The association of perioperative red blood cell transfusions and decreased long-term survival after cardiac surgery. Anesth Analg 108:1741–1746
van Straten AH, Soliman Hamad MA, van Zundert AA, Martens EJ, ter Woorst JF, de Wolf AM, Scharnhorst V (2011) Effect of duration of red blood cell storage on early and late mortality after coronary artery bypass grafting. J Thorac Cardiovasc Surg 141:231–237
Engoren M, Arslanian-Engoren C (2009) Long-term survival in the intensive care unit after erythrocyte blood transfusion. Am J Crit Care 18:124–131; quiz 132
Dardashti A, Ederoth P, Algotsson L, Bronden B, Luhrs C, Bjursten H (2011) Blood transfusion after cardiac surgery: is it the patient or the transfusion that carries the risk? Acta Anaesthesiol Scand 55:952–961
Klein H (2005) Immunology of leucocytes, platelets and plasma components mollison’s blood transfusion in clinical medicine. Blackwell Science Ltd, Malden, pp 546–610
Ranucci M, Pazzaglia A, Bianchini C, Bozzetti G, Isgro G (2008) Body size, gender, and transfusions as determinants of outcome after coronary operations. Ann Thorac Surg 85:481–486
Murad MH, Stubbs JR, Gandhi MJ, Wang AT, Paul A, Erwin PJ, Montori VM, Roback JD (2012) The effect of plasma transfusion on morbidity and mortality: a systematic review and meta-analysis. Transfusion 50:1370–1383
Statistiska centralbyrån. www.scb.se
Venkataraman R, Kellum JA (2007) Defining acute renal failure: the RIFLE criteria. J Intensive Care Med 22:187–193
Foot CL, Chinthamuneedi M, Fraser JF, Smith SE, Fayers T, Tesar P, Mullany DV (2009) The association between preoperative eGFR and outcomes in cardiac surgical patients. Crit Care Resusc 11:184–190
Brown JR, Cochran RP, MacKenzie TA, Furnary AP, Kunzelman KS, Ross CS, Langner CW, Charlesworth DC, Leavitt BJ, Dacey LJ, Helm RE, Braxton JH, Clough RA, Dunton RF, O’Connor GT (2008) Long-term survival after cardiac surgery is predicted by estimated glomerular filtration rate. Ann Thorac Surg 86:4–11
Hobson CE, Yavas S, Segal MS, Schold JD, Tribble CG, Layon AJ, Bihorac A (2009) Acute kidney injury is associated with increased long-term mortality after cardiothoracic surgery. Circulation 119:2444–2453
Hillis GS, Croal BL, Buchan KG, El-Shafei H, Gibson G, Jeffrey RR, Millar CG, Prescott GJ, Cuthbertson BH (2006) Renal function and outcome from coronary artery bypass grafting: impact on mortality after a 2.3-year follow-up. Circulation 113:1056–1062
Engoren M, Habib RH, Hadaway J, Zacharias A, Schwann TA, Riordan CJ, Durham SJ, Shah A (2009) The effect on long-term survival of erythrocyte transfusion given for cardiac valve operations. Ann Thorac Surg 88:95–100, 100 e101–100 e103
Koch CG, Khandwala F, Li L, Estafanous FG, Loop FD, Blackstone EH (2006) Persistent effect of red cell transfusion on health-related quality of life after cardiac surgery. Ann Thorac Surg 82:13–20
Engoren M (2011) Transfusion: is merely not bad good enough? Acta Anaesthesiol Scand 55:907–909
Maegele M, Lefering R, Wafaisade A, Theodorou P, Wutzler S, Fischer P, Bouillon B, Paffrath T (2011) Revalidation and update of the TASH-score: a scoring system to predict the probability for massive transfusion as a surrogate for life-threatening haemorrhage after severe injury. Vox Sang 100:231–238
Borgman MA, Spinella PC, Holcomb JB, Blackbourne LH, Wade CE, Lefering R, Bouillon B, Maegele M (2011) The effect of FFP:RBC ratio on morbidity and mortality in trauma patients based on transfusion prediction score. Vox Sang 101:44–54
Bilgin YM, van de Watering LM, Versteegh MI, van Oers MH, Vamvakas EC, Brand A (2011) Postoperative complications associated with transfusion of platelets and plasma in cardiac surgery. Transfusion 51:2603–2610
Karkouti K, Wijeysundera DN, Yau TM, Callum JL, Meineri M, Wasowicz M, McCluskey SA, Beattie WS (2006) Platelet transfusions are not associated with increased morbidity or mortality in cardiac surgery. Can J Anaesth 53:279–287
Devine DV, Serrano K (2010) The platelet storage lesion. Clin Lab Med 30:475–487
Welsby IJ, Lockhart E, Phillips-Bute B, Campbell ML, Mathew JP, Newman MF, Peterson E, Milano CA (2010) Storage age of transfused platelets and outcomes after cardiac surgery. Transfusion 50:2311–2317
van Straten AH, Soliman Hamad MA, Martens EJ, Tan ME, de Wolf AM, Scharnhorst V, van Zundert AA (2010) Effect of storage time of transfused plasma on early and late mortality after coronary artery bypass grafting. J Thorac Cardiovasc Surg 141(238–243):e231–e232
Koch CG, Li L, Sessler DI, Figueroa P, Hoeltge GA, Mihaljevic T, Blackstone EH (2008) Duration of red-cell storage and complications after cardiac surgery. N Engl J Med 358:1229–1239
Acknowledgments
We would like to express our gratitude to Assistant Prof. Peter Höglund for his invaluable help with survival statistics and Prof. Martin L. Olsson for providing transfusion data. This study was funded by hospital and Swedish governmental grants.
Conflicts of interest
Henrik Bjursten has a vested interest in ErySave AB. Lars Algotsson lectures for Orion Pharma AB and Abbott Scandinavia AB. The other authors have no conflicts of interest to report.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bjursten, H., Dardashti, A., Ederoth, P. et al. Increased long-term mortality with plasma transfusion after coronary artery bypass surgery. Intensive Care Med 39, 437–444 (2013). https://doi.org/10.1007/s00134-012-2723-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-012-2723-9