Abstract
Objective
To determine the dose-response effects of noradrenaline on the systemic and renal circulations during septic shock.
Design and setting
Prospective controlled experiment in a university animal laboratory.
Subjects
Eight anaesthetized dogs.
Interventions
Transonic flow probes were surgically placed on the aorta via a left lateral thoracotomy and on the left renal artery. Blood pressure was measured from the femoral artery. Acute bacteraemia shock was induced by injecting Escherishia coli bacteria intravenously. Increasing doses of noradrenaline (0.1, 0.2, 0.3, 0.4, 0.5 µg kg−1 min−1) were infused intravenously for 30 min at 30-min intervals. The model was first validated in four dogs.
Measurements and results
Mean arterial pressure, central venous pressure, cardiac output, and renal blood flow were measured. Systemic vascular resistance was derived. Induction of bacteraemia decreased mean arterial pressure, central venous pressure and systemic vascular resistance. Cardiac output slightly increased. Noradrenaline produced linear dose-dependent increases in both mean arterial pressure and systemic vascular resistance. The response was attenuated during bacteraemia. Under non-bacteraemic conditions the maximum dose of noradrenaline reduced the renal blood flow from 12±1 to 10±1 ml kg−1 min−1. Bacteraemia further reduced renal blood flow to 7±1 ml kg−1 min−1, which was partly restored by the maximum dose of noradrenaline to 11±3 ml kg−1 min−1.
Conclusions
Noradrenaline can restore mean arterial pressure in bacteraemic shock and increases in mean arterial pressure are dose-dependent. The noradrenaline response is attenuated by bacteraemic shock. In bacteraemic shock noradrenaline also improves renal perfusion, as perfusion pressure increases. However, renal blood flow is not fully restored, suggesting that an element of impairment of renal blood flow exists due to the bacteraemia or noradrenaline.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Distributive shock is a common problem amongst intensive care patients and sepsis is one of the main causes. The associated hypotension, if sustained, causes under perfusion and ischaemia of vital organs, which leads to organ failure [1, 2, 3]. The renal circulation is at particular risk [4]. Treatment includes aggressive volume resuscitation and vasopressor support [1, 3]. Current opinion favours noradrenaline, particularly in severe cases [1, 3]. However, one of the main concerns with using noradrenaline is that in high doses it can impair perfusion of vital organs, such as the kidneys [2, 5].
In anaesthetized dogs Bellomo et al. showed that a single 0.3 µg kg−1 min−1 dose of noradrenaline improved renal perfusion in sepsis, whereas in non-septic conditions it impaired renal blood flow [6]. Similar findings have also been reported in septic sheep using 0.4 µg kg−1 min−1 [7, 8]. Treggiari et al. [5] using two different doses of noradrenaline in septic pigs found that a blood pressure increase of 10 mmHg improved renal blood flow, whereas further increases had no further benefit. However, it is not clear whether there is a threshold at which noradrenaline is no longer of benefit. To address this issue we investigated the systemic and renal effects of increasing doses of noradrenaline in bacteraemic dogs.
Materials and methods
All experiments were performed under license from the Government of the Hong Kong SAR and endorsed by the Animal Experimentation Ethics Committee of the Chinese University of Hong Kong.
Anaesthesia and maintenance of homeostasis
Anaesthesia was maintained with inhaled halothane (0.5–1.5%) in oxygen, the dose adjusted to prevent spontaneous movement. The trachea was intubated and the lungs were mechanically ventilated. Intravenous access was secured in the forelimb and normal saline infused at 2 ml kg−1 h−1. The femoral artery and left internal jugular vein were cannulated and used to measure artery blood pressure and central venous pressure, respectively. Body temperature was maintained by covering the dog with an insulated blanket. (A more comprehensive account of the animal model methods is provided in the Electronic Supplementary Material).
Placement of flow probes
Via a left thoractomy a 16- or 20-mm A-series transit time flow probe (Transonic Systems, Ithaca, N.Y., USA) was placed around the ascending aorta [9]. The chest was closed and chest drain inserted. Via a left longitudinal flank incision a 4-mm R-probe (Transonic Systems) was placed on the renal artery.
Blood flow and pressure measurements
The flow probes were connected to a T106 flowmeter (Transonic Systems); central venous pressure and transduced arterial pressure wave were measured intermittently. Data were transferred to a laptop computer where it was displayed in real-time and stored at 10-s intervals using the data acquisition program WinDaq (DataQ Instruments, Ohio, USA).
Induction of bacteraemic shock
Bacteraemic shock was induced over 1–2 h by injecting intravenously a bolus of 2×109 cfu Escherichia coli bacteria (JM 109 strain).
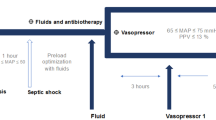
Circulatory management
The mean arterial pressure during the bacteraemic shock was maintained at around 60 mmHg and central venous pressure between 8 and 12 mmHg by infusing intravenously 100-ml aliquots of normal saline. Noradrenaline was delivered by syringe pump. Infusion rates of 0.1, 0.2, 0.3, 0.4 and 0.5 µg kg−1 min−1 were used.
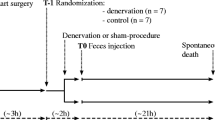
Part I: validity of the model
The reliability of the bacteraemic model was assessed in four dogs weighing 18–27 kg. The dog were prepared, and pre-bacteraemic haemodynamic data were recorded. Bacteraemic shock was then induced, and after 1 h a first set of baseline and noradrenaline response data recorded. Noradrenaline was infused for 5 min at 0.4 µg kg−1 min−1 and the peak effects recorded. Measurements were repeated at hourly intervals for the next 4 h. The dog was then killed.
Part II: noradrenaline dose response
In another eight dogs weighing 15–25 kg the haemodynamic response to increasing doses of noradrenaline was measured in both normal (non-bacteraemic) and bacteraemic conditions. The dog was prepared, and normal conditions were first tested. Pre-infusion values were measured. Noradrenaline was infused at 0.1 µg kg−1 min−1 for 30 min and then stopped for 30 min to allow the mean arterial pressure to return back to the baseline. The infusion rate was then increased and the protocol repeated until all five noradrenaline doses had been tested. Steady-state effects during the last 5 min of each infusion and recovery period were recorded. The dog was then made bacteraemic and the five doses of noradrenaline tested again. The experiment took 8–10 h to complete, and the dog was then killed.
Measured parameters
Mean arterial pressure, central venous pressure, cardiac output, heart rate and renal artery blood flow were recorded. Systemic vascular resistance was derived as: (mean arterial pressure−central venous pressure) ×80/cardiac output (dynes s−1 cm−5). The cardiac output and renal blood flow were indexed to the dog’s weight. The percentage of circulating blood flow perfusing both kidneys was estimated by dividing the cardiac output by 2 times the renal blood flow. The total fluid input and urine output during each phase of the study were recorded and divided by time to give an hourly rate.
Data analysis and statistics
Microsoft Excel was used for data analysis. Data were averaged over each 5 min collection period. The percentage changes from the baseline for each haemodynamic variable following induction of bacteraemia and each noradrenaline administration were calculated. Statistical analysis was performed using StatView for Windows (SAS Institute, Cary N.C., USA.). Student’s t test and analysis of variance for repeated measures (ANOVA-RM), with Bonferroni’s correction were used. Results were presented as mean ±standard deviation. Differences at the level of p<0.05 were considered statistically significant.
Results
Part I: validation of the model
The development of bacteraemic shock (n=4 dogs) resulted in a significant 27±4% decrease in mean arterial pressure (p=0.004, t test), which further decreased by 5±2% over the 4-h study period (Fig. 1; p=0.002, ANOVA-RM). The systemic vascular resistance decreased by 34±4% (p=0.009) and further decreased by 7±3% during the study (p=0.004). The central venous pressure decreased by 1.0±0.9 mmHg (p=0.04), but there was no further change during the study. The cardiac output index to weight increased by 7±2% (p=0.004) and further increased by 3±2% during the study (p<0.0001). The heart rate decreased by 17±2% (p=0.03), but there were no further changes during the study. The renal blood flow decreased by 35±6% (p=0.0006) and further decreased by 11±6% during the study (p<0.014). Noradrenaline increased the mean arterial pressure by 27±8% (p=0.004, t test), central venous pressure by 0.5±0.3 mmHg (p=0.04), cardiac index by 17±3% (p=0.004), and renal blood flow by 24±1% (p=0.0006) from the bacteraemic baseline (Fig. 1). These increases were consistent over the 4-h study period and returned to baseline once the noradrenaline was stopped (Fig. 1; p>0.05, ANOVA-RM).
Bar charts (mean ±standard deviation) demonstrating the reproducibility of baseline (black bars) and the noradrenaline response (grey bars) measurements from the bacteraemic model (n=4 dogs) recorded over a 4-h study period. Pre-bacteraemic data (white bars) also shown. ap<0.05 vs. pre-bacteraemic value; bp<0.05 vs. 1-h non-response value; cp<0.05 vs. 1-h value in series
Part II: noradrenaline dose response
Induction of bacteraemic shock (n=8 dogs) resulted in significant decreases in mean arterial pressure, systemic vascular resistance, renal blood flow and increase in heart rate (Table 1; p<0.0001, t test). Noradrenaline produced linear dose-dependent increases in mean arterial pressure under both normal and bacteraemic conditions (Fig. 2; p<0.0001, ANOVA-RM). When the noradrenaline was stopped, the mean arterial pressure returned to baseline, which remained constant throughout the experiment (Fig. 2). In addition to the decrease in mean arterial pressure following the induction of bacteraemic shock, there was also a significant reduction in the pressor response to noradrenaline (Fig. 2; p=0.0003). Similarly, linear dose-dependent increases were seen in systemic vascular resistance for both normal and bacteraemic conditions (Fig. 3; p<0.0001). There was also a reduction in the pressor response during bacteraemic conditions (p=0.003).
The effects (mean ±standard deviation) of noradrenaline dose on mean arterial pressure in anaesthetized dogs (n=8) during normal or pre-bacteraemic (upper plot) and bacteraemic (lower plot) conditions. Baseline line data after noradrenaline infusion discontinued (black bars) and the noradrenaline response (grey bars) shown. Reference (dotted lines) for normal response shown in lower plot. *p<0.05 vs. baseline
The central venous pressure was not significantly altered by the noradrenaline infusion in both normal and bacteraemic conditions (Fig. 3). In both normal and bacteraemic conditions cardiac index increased at the lower noradrenaline doses (Fig. 3; p=0.03), but this increase was not sustained at the higher doses, and there was no difference between the two groups (Fig. 3). Heart rate was increased by noradrenaline during bacteraemia (Fig. 3; p=0.05).
During normal conditions the renal blood flow decreased from 12±1 to 10±1 ml kg−1 min−1 at the highest noradrenaline infusion rates (p=0.002). During bacteraemic conditions the baseline renal blood flow was significantly decreased to 7±1 ml kg−1 min−1 (p<0.0001) and was partly restored to 11±3 ml kg−1 min−1 by the highest noradrenaline infusion rate (Fig. 4; p<0.0001). Similarly, during normal conditions the blood supply to the kidneys was 24±1%, and this percentage was reduced by noradrenaline to 21±2% (p<0.0001). Bacteraemic conditions reduced the baseline percentage blood flow to 15±2% (p<0.0001), and this percentage was partly restored by noradrenaline to 20±5% (Fig. 4; p<0.0001). There was a biphasic renal blood flow response to the noradrenaline infusion. During normal conditions the renal blood flow decreased as mean arterial pressure was increased. In contrast, during bacteraemic conditions the renal blood flow increased as mean arterial pressure was increased (data provided in Electronic Supplementary Material).
During the normal phase each dog received 225±21 ml h−1 or 10.8±1.1 ml kg−1 h−1 of intravenous fluid and their urine output was 64±9 ml h−1 or 3.1±0.3 ml kg−1 h−1. During the bacteraemic phase fluid intake increased to 321±19 ml h−1 or 15.5±1.2 ml kg−1 h−1 (p<0.01), and urine output decreased to18±3 ml/h or 0.8±0.1 ml kg−1 h−1 (p<0.01).
Discussion
Our main concern when using the bacteraemic dog model was whether the baseline circulatory status would remain constant. To answer this question we studied four bacteraemic dogs in which no major therapeutic interventions were made. We found that after the initial decreases in mean arterial pressure and renal blood flow following the induction of bacteraemic shock the dog’s circulation and noradrenaline response remained reasonably constant over a 4-h study period (Fig. 1). The pressor effect of noradrenaline was also very consistent (Fig. 1).
In our study noradrenaline produced linear dose-related increases in mean arterial pressure and systemic vascular resistance. However, this pressor response was attenuated during bacteraemia. This can be explained by a down-regulation of the vascular catecholamine receptor responsiveness, although the precise mechanism is unknown. However, the degree of down-regulation seems very variable and depends on the degree of septic shock. Thus regimens in sepsis for treating hypotension with noradrenaline should be based on blood pressure rather than dose.
Fluid administration is an important aspect of treating septic shock [1]. In the present study we gave repeated increments of intravenous saline to maintain the central venous pressure. Thus a normal volume status was maintained throughout the bacteraemic phase. Hypovolaemia was avoided, and cardiac output was keep constant (Table 1). However, one of the main criticisms of recent animal research to study vasopressors in septic shock has been that the circulatory condition did not mimic the clinical situation. In particular, septic shock patients tend to be fluid loaded and have hyperkinetic circulation which is associated with an increased cardiac output, which may be beneficial to organ perfusion. Further studies are needed.
Renal function was assessed by measuring renal blood flow. Some investigators have used more specific indicators of renal function such as urine output, renal oxygen consumption and glomerular filtration rate [10, 11, 12]. We measured the urine outputs for each phase of the experiment and during bacteraemia it decreased from 3 to less than 1 ml kg−1 h−1 despite adequate and increased volumes of intravenous fluids being given, indicating that significant renal shut down occurred during the bacteraemic phase. Under normal conditions the blood flow to the kidneys remained constant at 12 ml kg−1 min−1 (or 24%). Bacteraemia resulted in renal blood flow decreasing to 7 ml kg−1 min−1 (or 15%). Noradrenaline restored mean arterial pressure to 80 mmHg and renal blood flow back to 10 ml kg−1 min−1 (or 21%), but below the normal baseline (Fig. 4). Renal blood flow is autoregulated under normal circumstances, and increases in mean arterial pressure therefore tend to reduce renal blood flow. However, the autoregulatory threshold in mammals for renal perfusion is 80–180 mmHg [12]. When the blood pressure falls below this critical threshold, the kidneys stop autoregulating and blood flow becomes pressure dependent. Thus hypotension results in reduced kidney blood flow due to the low perfusion pressure. Treatment with noradrenaline benefits the perfusion of the kidneys by improving systemic blood pressure. However, our data suggest that there is still an element of renal vascular shut down within the kidneys. Whether higher doses of noradrenaline would have restored the renal perfusion to normal levels is unclear. Further studies are thus needed to investigate the effects of higher than 0.5 µg kg−1 min−1 doses of noradrenaline in bacteraemic shock.
References
Hollenberg SM, Ahrens TS, Annane D, Astiz ME, Chalfin DB, Dasta JF, Heard SO, Martin C, Napolitano LM, Susla GM, Totaro R, Vincent JL, Zanotti-Cavazzoni S (2004) Practice parameters for hemodynamic support of sepsis in adult patients: 2004 update. Crit Care Med 32:1928–1948
Guzman JA, Rosado AE, Kruse JA (2003) Vasopressin vs. norepinephrine in endotoxic shock: systemic, renal, and splanchnic hemodynamics and oxygen transport effects. J Appl Physiol 95:803–809
Kellum JA, Pinsky MR (2002) Use of vasopressor agents in critically ill patients. Curr Opin Crit Care 8:236–241
Richer M, Robert S, Lebel M (1996) Renal hemodynamics during norepinephrine and low-dose dopamine infusions in man. Crit Care Med 24:1150–1156
Treggiari MM, Romand JA, Burgener D, Suter PM, Aneman A (2002) Effects of increasing norepinephrine dosage on regional blood flow in a porcine model of endotoxin shock. Crit Care Med 30:1334–1339
Bellomo R, Kellum JA, Wisniewski SR, Pinsky MR (1999) Effects of norepinephrine on the renal vasculature in normal and endotoxemic dogs. Am J Respir Crit Care Med 4:1186–1192
Di Giantomasso D, May CN, Bellomo R (2002) Norepinephrine and vital organ blood flow. Intensive Care Med 28 1804–1809
Di Giantomasso D, May CN, Bellomo R (2003) Norepinephrine and Vital organ blood flow during experimental hyperdynamic sepsis. Intensive Care Med 29:1774–1781
Bednarik JA, May CN (1995) Evaluation of a transit-time system for the chronic measurement of blood flow in conscious sheep. J Appl Physiol 78:524–530
Schaer GL, Fink MP, Parrillo JE (1985) Norepinephrine alone versus norepinephrine plus low-dose dopamine: enhanced renal blood flow with combination pressor therapy. Crit Care Med 13:492–496
Hoogenberg K, Smit AJ, Girbes AR (1998) Effects of low-dose dopamine on renal and systemic hemodynamics during incremental norepinephrine infusion in healthy volunteers. Crit Care Med 26:260–265
Schetz M (2002) Vasopressors and the kidney. Blood Purif 20:243–251
Acknowledgements
We thank Mr. Anthony E. James, the Director of Laboratory Animals Services Centre of The Chinese University of Hong Kong, and his staff for their support and making this study possible. We also thank Mr. David Burrows and his staff at the Agriculture, Fisheries and Conservation Department of the Hong Kong Government for providing the animals used in this study.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article refers to the editorial available at http://dx.doi.org/10.1007/s00134-005-2740-z
Electronic Supplementary Material
Rights and permissions
About this article
Cite this article
Peng, ZY., Critchley, L.A.H. & Fok, B.S.P. The effects of increasing doses of noradrenaline on systemic and renal circulations in acute bacteraemic dogs. Intensive Care Med 31, 1558–1563 (2005). https://doi.org/10.1007/s00134-005-2741-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-005-2741-y