Abstract
Purpose
To assess the prevalence and predictive value of natural autoantibodies to high-mobility group box 1 (HMGB1) during sepsis.
Methods
Anti-HMGB1 and anti-human serum albumin (HSA) autoantibodies were detected by ELISA in 178 plasma samples longitudinally collected from 40 critically ill patients with septic shock. One hundred thirty-two plasma samples from healthy donors were used as control.
Results
IgGs to HMGB1 were detected in 15/40 patients (37.5%). The prevalence of anti-HMGB1 antibodies was significantly higher in the patients who survived (55%) compared to the patients who did not (20%) (p < 0.0001). The detection of anti-HMGB1 antibodies during the course of the disease was significantly associated with patient survival (p = 0.038). Moreover, there is a progressive and significant emergence of anti-HMGB1 antibodies during the course of the disease, mostly in patients who survived.
Conclusions
This study shows that autoantibodies to HMGB1 are produced during sepsis and are associated with a favorable outcome in patients undergoing septic shock.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
High mobility group box 1 (HMGB1) was initially identified as a conserved, abundant and ubiquitous chromatin-associated protein. In the nucleus, HMGB1 acts as an architectural factor and contributes to transcription, DNA replication, recombination and repair [1]. An increasing body of evidences supports that HMGB1 is also active out of the cell. Notably HMGB1 emerged progressively as a central player in the signalization and coordination of both septic and aseptic forms of inflammation [2, 3]. HMGB1 can be actively secreted from activated immune cells, or released during necrosis, autophagy and some forms of apoptosis [4–6]. Out of the cell, HMGB1 can bind to several receptors, including RAGE, TLR2, TLR4 and TLR9, which impacts many aspects of the cell behavior, such as proliferation, migration, differentiation, maturation and/or cytokine release [7–9]. The contribution of HMGB1 to septic inflammation was first described in an experimental mouse model of endotoxemia [10]. Thereafter, HMGB1's contribution to severe sepsis and septic shock has been investigated in detail both in animal models and in humans. Two sets of evidence indicate that HMGB1 plays a central role in sepsis and related conditions. First, HMGB1 concentration is significantly elevated in the serum of mice exposed to experimental endotoxemia or sepsis, as well as in sepsis-related conditions in humans [11–13]. Second, therapeutic agents that inhibit HMGB1 release and/or its activities, such as neutralizing antibodies, can rescue animals from severe sepsis [2].
Previous work by Gibot and colleagues [13] investigated the time course of HMGB1 in the plasma of septic shock patients admitted into an intensive care unit (ICU) and its relationship with severity of the disease and outcome. This work led to the conclusion that measurement of circulating HMGB1 could not predict outcome, although HMGB1 plasma concentrations correlated well with the degree of organ dysfunction. The same cohort of patients was used herein to investigate the presence and evaluate the predictive value of natural antibodies directed against HMGB1. Indeed, we postulated that natural antibodies could possibly modulate the normal activity of cytokines such as HMGB1. Although anti-cytokines antibodies have been detected in patients with chronic inflammatory diseases, they have also been detected in most healthy donors under the form of cytokine-autoantibodies complexes [14]. In addition, anti-cytokine antibodies have been transiently detected following viral, bacterial or parasitic infections [15]. All together, these observations led us to speculate that septic shock could stimulate the production of autoantibodies against HMGB1 that may in turn influence clinical outcome.
Patients and methods
Study population
Between February and June 2006, 42 patients admitted with a septic shock into a medical intensive care unit (ICU) of a teaching hospital (Nancy, France) were enrolled. The diagnosis of septic shock was established on the basis of the current definition. Patients were not enrolled if they were over 80 years of age or were immunocompromised. Upon admission into the ICU several items were recorded: age, gender, Simplified Acute Physiology Score II (SAPS), Sequential Organ Failure Assessment (SOFA) score, vital signs, respiratory variables, routine blood tests and microbial culture results. Outcome was assessed during a 90-day follow-up period.
These patients have already been described in detail previously [13], and their main clinical and biological features are summarized in Table 1. The present study focused on 40 of these 42 critically ill patients. Approval of the institutional review board and informed consent were obtained from patients or their relatives before inclusion.
Data collection
Day 1 was defined as the day of admission into the ICU. Within 12 h after admission and enrollment in the study, 5 ml of whole heparinized blood was drawn via an arterial catheter. Repeated sampling was performed longitudinally during the ICU stay. In this work 178 plasma samples collected from 40 patients were studied. The control group used to establish baseline values for ELISA was composed of 132 plasma samples collected from apparently healthy adult donors who were not matched with critically ill patients.
Antibody detection by ELISA
Human HMGB1 (rhHMGB1) recombinant protein was purified from Escherichia coli BL21 (DE3) pLysS strain transformed with pET15b-6His-HMGB1. Protein expression and purification were performed as previously described [16]. A commercial human serum albumin (HSA) protein (Sigma-Aldrich) was used in this study.
Maxisorp polystyrene 96-well plates were coated with 50 μl per well rHMGB1, or HSA at 2 μg/ml or 1.7 μg/ml, respectively, in 8 M urea pH 8, and incubated overnight at 4°C. The plates were blocked with 10% milk in PBS-Tween 20 0.2% for 1 h. Plasma samples, diluted 1:10 in blocking buffer, were added in duplicates (100 μl/well) and incubated for 1 h at 37°C. After four washes, 100 μl of rabbit anti-human IgG-horseradish peroxidase (HRP) (Rockland 209-4302), diluted at 1:1.000, was added to each well and incubated for 1 h at 37°C. Detection was achieved by addition of 100 μl of ABTS (Roche Diagnostic) per well and incubated at 37°C for 20 min. Optical densities (OD) were measured at 405 nm, and background levels were measured on wells in which plasma was omitted. Cutoff values were established for each antigen on 100 sera from apparently healthy people. They were calculated as the mean background OD value plus three standard deviations. The mean OD cutoff values were 0.16 and 0.2 for HSA and HMGB1, respectively. OD ratios were defined as the ratio of the OD measured for a given sample over the cutoff OD value.
Statistical analyses
Descriptive results of continuous variables are expressed as mean (±SD). Non-normally distributed values are reported as median (interquartile range, IQR) and compared using the Mann-Whitney U test. The log-rank test and Kaplan-Meier estimator were used for survival analyses. p < 0.05 was estimated statistically significant.
Results
Prevalence of anti-HMGB1 natural antibodies in apparently healthy adults and in septic shock patients
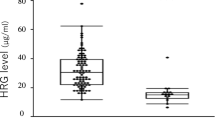
Although circulating HMGB1 is frequently elevated in septic shock patients, previous work by Gibot et al. suggested that HMGB1 plasma concentrations, as measured by commercial ELISA, only poorly correlate with outcome [13]. This led us to speculate that HMGB1 biological activities might be modulated by natural antibodies that would arise during sepsis. To test this assumption, we designed an ELISA using a recombinant form of human HMGB1 as an antigen. An ELISA was also performed with another abundant self-antigen, the human serum albumin (HSA), to evaluate the specificity of the detected antibodies. HSA was used as a control antigen since it shares several properties with HMGB1. Notably, HSA is abundantly expressed, and natural antibodies to HSA have previously been described in healthy individuals [17]. Plasma samples from 132 apparently healthy individuals were used to estimate the average level of natural IgG antibodies against these proteins in the normal adult population and to establish positive cutoff OD values (see “Patients and Methods”). IgGs to HSA and HMGB1 were detected in 3 and 15% of the samples, respectively, when plasma was diluted 1:10. No samples scored positive for higher plasma dilution, indicating that these antibodies have a low titer when present. The average values for the OD ratios were 0.6 (SD = 0.2; minimum = 0.3; maximum = 1.6) for anti-HSA and 0.9 (SD = 0.6; minimum = 0.4; maximum = 5.5) for anti-HMGB1. Then we conducted a similar study on 178 plasma samples collected sequentially from 40 septic shock patients. This cohort has been described in detail previously [15]. The main clinical and biological characteristics of these patients are summarized in the Table 1. IgGs to HSA or HMGB1 were detected in 17 and 15% of the 178 plasma samples, respectively. The average values for the OD ratios were 0.9 (SD = 1.0; minimum = 0.3; maximum = 6.2) for anti-HSA and 0.9 (SD = 1.1; minimum = 0.3; maximum = 8.1) for anti-HMGB1. Overall, IgGs to HMGB1 were detected at least once during the course of the disease in 15 patients (37.5%), whereas IgG directed against HSA was detected at least once in 8 patients (20%).
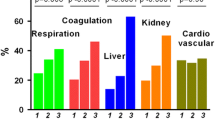
Prevalence of anti-HMGB1 natural antibodies and survival
Next, we wondered whether the presence of IgGs to HMGB1 could predict clinical outcome. As illustrated in Fig. 1, the prevalence of anti-HMGB1 antibodies was significantly higher in the patients who survived (55%) compared to the patients who did not (20%) (χ2 test, p < 0.0001). Conversely, anti-HSA antibodies were detected in 15 and 25% of the survivors and non-survivors, respectively, without any significant difference (χ2 test, p = 0.21; Fig. 1). Accordingly the detection of anti-HMGB1 antibodies during the course of the disease was significantly associated with patient survival (log rank test, p = 0.038), whereas the presence of IgGs to HSA was not (log-rank test, p = 0.645; Fig. 2). It is noteworthy that survival curves significantly differ from day 7 upwards. Therefore, we concluded that detection of anti-HMGB1 was both specific and highly predictive of clinical outcome in patients with septic shock. Strikingly, anti-HMGB1 antibodies were absent in most patients at day 1 and appeared gradually during the course of the disease, mostly in patients who survived (Fig. 3). Anti-HSA IgGs also appeared in a dynamic manner, but no significant difference was observed between survivors and non-survivors.
All together, our study showed for the first time that IgGs to HMGB1 are predictive of a favorable outcome during septic shock.
Discussion
In sepsis-related conditions, HMGB1 plasma concentrations are usually higher and persist longer in patients who succumb to the disease than in patients who survive, although some noticeable exceptions have been reported [12, 13, 18, 19]. Thus, it is tempting to assume that some biological processes may control HMGB1 plasma concentrations and/or activities in patients who survive. Since passive immunizations against HMGB1 improve outcome in experimental animal models of sepsis or endotoxemia, we hypothesized that natural antibodies to HMGB1 could improve clinical outcome of septic shock patients as well. Here we showed that IgGs to HMGB1 were detectable in 15 of 40 (37%) critically ill patients during severe sepsis, whereas they are present in about 15% of healthy adult blood donors. In both instances, these antibodies were present at a low but significant titer, which may limit their detection. This immune response was rather specific since anti-HMGB1 and anti-HSA IgG titers measured by ELISA correlate only poorly (Spearman’s rank correlation coefficient <0.5). So far, we have been unable to detect IgM in either HSA or HMGB1 in the same samples (data not shown). Autoantibodies against TNF-α, another key modulator in sepsis, have been detected in almost 40% of apparently healthy donors, a prevalence that reaches 66% in patients with gram-negative septicemia [20]. We showed here that anti-HMGB1 and anti-HSA antibodies are produced transiently in most cases during the course of the disease. This is reminiscent of the transient secretion of neutralizing IgG directed against IFN-γ and TNF-α that has been reported in an experimental model of self-limited meningitides associated with Haemophilus influenza inoculation [15]. Whether or not antibodies to other pro-inflammatory cytokines were also present in our patients and contribute to favorable outcome would deserve further investigation.
In 13 out of 15 patients, antibodies to HMGB1 were detected in one or several samples at a significant but low level, which hampered their purification and subsequent characterization. Evaluating their ability to neutralize active forms of HMGB1 in functional assays will be a major challenge to assess the exact contribution of anti-HMGB1 to patients’ recovery. Nonetheless, we have been able to purify IgGs from several plasma samples from two patients who exhibited high anti-HMGB1 titers. As both patients survived and maintained low levels of circulating HMGB1 during the course of the disease, we speculated that these antibodies could form inactive complexes with HMGB1 and/or degrade it. Indeed, recent work identified catalytic antibodies directed against key coagulation factors and endowed with serine protease activity in septic patients. This enzymatic activity was significantly higher in surviving patients, providing the first evidence that catalytic antibodies could modulate recovery in septic patients [21]. In these two patients, we could demonstrate that purified IgGs could degrade HMGB1 in vitro, although we have not yet characterized the biochemical process that was involved (data not shown). Additional experiments will be required to investigate anti-HMGB1 catalytic activity in patients secreting low amounts of anti-HMGB1 antibodies as well.
So far, we observed a poor correlation only between the presence of anti-HMGB1 IgGs and the levels of HMGB1 in the plasma of septic shock patients (data not shown). This raises many questions concerning the ability of the current commercial ELISA to quantify plasma HMGB1 precisely when bound to circulating antibodies, as already discussed by others [22]. Ongoing experiments in our laboratory clearly demonstrated that this commercial ELISA was indeed unable to detect HMGB1 when bound with known partners, including LPS or specific antibodies (S. Barnay-Verdier, personal communication). Technical improvement will therefore be required to measure HMGB1 and anti-HMGB1 relative levels precisely.
Although there are still many questions regarding the genesis and biological activities of anti-HMGB1 antibodies, the present study highlights their significant potential, in addition to plasma HMGB1, for the monitoring of sepsis-related conditions.
References
Stros M (2010) HMGB proteins: interactions with DNA and chromatin. Biochim Biophys Acta 1799:101–113
Yang H, Tracey KJ (2009) Targeting HMGB1 in inflammation. Biochim Biophys Acta 1799:149–156
Bianchi ME (2009) HMGB1 loves company. J Leuk Biol 86:573–576
Scaffidi P, Misteli T, Bianchi ME (2002) Release of chromatin protein HMGB1 by necrotic cells triggers inflammation. Nature 418:191–195
Thorburn J, Horita H, Redzic J, Hansen K, Frankel AE, Thorburn A (2009) Autophagy regulates selective HMGB1 release in tumor cells that are destined to die. Cell Death Differ 16:175–183
Bell CW, Jiang W, Reich CF 3rd, Pisetsky DS (2006) The extracellular release of HMGB1 during apoptotic cell death. Am J Physiol Cell Physiol 291:C1318–C1325
Rauvala H, Rouhiainen A (2010) Physiological and pathophysiological outcomes of the interactions of HMGB1 with cell surface receptors. Biochim Biophys Acta 1799:164–170
Tsung A, Klune JR, Zhang X, Jeyabian G, Cao Z, Peng X, Stolz Geller DA, Rosengart MR, Billiar TR (2007) HMGB1 release induced by liver ischemia involves toll-like receptor 4 dependent reactive oxygen species production and calcium-mediated signaling. J Exp Med 204:2913–2923
Yu M, Wang H, Ding A, Golenbock DT, Latz E, Czura CJ, Fenton MJ, Tracey KJ, Yang H (2006) HMGB1 signals through toll-like recpetor (TLR) 4 and TLR2. Shock 26:174–179
Wang H, Bloom O, Zhang M, Vishnubhakat JM, Ombrellino M, Che J, Frazier A, Yang H, Ivanova S, Borovikova L, Manogue KR, Faist E, Abraham E, Andersson J, Andersson U, Molina PE, Abumrad NN, Sama A, Tracey KJ (1999) HMG-1 as a late mediator of endotoxin lethality in mice. Science 285:248–251
Ueno H, Matsuda T, Hashimoto S, Amaya F, Kitamura Y, Tanaka M, Kobayashi A, Maruyama I, Yamada S, Hasegawa N, Soejima J, Koh H, Ishizaka A (2004) Contributions of high mobility group box protein in experimental and clinical acute lung injury. Am J Respir Crit Care Med 170:1310–1316
Sunden-Cullberg J, Norrby-Teglund A, Rouhiainen A, Rauvala H, Herman G, Tracey KJ, Lee ML, Andersson J, Tokics L, Treutiger CJ (2005) Persistent elevation of high mobility group box-1 protein (HMGB1) in patients with severe sepsis and septic shock. Crit Care Med 33:564–573
Gibot S, Massin F, Cravoisy A, Barraud D, Nace L, Levy B, Bollaert PE (2007) High-mobility group box 1 protein plasma concentrations during septic shock. Intensive Care Med 33:1347–1353
Watanabe M, Uchida K, Nakagaki K, Kanazawa H, Trapnell BC, Hoshino Y, Kagamu H, Yoshizawa H, Keicho N, Goto H, Nakata K (2007) Anti-cytokine autoantibodies are ubiquitous in healthy individuals. FEBS Lett 581:2017–2021
Bakhiet M, Diab A, Mahamustafa Jiezhu, Lindqvist L, Link H (1997) Potential role of autoantibodies in the regulation of cytokine responses during bacterial infections. Infect Immun 65:3300–3303
Thierry S, Gozlan J, Jaulmes A, Boniface R, Nasreddine N, Strauss F, Marechal V (2007) High-mobility group box 1 protein induces HIV-1 expression from persistently infected cells. AIDS 21:283–292
Avrameas S, Guilbert B, Dighiero G (1981) Natural antibodies against tubulin, actin myoglobin, thyroglobulin, fetuin, albumin and transferrin are present in normal human sera, and monoclonal immunoglobulins from multiple myeloma and Waldenström’s macroglobulinemia may express similar antibody specificities. Ann Immunol (Paris) 132C:231–236
Angus DC, Yang L, Kong L, Kellum JA, Delude RL, Tracey KJ, Weissfeld L (2007) Circulating high-mobility group box 1 (HMGB1) concentrations are elevated in both uncomplicated pneumonia and pneumonia with severe sepsis. Crit Care Med 35:1061–1067
Karlsson S, Pettila V, Tenhunen J, Laru-Sompa R, Hynninen M, Ruokonen E (2008) HMGB1 as a predictor of organ dysfunction and outcome in patients with severe sepsis. Intensive Care Med 34:1046–1053
Fomsgaard A, Zhang GH, Shand GH, Bendtzen K, Baek L (1989) Immunochemical and biological reactivity of human anti-lipopolysaccharide IgG obtained by screening of blood donors. Scand J Immunol 29:309–316
Lacroix-Desmazes S, Bayry J, Kaveri SV, Hayon-Sonsino D, Thorenoor N, Charpentier J, Luyt CE, Mira JP, Nagaraja V, Kazatchkine MD, Dhainaut JF, Mallet VO (2005) High levels of catalytic antibodies correlate with favorable outcome in sepsis. Proc Natl Acad Sci USA 102:4109–4113
Urbonaviciute V, Furnrohr BG, Weber C, Haslbeck M, Wilhelm S, Herrmann M, Voll RE (2007) Factors masking HMGB1 in human serum and plasma. J Leuk Biol 81:67–74
Acknowlegdments
CB received a PhD fellowship from the Ministère de l’Enseignement Supérieur et de la Recherche français, from the Réseau Herpesvirus et Cancer and from La Ligue contre le Cancer. SBV is indebted to Mélanie Messmer for her helpful discussions and constant support. The authors are grateful to Dr. Joel Gozlan for comments and fruitful discussions.
Conflict of interest
All authors certify that there is no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
V. Maréchal and S. Gibot share the seniorship position.
Rights and permissions
About this article
Cite this article
Barnay-Verdier, S., Fattoum, L., Borde, C. et al. Emergence of autoantibodies to HMGB1 is associated with survival in patients with septic shock. Intensive Care Med 37, 957–962 (2011). https://doi.org/10.1007/s00134-011-2192-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-011-2192-6