Abstract
Background
We determined the effects of two antibiotic policies (predominance of either β-lactam antibiotics or fluroquinolones) on acquisition with third-generation cephalosporin-resistant Enterobacteriaceae (CRE) and fluoroquinolone-resistant CRE (FCRE) in two ICUs, with monitoring of other variables that may influence acquisition.
Methods
After an 8-month baseline period, units were randomized to a predominant β-lactam antibiotic regimen (weekly cycling of ceftriaxone, amoxicillin–clavulanic acid and fluroquinolones) or a fluoroquinolone regimen for 3 months, with cross-over for another 3 months. Acquisition of CRE and FCRE was determined by microbiological surveillance.
Results
During baseline, acquisition rates for CRE and FCRE were 14/1,000 and 2/1,000 patient days at risk, respectively. Cross-transmission of CRE accounted for ≤25% of acquisitions, and CRE acquisition was associated with the use of β-lactam antibiotics (amoxicillin–clavulanic acid in particular). As compared to baseline, β-lactam antibiotic use [in defined daily dose (DDD)/1,000 patient days] was reduced from 854 to 526 (−39%) and 555 (−35%) during both intervention periods. Fluoroquinolone use was increased from 150 and 129 DDD/1,000 patient days in baseline and the β-lactam period to 514 DDD/1,000 patient days (+243%) in the fluoroquinolone period. Reductions in β-lactam use were not associated with reduced CRE acquisition [adjusted HRs were 1.0 (95% CR: 0.5–2.2) and 1.1 (95% CI: 0.5–2.5) during both periods, respectively]. Increased use of fluoroquinolones was associated with increased acquisition of FCRE [adjusted HR 4.1 (95% CI: 1.4–11.9; p < 0.01]. Infection control variables remained comparable during all periods.
Conclusion
A 35–39% reduction of β-lactam exposure was not associated with reduced acquisition of CRE, whereas a 243% increase of fluoroquinolone use increased acquisition of FCRE.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Antimicrobial resistance is a serious and continuously increasing threat to patient treatment worldwide. It is obvious that antibiotic exposure contributes to the emergence and spread of resistant pathogens, both in hospitals and the community at large [1, 2]. Within intensive care units (ICU) patients are frequently colonized with antibiotic-resistant bacteria. Conversion of the colonization status (i.e., from non-colonized to colonized) may occur through (1) de novo resistance development in previously susceptible bacteria, (2) antibiotic-induced selection of previously present, though undetectable, resistant bacteria or (3) through patient-to-patient transmission of pathogens (i.e., cross-transmission) [3]. Cross-transmission is a multi-factorial process and depends on patient characteristics, contact rates, staffing and cohorting levels of health-care workers (HCW), adherence to hand hygiene, antibiotic use and colonization pressure (i.e., proportion of patients colonized) [4]. The typically small ICU patient populations (10–20 patients) and rapid turnover create continuous fluctuation of the prevalence of resistant pathogens, hampering straightforward analysis of interventions [5].
Data on the effects of modulation of antibiotic policies on antibiotic resistance levels in ICUs are conflicting. Antibiotic cycling has been advocated by some [6–8], but positive findings were not confirmed in other studies [9, 10]. Importantly, confounding by unmeasured, but potentially relevant, variables was not excluded in any of these studies [5]. Therefore, we evaluated the effects of a single antibiotic intervention on acquisition of colonization with third-generation cephalosporin-resistant Enterobacteriaceae (CRE) in two ICUs. These bacteria were chosen pragmatically, as prevalence rates of other important antibiotic-resistant bacteria (i.e., methicillin-resistant Staphylococcus aureus, vancomyin-resistant enterococci, extended-spectrum β-lactamase producing Enterobacteriaceae or carbapenem-resistant P. aueruginosa or Acinetobacter species) were very low and because an easy screening method was available. In a baseline period, CRE acquisition appeared to be predominantly of endogenous origin (i.e., de novo resistance development or selection) with the use of β-lactam antibiotics (amoxicillin–clavulanic acid in particular) as a risk factor. Therefore, a reduction of β-lactam use was pursued with a homogeneous (fluoroquinolones) antibiotic regimen, which was compared to a cycling strategy (amoxicillin–clavulanic acid, ceftriaxone and levofloxacin) in a randomized crossover study.
Patients and methods
Setting and study design
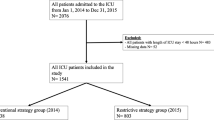
This study was conducted in two ICUs, a medical (MICU) and neurosurgical ICU (NSICU), of the University Medical Centre Utrecht, The Netherlands. The MICU has ten beds, of which four are in separate rooms, and is situated in the hospitals’ basement. The NSICU has eight beds, one in a separate room, and is situated on the fourth floor. Medical and nursing staffs are not shared between both ICUs.
During a baseline period of 8 months (9 September 2001 through 13 May 2002), colonization dynamics of CRE were analyzed by means of microbiological surveillance and genotyping, collection of demographical and clinical data, and monitoring of infection control practices. Based on the epidemiological findings obtained during baseline (i.e., relative importance of acquisition routes and risk factors for acquisition), an intervention was designed to reduce the acquisition rate of CRE.
In a crossover design, reduction of β-lactam antibiotic exposure (most notably amoxicillin–clavulanic acid and ceftriaxone) was pursued by applying a homogeneous (3 months) antibiotic policy for empirical treatment. This strategy was compared to a cycling (3 months) period, in which the first choice antibiotic for empirical therapy changed weekly from ceftriaxone in the 1st week, to amoxicillin–clavulanic acid in the 2nd week, to levofloxacin or ciprofloxacin in the 3rd week, and back to ceftriaxone in the 4th week, and so on. For individual patients, antibiotics started, according to the weekly schedule, were not adjusted when the weekly schedule changed. During the homogenous regimen, levofloxacin or ciprofloxacin was the first choice of empirical therapy. The MICU was randomized to start with the cycling regimen and the NSICU with the homogeneous regimen. There were no wash-in/wash-out periods between different study periods.
This study was approved by the institutional review board, which waived the need of informed consent.
Data collection and microbiological surveillance
All patients admitted were included, and age, gender, APACHE II score and admission indication were recorded on admission. Antibiotic use was monitored throughout the patients’ ICU stays. Collection of all variables (demographics, antibiotic use, infection control measures and microbiological data) was similar in all three study periods.
Colonization with CRE was determined by means of rectal swabs taken on admission and twice weekly thereafter, plated on Chromogenic UTI agar plates (Oxoid Limited, Basingstoke, UK) supplemented with 8 μg/ml cefpodoxime and 6 μg/ml vancomycin. Species identification of every morphological distinct colony was performed using VITEK II (bioMérieux, Lyon, France). Resistance to third-generation cephalosporins was then confirmed by determination of the MIC values for cefpodoxime and ceftazidime using Micronaut-S β-lactamase III (Merlin Diagnostika GMBH, Bornheim-Hersel, Germany). Isolates not resistant to either cefpodoxime or ceftazidime, according to NCCLS guidelines [11], were considered susceptible in further analyses. In addition, susceptibility of CRE isolates to ciprofloxacin was determined using microdilution susceptibility testing according to NCCLS guidelines [11].
Colonization on admission was defined as colonization within the first 48 h after ICU admission. Acquired colonization was defined as colonization after 48 h of ICU admission after a previous negative culture. The primary end-point of analysis was number of acquisitions per 1,000 patient days at risk (i.e., CRE acquisition rate).
Cross-transmission was defined as acquired colonization with genotypically related strains in epidemiologically linked patients. CRE acquisitions not fulfilling this definition were considered endogenous acquisition, i.e., selection of pre-existing flora or de novo resistance development. Epidemiological linkage was defined as two patients having an overlap in ICU stay. Because of the possibility of low-level colonization directly after acquisition, a maximum time window (between discharge and admission of “donor” and “acceptor” patients) of 7 days was accepted [12]. CRE isolates were genotyped by means of amplified fragment-length polymorphism (AFLP) [13], and 80% similarity was used as the cutoff point for genetic relatedness. Results of surveillance cultures and genotyping were not available for the hospitals’ infection control department or ICU physicians.
Infection control practices
Observations of patients and nurses were used to determine contact rates, cohorting levels of nursing staff and adherence to hand hygiene. Cohorting is defined as the likelihood that after a previous contact, the next contact of a health-care worker (HCW) is with the same patient [14]. Observations were performed by trained infection control nurses, according to predetermined schedules (unknown to the ICU staff), and were evenly distributed between 7 a.m. and 11 p.m. Two types of observations were performed—nurse-oriented and patient-oriented observations—to calculate contact rates, cohorting of nursing staff and adherence to hand hygiene. Nurses were observed for 20 min, during which the number of contacts and number of contacted patients (nurse-patient contacts) were recorded, in order to calculate contact rates and level of cohorting. Patients were also observed for 20 min, during which number of contacts (HCW–patient contacts), type of health-care worker (physician, nurse, physical therapist, radiology assistant), type of contact, use and removal of gloves, and use and type of hand hygiene were recorded, in order to determine contact rates and adherence to hand hygiene.
A patient contact was defined as any contact with a patients’ skin or gown, irrespective of the duration or intensity of contact. Contacts with other inanimate objects were considered environmental. Gloves needed to be removed and hand hygiene to be used before returning to the communal environment of the ICU. Appropriate hand hygiene was considered to be either washing hands with soap and water or use of an alcoholic hand rub. Both ICUs are provided with two sinks with both soap and alcohol hand rub dispensers, with each bedside also having its own alcohol hand rub dispenser.
Statistical and risk factor analysis
Continuous variables were analysed by Student’s t test or Mann–Whitney U test and categorical variables by χ2 statistics. Acquisition rates (events per 1,000 patient days at risk) were compared using a multivariate Cox proportional hazard model, which controls for the time at risk, with subsequent addition of potential confounders (all variables with p < 0.10). The model calculates hazard ratios (HR) and 95% confidence intervals. All analyses were performed with SPSS software (SPSS Inc., Chicago, IL).
Results
Baseline
Patient characteristics, CRE colonization and infection control
All analyses of the baseline period were performed separately for both ICUs. As no relevant differences (apart from patient characteristics) were obtained, the combined data of both wards are presented. During the 8-month baseline period, 457 patients were admitted from which 1,243 cultures were obtained (Table 1). Thirty-three patients (7.2%; 23 in MICU and 10 in NSICU) were colonized with CRE on admission, and 44 patients (9.6%; 23 in MICU and 21 in MSICU) acquired colonization during their stay in the ICU (Table 2). Origin of colonization (i.e., present on admission or acquired) could not be determined for six patients, because cultures were either taken more than 48 h after admission or patients had been admitted before the start of the study period. The CRE acquisition rate was 14/1,000 patient days at risk with a mean time to acquisition of 7 days (Table 2). Based on epidemiological linkage and genotyping, CRE colonization was predominantly acquired endogenously: 11 of 44 (25%) cases of acquired colonization [5 of 23 in MICU (21.7%) and 6 of 21 in NSICU (28.6%)] resulted from cross-transmission. Therefore, the endogenous route was considered the dominant route for acquired colonization. Of all patients colonized with CRE (n = 83), 16 (19%) were colonized with a fluoroquinolone-resistant isolate (FCRE): 9 on admission and 6 after acquisition of FCRE in the ICU after a mean of 7 ± 10 days. The acquisition rate of FCRE was 2.1/1,000 patient days.
In total, 352 nurse-patient contacts (nurse observations) and 435 HCW–patient contacts (patient observations) were observed during 197 h (Table 3). Nurses had 3.2 ± 1.3 patient contacts/h, and their level of cohorting was 71% ± 22%. Patients received 4.0 ± 1.8 contacts/h from HCW (nurses, physicians, radiology technicians, physical therapists). Adherence to hand hygiene after patient contact was 55% overall, 59% for physicians and 53% for nurses (p = 0.399) (Table 3).
Risk factors for acquisition with CRE during baseline
In univariate analysis, CRE acquisition was associated with a pulmonary admission indication, trauma, admission after surgery and admission for “other” indications (Table 4). Furthermore, all patients acquiring CRE had received antibiotics, as compared to 63% of non-affected patients (p < 0.01). Amoxicillin–clavulanic acid and aminoglycosides were associated with CRE acquisition. ICU ward, APACHE II score, patient-specific contact rates and hand hygiene were not associated with CRE acquisition. For this analysis, hand hygiene and contact rates were calculated on the patient-level instead of using the means of each period. In multivariate analysis, admission because of trauma remained independently associated with CRE acquisition [hazard ratio (HR): 2.7, CI: 1.1–6.6].
In summary, acquired colonization with CRE predominantly occurred endogenously (75% of acquisitions), and amoxicillin–clavulanic acid and ceftriaxone accounted for 62% of antibiotic exposure. Based upon this finding and reported associations of β-lactam use and acquisition of gram-negatives resistant to these antibiotics [15, 16], we hypothesized that reducing β-lactam antibiotic use would decrease CRE acquisition rates.
Intervention period
During the intervention periods, patient characteristics were comparable to baseline (Table 1). Again, all analyses were performed first for both ICUs separately with similar results (data not shown). As there were no relevant demographic differences between the wards (apart from indication of admission) and intervention effects were comparable, data are combined. In all, 421 and 376 cultures were obtained during the heterogeneous and homogeneous period, respectively. Percentages of patients colonized on admission with CRE or FCRE were comparable in all three study periods (Table 2).
Antibiotic use
As compared to baseline, overall usage of antibiotics did not change (Table 5). During baseline 67% of all patients received antibiotics, as compared to 61 and 72% during cycling and homogeneous study periods, respectively (p = 0.12 and p = 0.33; data not shown). Yet, amoxicillin–clavulanic acid use decreased from 37% of all patients in baseline to 21% (p < 0.01) and 16% (p < 0.01) during cycling and homogeneous periods, respectively. Expressed in DDD/1,000 patient days, use of amoxicillin–clavulanic acid was reduced from 326 in baseline, to 131 in the cycling and 31 in the homogeneous period, respectively. Ceftriaxone use during the cycling regimen (19%, 130 DDD/1,000 patient days) was comparable to baseline (17%, 134 DDD/1,000 patient days), but decreased to 10% of all patients (55 DDD/1,000 patient days) during the homogeneous regimen (p < 0.01). Naturally, other β-lactam antibiotics (i.e., ceftazidime, piperacillin–tazobactam and carbapenems) were needed for specific treatment indications, and their need increased by 19% during the homogeneous period. Therefore, total use of β-lactam antibiotics was reduced by 39 and 35% in the cycling and homogeneous periods, respectively. Fluoroquinolone use slightly decreased in the cycling period (150 vs 129 DDD/1,000 patient days in the baseline and heterogeneous period, respectively), although proportions of patients being exposed slightly increased (from 8% during baseline to 13% in the heterogeneous period (p = 0.07). In the homogeneous period, 51% of all patients received fluorquinolones, yielding a total exposure of 514 DDD/1,000 patient days (+243% as compared to baseline).
Infection control
Contact rates received by patients were lowest during the cycling period, 2.9 ± 1.3, as compared to 4.0 ± 1.8 (p = 0.01) during baseline and 4.3 ± 2.5 (p = 0.02) during the homogeneous period (Table 3). The contact rates of nurses were also lowest during the cycling period: 2.5 ± 1.0, as compared to 3.2 ± 1.3 (p = 0.02) during baseline and 2.8 ± 1.4 (p = 0.28) during the homogeneous period. Adherence to hand hygiene and cohorting levels were comparable during all three study periods.
Acquisition rates
Acquisition rates of CRE were 14/1,000 and 18/1,000 patient days at risk during the cycling and homogenous period, respectively (as compared to 14/1,000 patient days at risk in baseline). In a Cox proportional hazards model (using baseline as reference), with adjustment for ICU, age, APACHE II score, admission indication and contact rates, acquisition was comparable in all three study periods (adjusted HR: 1.0, 95% CI: 0.5–2.2; p = 0.95 for the cycling regimen and adjusted HR: 1.1, 95% CI: 0.5–2.5; p = 0.69 for the homogeneous regimens).
Acquisition rates FCRE were 2.1 and 2.5/1,000 patient days at risk in the baseline and cycling period, respectively, and increased to 8.3/1,000 patient days at risk during the homogeneous period. The adjusted HR (using the same variables for adjustment) was 4.1 (95% CI: 1.4–11.9; p < 0.01). Seventeen patients acquired colonization with FCRE. Five patients had acquired isolates that were genotypically related and epidemiologically linked to those of other patients (one during the cycling period and four during the homogeneous period). The remaining 12 patients either did not have epidemiological linkage or acquired colonization with other genotypes, and thus, acquired colonization via the endogenous route.
Discussion
In this study, we evaluated the effects of two empiric antibiotic regimens on acquisition of third-generation cephalosporin-resistant Enterobacteriaceae (CRE) and fluoroquinolone-resistant CRE (FCRE) in two ICUs. Based on the relevance of endogenous acquisition of colonization and the predominant use of amoxicillin–clavulanic acid and ceftriaxone use (62% of total antibiotic use) in a baseline period, a step-wise reduction of amoxicillin–clavulanic acid use (of 60 and 91%) and ceftriaxone use (of 3 and 59%), at the costs of increased usage of fluoroquinolones (+243% in the homogeneous period), failed to reduce CRE acquisition, but significantly increased acquisition of FCRE.
A strength of our study is that it is the first to use prospective surveillance of colonization, large-scale genotyping, a baseline period to determine colonization dynamics and accurate monitoring of multiple variables that might influence colonization dynamics. Although AFLP is not the most widely used genotyping method, it has similar discriminatory power as pulsed-field gel-electrophoresis and multi-locus sequence typing for both gram-positive and gram-negative bacteria [17, 18]. As only few studies have monitored antibiotic use in DDD/1,000 patient days, contact rates, cohorting levels and adherence to hand hygiene, comparison to other ICUs is difficult.
Total antibiotic use in our ICUs (1,380 DDD/1,000 patient days in our ICU) was comparable to German ICUs (on average 1,332 DDD/1,000 patient days) participating in the project Surveillance of Antimicrobial Use and Antimicrobial Resistance in ICUs (SARI) [19]. And distribution of antibiotic classes in our setting corresponded to the average of 53 ICUs in non-university acute care hospitals in Southern Germany, where beta-lactams and fluoroquinolones accounted for 59 and 11% of total use (61 and 8% in our ICUs) [20].
In our study the number of contacts received by an individual patient per hour ranged from 0 to 9 contacts/h, which would yield 0–72 contacts/h unit-wide with 100% occupancy. This is similar to contact rates reported by others [21, 22]. Slightly lower (15/h for a whole ICU)) and higher (6.6/patient/h) contact rates, though, have been reported as well [23, 24]. Reported cohorting levels of nurses in ICUs have ranged from 70 to 77% [21, 24, 25], which is fairly similar to the 71–74% that we observed. Most information is available on adherence to hand hygiene. Using different monitoring strategies, reported adherence rates in ICUs have ranged from 12 to 81%, but usually do not exceed 50% [26, 27]. Although still not optimal, adherence rates, as observed in our study, appeared to be above average, which might explain the low incidence of cross-transmission in the baseline period. For all these reasons, we consider our units as rather generalizable with regard to antibiotic use and infection control practices.
There are also several limitations of our study that must be addressed. The first limitation is related to the complexity of patient care in ICUs. With all efforts, we were only able to reduce overall β-lactam antibiotic use by 35–39%. These antibiotics are considered optimal treatment for many indications, and need for them of course overruled the study protocol. Therefore, further reductions in β-lactam antibiotic exposure may not be feasible. Furthermore, for logistical reasons we only obtained rectal swabs, and not respiratory or environmental samples. Although the rectum is the most important colonization site for CRE, we may have missed some patients that were only colonized in the respiratory tract. And in contrast to, for instance, enterococci, there is no evidence that environmental contamination is important in the epidemiology of multi-resistant Enterobacteriaceae. In addition, we used intestinal colonization as endpoint, and we did not collect information on CRE infections, or any other infections. Observations for adherence to infection control measures were only performed during daytime and not in nightly hours and during weekends, and duration and intensity of contacts were not monitored. Since there were no interventions related to infection control measures, we assume that this limitation had no effects. Finally, longer intervention periods might have yielded different results. Yet, in the absence of an environmental reservoir, the ecological dynamics in an ICU are driven by patients who have a short length of stay. In fact, the study periods were long enough to document the increase in FCRE resistance. Naturally, our findings are only generalizable to ICUs using similar classes of antibiotics.
Our findings have demonstrated two important aspects of antibiotic resistance in ICUs: (1) in two settings with endemicity of resistance to β-lactam antibiotics, a straightforward reduction of exposure to this antibiotic class did not reduce prevalence levels of β-lactam resistance; (2) in the absence of endemicity of fluoroquinolone resistance, increased exposure of this antibiotic class increased fluoroquinolone resistance. These findings underscore the complexity of antibiotic resistance in ICUs and the need to apply rigorous study designs when evaluating interventions.
References
Neuhauser MM, Weinstein RA, Rydman R, Danziger LH, Karam G, Quinn JP (2003) Antibiotic resistance among gram-negative bacilli in US intensive care units: implications for fluoroquinolone use. JAMA 289:885–888
Malhotra-Kumar S, Lammens C, Coenen S, Van HK, Goossens H (2007) Effect of azithromycin and clarithromycin therapy on pharyngeal carriage of macrolide-resistant streptococci in healthy volunteers: a randomised, double-blind, placebo-controlled study. Lancet 369:482–490
Bonten MJ, Austin DJ, Lipsitch M (2001) Understanding the spread of antibiotic resistant pathogens in hospitals: mathematical models as tools for control. Clin Infect Dis 33:1739–1746
Bonten MJ, Slaughter S, Ambergen AW, Hayden MK, van Voorhis J, Nathan C, Weinstein RA (2006) The role of “colonization pressure” in the spread of vancomycin- resistant enterococci: an important infection control variable. Arch Intern Med 158:1127–1132
Nijssen S, Bootsma M, Bonten M (2000) Potential confounding in evaluating infection-control interventions in hospital settings: changing antibiotic prescription. Clin Infect Dis 43:616–623
Gruson D, Hilbert G, Vargas F, Valentino R, Bebear C, Allery A, Bebear C, Gbikpi-Benissan G, Cardinaud JP (2000) Rotation and restricted use of antibiotics in a medical intensive care unit. Am J Respir Crit Care Med 162:837–843
Martinez JA, Nicolas JM, Marco F, Horcajada JP, Garcia-Segarra G, Trilla A, Codina C, Torres A, Mensa (2006) Comparison of antimicrobial cycling and mixing strategies in two medical intensive care units. Crit Care Medicine 34:329–336
Raymond DP, Pelletier SJ, Crabtree TD, Gleason TG, Hamm LL, Pruett TL, Sawyer RG (2001) Impact of a rotating empiric antibiotic schedule on infectious mortality in an intensive care unit. Crit Care Med 29:1101–1108
Warren DK, Hill HA, Merz LR, Kollef MH, Hayden MK, Fraser VJ, Fridkin SK (2004) Cycling empirical antimicrobial agents to prevent emergence of antimicrobial-resistant Gram-negative bacteria among intensive care unit patients. Crit Care Med 32:2450–2456
van Loon HJ, Vriens MR, Fluit AC, Troelstra A, van der Werken C, Verhoef J, Bonten MJ (2005) Antibiotic rotation and development of Gram-negative antibiotic resistance. Am J Respir Crit Care Med 171:480–487
National Committee for Clinical Laboratory Standards (1999) Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically. Approved standard M7–A4. National Committee for Clinical Laboratory Standards, Wayne
Grundmann H, Barwolff S, Tami A, Behnke M, Schwab F, Geffers C, Halle E, Göbel UB, Schiller R, Jonas D, Klare I, Weist K, Witte W, Beck-Beilecke K, Schumacher M, Rüden H, Gastmeier P (2005) How many infections are caused by patient-to-patient transmission in intensive care units? Crit Care Med 33:946–951
Willems RJ, Top J, van den Braak N, van Belkum A, Endtz H, Mevius D, Stobberingh E, van Den Bogaard A, van Embden JD (2000) Host specificity of vancomycin-resistant Enterococcus faecium. J Infect Dis 182:816–823
Austin DJ, Bonten MJM, Slaughter S, Weinstein RA, Anderson RM (1999) Vancomycin-resistant enterococci in Intensive Care hospital settings: transmission dynamics, persistence and the impact of infection control programs. Proc Natl Acad Sci USA 96:6908–6913
Sandoval C, Walter SD, McGeer A, Simor AE, Bradley SF, Moss LM, Loeb MB (2004) Nursing home residents and Enterobacteriaceae resistant to third-generation cephalosporins. Emerg Infect Dis 10:1050–1055
Kim PW, Harris AD, Roghmann MC, Morris JG Jr, Strinivasan A, Perencevich EN (2003) Epidemiological risk factors for isolation of ceftriaxone-resistant versus -susceptible citrobacter freundii in hospitalized patients. Antimicrob Agents Chemother 47:2882–2887
Torpdahl M, Skov MN, Sandvang D, Baggesen DL (2005) Genotypic characterization of Salmonella by multilocus sequence typing, pulsed-field gel electrophoresis and amplified fragment length polymorphism. J Microbiol Methods 63:173–184
Melles DC, van Leeuwen WB, Snijders SV, Horst-Kreft D, Peeters JK, Verbrugh HA, van Belkum A (2007) Comparison of multilocus sequence typing (MLST), pulsed-field gel electrophoresis (PFGE), and amplified fragment length polymorphism (AFLP) for genetic typing of Staphylococcus aureus. J Microbiol Methods 69:371–375
Meyer E, Schwab F, Gastmeier P, Rueden H, Daschner FD (2006) Surveillance of antimicrobial use and antimicrobial resistance in German intensive care units (SARI): a summary of the data from 2001 through 2004. Infection 34:303–309
Kern WV, de WK, Steib-Bauert M, Fellhauer M, Plangger A, Probst W (2005) Antibiotic use in non-university regional acute care general hospitals in southwestern Germany, 2001–2002. Infection 33:333–339
Grundmann H, Hori S, Winter B, Tami A, Austin DJ (2002) Risk factors for the transmission of methicillin-resistant Staphylococcus aureus in an adult intensive care unit: fitting a model to the data. J Infect Dis 185:481–488
Pittet D, Mourouga P, Perneger TV (1999) Compliance with handwashing in a teaching hospital. Ann Intern Med 130:126–130
Kim PW, Roghmann MC, Perencevich EN, Harris AD (2003) Rates of hand disinfection associated with glove use, patient isolation, and changes between exposure to various body sites. Am J Infect Control 31:97–103
McArdle FI, Lee RJ, Gibb AP, Walsh TS (2006) How much time is needed for hand hygiene in intensive care? A prospective trained observer study of rates of contact between healthcare workers and intensive care patients. J Hosp Infect 62:304–310
Nijssen S, Bonten MJ, Franklin C, Verhoef J, Hoepelman AI, Weinstein RA (2003) Relative risk of physicians and nurses to transmit pathogens in a medical intensive care unit. Arch Intern Med 163:2785–2786
Pittet D, Allegranzi B, Sax H, Dharan S, Pessoa-Silva CL, Donaldson L, Boyce JM, WHO Global Patient Safety Challenge, World Alliance for Patient Safety (2006) Evidence-based model for hand transmission during patient care and the role of improved practices. Lancet Infect Dis 6:641–652
Pittet D, Boyce JM (2003) Revolutionising hand hygiene in health-care settings: guidelines revisited. Lancet Infect Dis 3:269–270
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Nijssen, S., Fluit, A., van de Vijver, D. et al. Effects of reducing beta-lactam antibiotic pressure on intestinal colonization of antibiotic-resistant gram-negative bacteria. Intensive Care Med 36, 512–519 (2010). https://doi.org/10.1007/s00134-009-1714-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-009-1714-y