Abstract
Objective
In sepsis, dysregulation of the immune response leads to rapid multiorgan failure and death. Accurate and timely diagnosis is lifesaving and should discriminate sepsis from the systemic inflammatory response syndrome (SIRS) caused by non-infectious agents. Osteopontin acts as an extracellular matrix component or a soluble cytokine in inflamed tissues. Its exact role in immune response and sepsis remains to be elucidated. Therefore, we investigated the role of osteopontin in SIRS and sepsis.
Design
Prospective, observational study.
Setting
Intensive care unit of a university hospital.
Patients and participants
Fifty-six patients with SIRS or sepsis and 56 healthy subjects were enrolled.
Interventions
We analyzed the serum levels of osteopontin and TH1–TH2 cytokines and investigated the role of osteopontin on interleukin 6 secretion by monocytes.
Measurements and main results
Serum osteopontin levels were strikingly higher in patients than in controls and in sepsis than in SIRS, and decreased during the resolution of both the disorders. Receiver operating characteristic curves showed that osteopontin levels have discriminative power between SIRS and sepsis with an area under the curve of 0.796. Osteopontin levels directly correlated with those of interleukin 6 and in vitro, recombinant osteopontin increased interleukin 6 secretion by monocytes in both the absence and presence of high doses of lipopolysaccharide.
Conclusion
These data suggest that osteopontin might be a mediator involved in the pathogenesis of SIRS and sepsis, possibly by supporting interleukin 6 secretion.
Descriptor
45. SIRS/Sepsis: clinical studies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sepsis is characterized by signs of systemic inflammation and its most serious forms, i.e., severe sepsis and septic shock (SS/SS), are a major cause of morbidity and mortality in intensive care unit (ICU) [1]. Sepsis must be distinguished from the non-infectious systemic inflammatory response syndrome (SIRS) induced by agents such as trauma and ischemia causing extensive tissue injury. Discrimination between SIRS and sepsis is crucial to promptly establish appropriate treatments in critically ill patients, since therapies and outcomes greatly vary in patients with and without infection [2]. Early detection of sepsis, however, is not easy and no single clinical or biological indicator has so far won unanimous acceptance.
The pathogenesis of both SIRS and sepsis is only partially defined, but a key role is ascribed to systemic inflammation with overwhelming production of several inflammatory cytokines [i.e., tumor necrosis factor (TNF)-α, interleukin (IL)1, IL6 by many cell types (monocytes, macrophages, endothelial cells)]. The pro- and anti-inflammatory phases must be coordinated to mount a balanced effective defense that is not harmful for the host. Antagonists of IL1 and TNF-α have been used to counteract systemic inflammation, but they failed to improve the outcome and even display a detrimental effect [3, 4].
Osteopontin is a phosphoprotein with adhesive and cell-signaling functions involved in cell–cell and cell–matrix interactions crucial in the inflammatory response [5, 6]. It can act as either an extracellular matrix component in mineralized tissues or a soluble cytokine in inflamed tissues and serum. The exact role of osteopontin in vivo immune responses is partly unclear since it is believed to mainly act as a pro-inflammatory cytokine by chemoattracting monocytes/macrophages and modulating T cell function, but may also have some anti-inflammatory effects since it can inhibit nitric oxide production by macrophages in vitro and support tissue repair at sites of inflammation [7, 8]. Its tissue and serum levels are increased in diseases with either systemic or focal chronic inflammation, such as Crohn’s disease [9], systemic lupus erythematosus [10], multiple sclerosis [11, 12] and tuberculosis [13], but little is known about its levels in acute inflammatory diseases [14]. Since osteopontin seems to be a key player in macrophage function and inflammation, this study investigated its levels in SIRS and sepsis to assess its involvement in the pathogenesis of these acute inflammatory diseases and its possible role as a marker of the disease status.
Materials and methods
Study population
We performed a prospective observational study on 56 consecutive patients (43 male, 13 female) admitted to the ICU of the Maggiore della Carità Hospital, Novara, Italy from May 2004 to May 2005. The study was approved by our institutional ethical committee; written informed consent was obtained from the patients or their legal representative.
Patients were enrolled when they met the criteria of SIRS or SS/SS [15]. Briefly, patients were considered to have SIRS if they met two or more of the following conditions: (1) temperature >38 or <36°C, (2) heart rate >90 beats/min, (3) respiratory rate >20 breaths/min or PaCO2 <32 mmHg, and (4) white blood cells count >12,000 or <4,000/μL, or the presence of more than 10% immature neutrophils. Patients had sepsis when they developed SIRS as a result of infection [15]. Septic patients with organ dysfunction were considered to have severe sepsis, and those with persisting hypotension, requiring vasopressor treatment, were considered to have septic shock. Clinical severity was evaluated by blood sampling with the Acute Physiology and Chronic Health Evaluation (APACHE) II and the Sequential Organ Failure Assessment (SOFA) scores by physicians blinded to the experimental results [16, 17].
The two groups consisted of 29 patients with SIRS and 27 with SS/SS. We also studied: (1) 56 healthy volunteers, defined as controls, matched for gender and age; (2) 21 patients in resolution from SIRS (14 patients) and SS/SS (7 patients). The resolution group comprised patients who no longer met the inclusion criteria of SIRS (i.e., displaying one or no inclusion criteria) [15].
Samples collection
All blood samples were obtained within 6 h after patients were enrolled and met the criteria of SIRS or SS/SS [15]. For patients analyzed during the resolution phase, blood withdrawal was performed on the first day in which they lost the inclusion criteria for SIRS. In all patients and controls, serum was preferred over plasma to overcome the possible problems related to the influence of different basal coagulation activity on osteopontin levels.
Monocytes isolation and culture
CD14+ monocytes were isolated from peripheral blood mononuclear cells by plastic adherence. To evaluate the dose-dependence of IL6 secretion, monocytes were plated at 5 × 105 cells/mL in 48 well plates, activated or not with lipopolysaccharide at 25 ng/mL (Escherichia coli, serotype 055:B5; Sigma Chemicals Co., St Louis, MO) and cultured in the presence or absence of human recombinant osteopontin (rOPN) at 0.1, 0.5 or 1 μg/mL, (R&D System, Minneapolis, MN). After 6 h, supernatants were harvested and cells were recovered for mRNA extraction. For time-course analysis, monocytes (105 cells/mL in 96 well plates), were activated with lipopolysaccharide at 25 ng/mL and supernatants were harvested after 6, 24 and 48 h. Endotoxin level in rOPN preparations, was <1.0 UE/μg of rOPN corresponding to 0.2 ng/ml. We compared IL6 secretion in monocytes (5 × 105 cells/mL in 48 well plates) treated with 0.2 ng/ml of lipopolysaccharide or rOPN (1 μg/ml) or rOPN (1 μg) plus a neutralizing α-OPN mAb (10 μg) (R&D System).
Osteopontin and IL6 ELISA assay
Serum osteopontin and IL6 concentrations were evaluated in a capture enzyme-linked immunoadsorbent assay (ELISA) according to the manufacturer’s protocol (Assay Designs Inc., Michigan; Pierce Biotechnology Inc., Rockford, IL) by investigators blinded to patient clinical condition.
T helper type (TH)1 and TH2 cytokine assay
A panel of TH1 and TH2 cytokines comprising IL2, IL4, IL5, IL10, IFN-γ, and TNF-α were simultaneously quantified by the Human TH1/TH2 Cytokine Cytometric Bead Array Kit (BD Pharmingen, San Diego, CA, USA) according to the manufacturer’s protocol, using a flow cytometer (BD Pharmingen, San Diego, CA, USA).
Real-time RT-PCR Assay
Total RNA was isolated from monocytes treated or not with different concentrations of rOPN for 6 h, using Nucleospin RNAII kit (Machery-Nagel, Germany). RNA (500 ng) was retrotrascribed by the ThermoScript™ RT PCR System (Invitrogen, Burlington, ON, Canada) and IL6 expression was determined with a commercial gene expression assay (Applied Biosystem, Foster City, CA, USA). The housekeeping gene HPRT was used to normalize for variations in cDNA. Real-time PCR was performed on 7000 Sequence Detection System (Applied Biosystem) in duplicate for each sample. The results were analyzed with a standard curve model.
Determination of necrosis and apoptosis
To estimate the level of necrosis during the time-course experiments, we evaluated the release of lactate dehydrogenase (LDH) in the supernatants after a 48 h culture, with the CytoTox-One™ Homogeneous Membrane Integrity Kit (Promega, Madison, USA) by following the manufacturer’s instruction. In the same conditions, cells were harvested and stained with trypan blue evaluating live cells.
Statistical analysis
Mann–Whitney U-test and Wilcoxon’s signed rank were used to analyze the unpaired or paired data, respectively. Comparison among groups was performed using Kruskal–Wallis test. When an overall p < 0.05, a Dunn’s multiple-comparison post hoc analysis was conducted. Correlations were tested with Spearman’s rho. A p value <0.05 was considered statistically significant. Data were analyzed by sensitivity and specificity derived from the receiver operating characteristic curve (ROC), and area under the curve (AUC) [18]. Statistical analysis was performed with GraphPad Instat (GraphPad Software, San Diego, CA, USA) software.
Results
Study population
We analyzed 29 patients with SIRS and 27 with SS/SS admitted to the ICU of the Maggiore della Carità Hospital, Novara, Italy, and 56 healthy volunteers matched for gender and age, as controls. Moreover, 21 patients were also analyzed on the first day in which they lost the inclusion criteria for SIRS [15]. Baseline clinical features of the patients and microbiological findings are summarized in Tables 1 and 2, respectively. Clinical severity was evaluated using scores calculated according to the APACHE II system [16] and the SOFA system [17]. Both the scores were significantly different in SS/SS and SIRS patients (p < 0.0001) (Table 1).
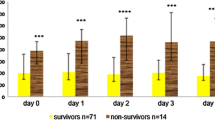
Serum osteopontin levels are elevated in patients with SIRS and SS/SS
Serum osteopontin levels were measured in patients and controls. Levels were strikingly higher in the patients (median 1,653 ng/mL) than in the controls (median 159 ng/mL, p < 0.0001) (Table 3). Moreover, they were significantly higher in SS/SS (median 2,031 ng/mL) than in SIRS (median 1,396 ng/mL, p < 0.001) (Table 3) and seemed to be associated with the clinical outcome since they were significantly higher in non-survivors (median 2,410 ng/ml) than in survivors (median 1,552 ng/ml p < 0.01) (Table 3) and displayed a direct correlation with clinical severity scores (APACHE II: r = 0.3858, p < 0.01; SOFA: r = 0.4759, p < 0.001). Furthermore, during the resolution phase, osteopontin levels significantly decreased (median 438 ng/mL) compared to the overt disease (p < 0.001), but were still threefold higher than in the controls (Fig. 1).
Serum osteopontin levels during resolution. Serum levels of osteopontin in patients with SIRS (triangles) or severe sepsis/septic shock (circles) evaluated in the acute and in the resolution phase. The gray box represents the median (horizontal dotted bar) and the 25th and 75th percentile of controls. *p < 0.05, Wilcoxon signed rank test
Serum cytokine profile
In the pathogenesis of SIRS and sepsis, a role has been suggested for both pro- and anti-inflammatory cytokines and for the balance between TH1 and TH2 responses. To draw a broader picture of the behavior of osteopontin within the global cytokine response, we evaluated the serum levels of IL6 and TNF-α (acute inflammation cytokines), IL2 and IFN-γ (TH1 cytokines), and IL4, IL5 and IL10 (TH2 cytokines) in patients and controls. Few patients displayed detectable levels of TNF-α, IFN-γ, IL2, IL4, and IL5 and no significant differences were found with controls (data not shown). By contrast, levels of IL6 (median 81 ng/L, p < 0.0001) and IL10 (median 20 ng/L, p < 0.0001) were higher in patients (Table 3), as already reported [19, 20]. These data also showed that IL6 but not IL10 levels were significantly higher in SS/SS than in SIRS (median 130 vs. 55 ng/L, p < 0.01), whereas levels of both cytokines were higher in non-survivors compared to survivors patients, although only osteopontin levels reached statistical significance (Table 3). Osteopontin levels displayed a significant direct correlation with IL6 (r = 0.3033, p < 0.05) (Fig. 2), but not with IL10 (data not shown).
Osteopontin and IL6 as markers of inflammation and sepsis
In view of the significant difference of osteopontin and IL6 levels in patients with SS/SS and those with SIRS, we used the receiver operator characteristics curve (ROC) to explore their ability to differentiate SS/SS and SIRS patients (Fig. 3) [18]. The AUC was 0.796 (95% CI 0.667–0.892, p = 0.0001) for osteopontin and 0.727 for IL6 (95% CI 0.591–0.837, p = 0.0009). For osteopontin, the optimal s value discriminating between SS/SS and SIRS (1,708 ng/mL) gave a sensitivity of 70% and specificity of 79% with a positive likelihood ratio of 3.40.
Receiver operating characteristic curves. Receiver operating characteristic curve evaluating the accuracy of osteopontin and interleukin 6 in differentiating patients with severe sepsis/septic shock and SIRS. The area under the curve was 0.796 (95% CI 0.667–0.892; p = 0.0001) for osteopontin and 0.727 (95% CI 0.591–0.837; p = 0.0009) for interleukin 6
Osteopontin induces IL6 secretion in resting and activated monocytes
The direct correlation between osteopontin and IL6 in the patients’ sera raises the possibility that their production might be related. Therefore, we investigated the dose- and time-dependent effect of rOPN on IL6 secretion by monocytes.
Firstly, we performed titration experiments by treating monocytes with 0.1, 0.5, and 1 μg/ml of rOPN, (i.e., a range comprising OPN median levels of controls and patients). After 6 h, IL6 was measured in the supernatants by ELISA and IL6 mRNA was measured in cell extracts by real-time PCR. Results showed that levels of both IL6 mRNA and secreted protein were increased by rOPN treatment in a dose dependent manner (Fig. 4a).
Osteopontin induces secretion of interleukin 6 by monocytes. a Interleukin 6 is induced by recombinant osteopontin (rOPN) in a dose dependent manner both at mRNA (left panel) and protein (right panel) level. b Time-course evaluating interleukin 6 secretion by monocytes treated with vehicle control (left panel) or with lipopolysaccharide (LPS) (right panel) (25 ng/mL) and cultured for 6, 24 and 48 h, in the presence and absence of 1 μg/mL recombinant osteopontin. The significance of differences was determined with the Wilcoxon signed rank test. *p < 0.05. c Interleukin 6 secretion in monocytes not treated (NT), or treated with recombinant osteopontin (1 μg/mL), recombinant osteopontin and osteopontin neutralizing antibody (10 μg/mL) or lipopolysaccharide (LPS) (0.2 ng/mL). *p < 0.01 compared to lipopolysaccharide or untreated cells (NT); §p < 0.01 compared to sample with neutralizing antibody (α OPN) using Kruskal–Wallis test followed by Dunn’s multiple-comparison test
Secondly, we performed time-course experiments comparing the rOPN effect on IL6 secretion, in the presence or absence of lipopolysaccharide, to stimulate monocyte activation (Fig. 4b). Results showed that treatment with lipopolysaccharide induced secretion of high levels of IL6 (in the μg/mL range), which were already detectable after 6 h and increased after 24 and 48 h; this secretion was significantly increased by treatment with rOPN only at the 48 h time point. In the absence of lipopolysaccharide, rOPN induced secretion of low levels of IL6 (in the ng/mL range), but this effect was already detectable after 6 h of culture. The rOPN effect was not ascribable to modulation of monocytes death in culture, since LDH release and trypan blue exclusion test detected similar levels of cell death in all conditions (data not shown).
Lastly, we assessed the specificity of the rOPN effect to rule out if it was ascribable to the contaminant endotoxin (<0.2 ng endotoxin/μg rOPN) present in rOPN. To address this issue, we evaluated IL6 secretion induced by rOPN, in the presence or absence of anti-OPN neutralizing antibody (Fig. 4c). Results showed that addition of the neutralizing antibody abrogated the osteopontin-induced secretion of IL6. Moreover, we evaluated the effect on IL6 secretion of the maximal contaminant dose of endotoxin in the rOPN preparation. Results showed that no IL6 secretion was induced by the low doses of lipopolysaccharide alone (Fig. 4c) showing that the effect of rOPN is specific and not ascribable to contaminant endotoxin.
Discussion
The main finding of this study is that serum osteopontin levels are high in SIRS and SS/SS and correlate with IL6 levels. It also suggests that high osteopontin levels could be used to discriminate between SIRS and SS/SS, and that osteopontin might be involved in the pathogenesis of systemic inflammation, possibly through its effect on macrophages and its ability to enhance their IL6 secretion.
Osteopontin is implicated in several physiological and pathological events, including cell-mediated immunity, inflammation, tumor progression, and cell survival [21–23]. Originally viewed as mainly involved in bone remodeling and tissue debridement, its critical involvement in both acute and chronic inflammation is now apparent [9–12, 14, 24–27].
We and others have reported increased osteopontin levels in chronic inflammatory diseases such as multiple sclerosis [11, 12], systemic lupus erythematosus [10, 28], mycobacterial infection [13, 25], and HBV-induced liver cirrhosis [27]. Fewer reports focus on acute inflammatory diseases. One has shown that osteopontin levels are increased in patients with acute liver dysfunction [14]. In all these inflammatory diseases, osteopontin levels seem to be a good marker of the host response, since they increase in function of severity.
In this study, we found that serum osteopontin levels were tenfold higher in patients with SIRS or SS/SS than in the controls. They were also higher in SS/SS than in SIRS, and decreased with the resolution of both the conditions. Evaluation of osteopontin levels may thus be useful in monitoring the status and progression of these forms of systemic inflammation. Two of our findings indicate that osteopontin levels could be used to discriminate between SIRS and sepsis. Firstly, most septic patients (17/27, 63%) displayed higher osteopontin levels than the 75th percentile limit displayed by patients with SIRS (1,704 ng/mL). Secondly, the diagnostic accuracy of osteopontin in discriminating SIRS from SS/SS, as evaluated from the ROC curve, was similar to that reported in a recent meta-analysis for procalcitonin [29] and IL6 [19], i.e., the main serum protein markers currently used to monitor systemic inflammation.
The role of procalcitonin in the immune response is still poorly understood [30]. Its serum levels have been shown to correlate with the infection severity in sepsis. Even so, it is increasingly evident that procalcitonin does not provide a definitive diagnosis of sepsis [19, 31, 32] and its ability to discriminate sepsis from SIRS has been disproved [29, 32–34].
IL6 is believed to play a key role in sepsis through its effect on inflammation and the acute phase response. It is the most commonly used cytokine marker in the clinical setting of SIRS/sepsis [35, 36] and several studies have shown that high levels correlate with infection in adult patients. However, it seems no better than procalcitonin in the diagnosis of sepsis because it displays lower sensitivity and specificity [19]. Osteopontin levels could thus supplement the information given by procalcitonin and IL6.
A different issue is the role played by osteopontin in the pathogenesis of systemic inflammation. The direct correlation between the serum osteopontin and IL6 levels in SIRS and SS/SS suggests that these cytokines may be functionally related. One possibility is that their secretion is coordinated by the responsiveness to the same stimuli, especially since the osteopontin and IL6 genes share responsiveness to the transcription factor NF-IL6 involved in the acute phase response and macrophage activation [37]. However, our in vitro experiments suggest that osteopontin may also directly promote IL6 secretion, since rOPN induced mRNA expression and stimulated IL6 secretion by monocytes. A functional interaction between osteopontin and monocyte/macrophages is intriguing since these cells are activated by both necrotic cells and microbial endotoxins, and are believed to play a pivotal role in SIRS/sepsis. It is also intriguing that rOPN enhanced IL6 secretion in both the presence and the absence of high doses of lipopolysaccharide added to the cultures to mimic severe bacterial infections. Since our rOPN preparations contained low doses of contaminant endotoxin, these results do not prove that osteopontin is per se capable to induce IL6 secretion in the absence of monocyte-activating agents, but suggest that it may support the systemic inflammatory response even in the presence of limited amounts of these agents. This could be particularly relevant for sepsis under effective antibiotic therapy and SIRS.
The prominence of the functional interaction between osteopontin and macrophages is highlighted by data on osteopontin-deficient mice showing that osteopontin attracts to the injury sites and supports their survival [5, 7, 38, 39]. For instance, these mice show a markedly reduced macrophage infiltration in ischemic kidneys and an enhanced rate of apoptosis during the injury phase of acute renal failure [39]. Moreover, they display increased susceptibility to mycobacterial infections in which macrophages play a key role [40].
Our study did not investigate the source of osteopontin in SIRS/sepsis, but many OPN-producing cells present in injured and inflamed tissues may be involved since OPN is constitutively expressed by bone cells and several epithelial tissues, and is expressed upon activation by endothelial cells, macrophages, smooth muscle cells, NK cells, and activated T cells [5, 23].
In conclusion, our data show that osteopontin is strongly up-regulated during SIRS and sepsis and correlates with IL6 levels. Furthermore, they show that osteopontin induces IL6 release and enhances lipopolysaccharide-induced IL6 release by monocytes in vitro. To ascertain whether osteopontin offers a clinically relevant advantage over the markers currently used for diagnosis and monitoring of SIRS/sepsis, further studies with a higher number of patients are needed.
References
Alberti C, Brun-Buisson C, Burchardi H, Martin C, Goodman S, Artigas A, Sicignano A, Palazzo M, Moreno R, Boulme R, Lepage E, Le GR (2002) Epidemiology of sepsis and infection in ICU patients from an international multicentre cohort study. Intensive Care Med 28:108–121
Leibovici L, Shraga I, Drucker M, Konigsberger H, Samra Z, Pitlik SD (1998) The benefit of appropriate empirical antibiotic treatment in patients with bloodstream infection. J Intern Med 244:379–386
Cohen J, Carlet J (1996) INTERSEPT: an international, multicenter, placebo-controlled trial of monoclonal antibody to human tumor necrosis factor-alpha in patients with sepsis. International Sepsis Trial Study Group. Crit Care Med 24:1431–1440
Fisher CJ Jr, Dhainaut JF, Opal SM, Pribble JP, Balk RA, Slotman GJ, Iberti TJ, Rackow EC, Shapiro MJ, Greenman RL et al (1994) Recombinant human interleukin 1 receptor antagonist in the treatment of patients with sepsis syndrome. Results from a randomized, double-blind, placebo-controlled trial. Phase III rhIL-1ra Sepsis Syndrome Study Group. JAMA 271:1836–1843
Ashkar S, Weber GF, Panoutsakopoulou V, Sanchirico ME, Jansson M, Zawaideh S, Rittling SR, Denhardt DT, Glimcher MJ, Cantor H (2000) Eta-1 (osteopontin): an early component of type-1 (cell-mediated) immunity. Science 287:860–864
Gravallese EM (2003) Osteopontin: a bridge between bone and the immune system. J Clin Invest 112:147–149
Rollo EE, Laskin DL, Denhardt DT (1996) Osteopontin inhibits nitric oxide production and cytotoxicity by activated RAW264.7 macrophages. J Leukoc Biol 60:397–404
Takahashi F, Takahashi K, Shimizu K, Cui R, Tada N, Takahashi H, Soma S, Yoshioka M, Fukuchi Y (2004) Osteopontin is strongly expressed by alveolar macrophages in the lungs of acute respiratory distress syndrome. Lung 182:173–185
Mishima R, Takeshima F, Sawai T, Ohba K, Ohnita K, Isomoto H, Omagari K, Mizuta Y, Ozono Y, Kohno S (2007) High plasma osteopontin levels in patients with inflammatory bowel disease. J Clin Gastroenterol 41:167–172
Wong CK, Lit LC, Tam LS, Li EK, Lam CW (2005) Elevation of plasma osteopontin concentration is correlated with disease activity in patients with systemic lupus erythematosus. Rheumatology (Oxford) 44:602–606
Chiocchetti A, Comi C, Indelicato M, Castelli L, Mesturini R, Bensi T, Mazzarino MC, Giordano M, D’Alfonso S, Momigliano-Richiardi P, Liguori M, Zorzon M, Amoroso A, Trojano M, Monaco F, Leone M, Magnani C, Dianzani U (2005) Osteopontin gene haplotypes correlate with multiple sclerosis development and progression. J Neuroimmunol 163:172–178
Vogt MH, Lopatinskaya L, Smits M, Polman CH, Nagelkerken L (2003) Elevated osteopontin levels in active relapsing-remitting multiple sclerosis. Ann Neurol 53:819–822
Inomata S, Shijubo N, Kon S, Maeda M, Yamada G, Sato N, Abe S, Uede T (2005) Circulating interleukin 18 and osteopontin are useful to evaluate disease activity in patients with tuberculosis. Cytokine 30:203–211
Arai M, Yokosuka O, Kanda T, Fukai K, Imazeki F, Muramatsu M, Seki N, Miyazaki M, Ochiai T, Hirasawa H, Saisho H (2006) Serum osteopontin levels in patients with acute liver dysfunction. Scand J Gastroenterol 41:102–110
American College of Chest Physicians/Society of Critical Care Medicine Consensus Conference (1992) Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Crit Care Med 20:864–874
Knaus WA, Draper EA, Wagner DP, Zimmerman JE (1985) APACHE II: a severity of disease classification system. Crit Care Med 13:818–829
Vincent JL, Moreno R, Takala J, Willatts S, de MA, Bruining H, Reinhart CK, Suter PM, Thijs LG (1996) The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med 22:707–710
Metz CE, Herman BA, Shen JH (1998) Maximum likelihood estimation of receiver operating characteristic (ROC) curves from continuously-distributed data. Stat Med 17:1033–1053
Harbarth S, Holeckova K, Froidevaux C, Pittet D, Ricou B, Grau GE, Vadas L, Pugin J (2001) Diagnostic value of procalcitonin, interleukin 6, and interleukin 8 in critically ill patients admitted with suspected sepsis. Am J Respir Crit Care Med 164:396–402
Oberholzer A, Souza SM, Tschoeke SK, Oberholzer C, Abouhamze A, Pribble JP, Moldawer LL (2005) Plasma cytokine measurements augment prognostic scores as indicators of outcome in patients with severe sepsis. Shock 23:488–493
Jain S, Chakraborty G, Bulbule A, Kaur R, Kundu GC (2007) Osteopontin: an emerging therapeutic target for anticancer therapy. Expert Opin Ther Targets 11:81–90
Jansson M, Panoutsakopoulou V, Baker J, Klein L, Cantor H (2002) Cutting edge: attenuated experimental autoimmune encephalomyelitis in eta-1/osteopontin-deficient mice. J Immunol 168:2096–2099
O’Regan AW, Nau GJ, Chupp GL, Berman JS (2000) Osteopontin (Eta-1) in cell-mediated immunity: teaching an old dog new tricks. Immunol Today 21:475–478
Comabella M, Pericot I, Goertsches R, Nos C, Castillo M, Blas NJ, Rio J, Montalban X (2005) Plasma osteopontin levels in multiple sclerosis. J Neuroimmunol 158:231–239
Nau GJ, Chupp GL, Emile JF, Jouanguy E, Berman JS, Casanova JL, Young RA (2000) Osteopontin expression correlates with clinical outcome in patients with mycobacterial infection. Am J Pathol 157:37–42
Yamaguchi H, Igarashi M, Hirata A, Tsuchiya H, Sugiyama K, Morita Y, Jimbu Y, Ohnuma H, Daimon M, Tominaga M, Kato T (2004) Progression of diabetic nephropathy enhances the plasma osteopontin level in type 2 diabetic patients. Endocr J 51:499–504
Zhao L, Li T, Wang Y, Pan Y, Ning H, Hui X, Xie H, Wang J, Han Y, Liu Z, Fan D (2008) Elevated plasma osteopontin level is predictive of cirrhosis in patients with hepatitis B infection. Int J Clin Pract 62(7):1056–1062
D’Alfonso S, Barizzone N, Giordano M, Chiocchetti A, Magnani C, Castelli L, Indelicato M, Giacopelli F, Marchini M, Scorza R, Danieli MG, Cappelli M, Migliaresi S, Bigliardo B, Sabbadini MG, Baldissera E, Galeazzi M, Sebastiani GD, Minisola G, Ravazzolo R, Dianzani U, Momigliano-Richiardi P (2005) Two single-nucleotide polymorphisms in the 5′ and 3′ ends of the osteopontin gene contribute to susceptibility to systemic lupus erythematosus. Arthritis Rheum 52:539–547
Tang BM, Eslick GD, Craig JC, McLean AS (2007) Accuracy of procalcitonin for sepsis diagnosis in critically ill patients: systematic review and meta-analysis. Lancet Infect Dis 7:210–217
Meisner M (2002) Pathobiochemistry and clinical use of procalcitonin. Clin Chim Acta 323:17–29
Giamarellos-Bourboulis EJ, Mega A, Grecka P, Scarpa N, Koratzanis G, Thomopoulos G, Giamarellou H (2002) Procalcitonin: a marker to clearly differentiate systemic inflammatory response syndrome and sepsis in the critically ill patient? Intensive Care Med 28:1351–1356
Ruokonen E, Ilkka L, Niskanen M, Takala J (2002) Procalcitonin and neopterin as indicators of infection in critically ill patients. Acta Anaesthesiol Scand 46:398–404
Tugrul S, Esen F, Celebi S, Ozcan PE, Akinci O, Cakar N, Telci L (2002) Reliability of procalcitonin as a severity marker in critically ill patients with inflammatory response. Anaesth Intensive Care 30:747–754
Wanner GA, Keel M, Steckholzer U, Beier W, Stocker R, Ertel W (2000) Relationship between procalcitonin plasma levels and severity of injury, sepsis, organ failure, and mortality in injured patients. Crit Care Med 28:950–957
Doellner H, Arntzen KJ, Haereid PE, Aag S, Austgulen R (1998) Interleukin 6 concentrations in neonates evaluated for sepsis. J Pediatr 132:295–299
Resch B, Gusenleitner W, Muller WD (2003) Procalcitonin and interleukin 6 in the diagnosis of early-onset sepsis of the neonate. Acta Paediatr 92:243–245
Akira S, Isshiki H, Sugita T, Tanabe O, Kinoshita S, Nishio Y, Nakajima T, Hirano T, Kishimoto T (1990) A nuclear factor for IL6 expression (NF-IL6) is a member of a C/EBP family. EMBO J 9:1897–1906
O’Regan AW, Hayden JM, Body S, Liaw L, Mulligan N, Goetschkes M, Berman JS (2001) Abnormal pulmonary granuloma formation in osteopontin-deficient mice. Am J Respir Crit Care Med 164:2243–2247
Persy VP, Verhulst A, Ysebaert DK, De Greef KE, De Broe ME (2003) Reduced postischemic macrophage infiltration and interstitial fibrosis in osteopontin knockout mice. Kidney Int 63:543–553
Nau GJ, Liaw L, Chupp GL, Berman JS, Hogan BL, Young RA (1999) Attenuated host resistance against Mycobacterium bovis BCG infection in mice lacking osteopontin. Infect Immun 67:4223–4230
Acknowledgments
This work was partially supported by Telethon grant E1170 (Rome), AIRC (Milan), PRIN Project (MIUR, Rome), Compagnia di San Paolo (Turin), Regione Piemonte (Ricerca Sanitaria Finalizzata Project and Ricerca Sanitaria Applicata-CIPE Project), FISM 2005/R/10 (Genoa), Ricerca Corrente Ministeriale (Rome), Fondazione CARIPLO (Milan).
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is discussed in the editorial available at: doi:10.1007/s00134-008-1275-5.
Rights and permissions
About this article
Cite this article
Vaschetto, R., Nicola, S., Olivieri, C. et al. Serum levels of osteopontin are increased in SIRS and sepsis. Intensive Care Med 34, 2176–2184 (2008). https://doi.org/10.1007/s00134-008-1268-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-008-1268-4