Abstract
Objective
To determine the incidence and risk factors for post-ICU mortality in patients with infection.
Design and setting
International observational cohort study including 28 ICUs in eight countries.
Patients
All 1,872 patients discharged alive from the ICU over a 1-year period were screened for infection at ICU admission and daily throughout the ICU stay. Outcomes at ICU and hospital discharge were recorded.
Measurements and results
Post-ICU death occurred in 195 (10.4%) patients and was associated in the multivariable analysis with age, chronic respiratory failure, immunosuppression, cirrhosis, Simplified Acute Physiology Score II on the first day with infection, and LOD score at ICU discharge. Post-ICU death was more common among medical patients and patients with hospital-acquired infection or microbiologically documented infection and was less common in patients with pneumonia.
Conclusions
Post-ICU death in patients with infection was within previously reported ranges in overall ICU populations. The main risk factors were patient and infection characteristics, severity at ICU admission, and persistent organ dysfunction at ICU discharge. Further interventions such as further ICU management, discharge to a step-down unit, or follow-up by intensivists on the ward should be evaluated in patients with a high risk of post-ICU mortality
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sepsis is a major challenge. Hospital mortality in patients with sepsis has ranged from 25% to 80% over the past few decades [1]. Although there is considerable heterogeneity in the epidemiology of sepsis [2], previous studies suggest that both the incidence of and mortality from sepsis may be diminishing [3]. However, severe sepsis remains a common reason for intensive care unit (ICU) admission with a high mortality rate and high management costs [4, 5]. Considerable effort has been expended to elucidate the pathophysiology of the systemic inflammation and multiorgan failure characteristic of severe sepsis [6]. Risk factors for death include severe physiological derangement, organ dysfunction, underlying illness, site of infection, and causative organism [2, 7]. Although massive resources have been invested in developing and evaluating potential treatments and strategies, there have been few successes [8, 9, 10] and many failures [11, 12].
After hospital discharge ICU patients have a fivefold higher risk of death than the general population [13]. Recent guidelines stress the importance of capturing long-term survival and quality-adjusted survival [14]. However, the hospital stay following discharge from the ICU also contributes to mortality, with wide variations across studies, from 6.1% to 27% [15, 16, 17]. Post-ICU in-hospital mortality (PIIHM) can be related to factors occurring before [18], during [17], or after [19, 20] the ICU stay. Goldfrad and Rowan [21] recently found that in-hospital mortality was higher among patients discharged from the ICU at night. Moreover, Daly et al. [22] suggested that keeping at-risk patients in the ICU for another 48 h might reduce PIIHM after ICU discharge by 39%. No studies specifically designed to investigate the characteristics of PIIHM in critically ill patients with infection have been published.
Infected patients are at higher risk of ICU mortality than ICU patients overall [4, 5]. Whether there is a similar difference regarding mortality on the ward after ICU discharge is unknown. We investigated risk factors for PIIMH in patients with infection from a large prospective cohort of unselected consecutive adults admitted to ICUs in Europe, Canada, and Israel between May 1997 and May 1998.
Patients and methods
Eligibility criteria
This prospective cohort study was conducted over a 1-year period in 28 ICUs in six European countries, Canada, and Israel (see Electronic Supplementary Material). Of these ICUs 25 (89%) were in teaching hospitals. The median number of beds was 632 per hospital (5th–95th percentiles, 450–1660) and 14 per ICU (6–28). There were 2 (7.1%) surgical units, 8 (28.6%) medical units, and 18 (64.3%) mixed units. Five units incompletely recorded hospital vital status and were excluded from the present analysis (one in Canada, two in Italy, one in Portugal, one in Spain). All 14,364 adults (age ≥18 years) consecutively admitted to the participating ICUs between 1 May 1997 and 30 April 1998 were entered into a database. Tables 1, 2, 3 report characteristics of the patients, ICU admissions, and infections; overall, there were 1,171 men (63%), median age was 60 years (range 43–71), and median Simplified Acute Physiology Score (SAPS) II on the first day of infection was 35 (range 26–44). Among these patients there were 2,984 with either clinically diagnosed or microbiologically documented infection. These were included in the study regardless of the severity of their infection [4] provided they had a ICU follow-up of 28 days or less after the onset of infection and were discharged alive from the ICU and followed until their discharge from the hospital. The final series for the present analysis thus included 1,872 patients. Among these, 195 (10.4%) died on the ward. To test the hypothesis that residual organ dysfunction at ICU discharge negatively influences hospital survival, organ dysfunctions were recorded daily in the ICU. If a patient was admitted more than once, only the data from the first admission were analyzed.
Data collection and definitions
In each participating ICU a single trained data collector recorded the data using standardized forms and dedicated database software derived from FoxPro (Microsoft Visual FoxPro 5.0, 1995). The data collector was a physician in 22 ICUs and a research nurse in 6 ICUs. For each patient the data collectors obtained and recorded data prospectively both by interviewing the physician in charge of the patient and by reviewing the medical charts. For all the study variables detailed definitions were provided in an operating manual.
The study variables are reported in Tables 1, 2, and 3. Comorbidities were recorded using the definitions included in the SAPS II [23] and the Acute Physiology and Chronic Health Evaluation II (APACHE II) [24]. Immunocompromised status included AIDS, cancer, bone marrow transplantation, and hematological malignancy. For computing SAPS II and LOD scores unavailable clinical and laboratory data were assigned zero values [23, 25]. Use at any time during the ICU stay of isotropic or vasopressor agents, ventilatory assistance, and renal replacement therapy were recorded.
Infection was defined as a suggestive clinical history, clinical symptoms, physical findings, and laboratory findings (a known or strongly suspected source of infection with positive cultures for a pathogen or gross pus in a closed space) that led to anti-infective treatment (excluding prophylaxis). Infections were categorized as clinically diagnosed or microbiologically documented and as community, hospital, or ICU acquired; they were also characterized according to the anatomical site or sites involved and to the causative micro-organism(s) [4]. Definitions of infection were those from the Centers for Disease Control [26].
Microbiologically documented infection was defined as infection confirmed by positive cultures of blood or samples from a site of suspected infection. Clinical infection was presence of gross pus or abscess formation (anatomical and/or by imagery and/or by histology) with negative microbiological studies. Community-acquired infection was defined as infection present at or within 48 h after hospital admission and hospital-acquired infection as infection developing 48 h or more after admission or in relation to a medical or surgical procedure. ICU-acquired infection was infection developing 48 h or more after ICU admission or related to a medical or surgical procedure performed during the ICU stay. When a patient experienced more than one episode of ICU-acquired infection, only the first episode was used in the analysis.
Follow-up and outcome variable of interest
Outcomes at hospital discharge were recorded. PIIHM was defined as mortality on the ward after ICU discharge. Median hospital length of stay calculated from ICU discharge to hospital discharge was 13 days [interquartile range 6–23, range 1–220]. Some patients remained in hospital for a long period or time (>3 months).
Quality of the data
Reliability checks, data audit, a hotline for queries and management of problems, and resolution of missing data and inconsistencies were performed as previously reported [4].
Statistical analysis
Categorical data are expressed as numbers and percentages and continuous data as medians and 25th–75th percentiles. Logistic regression was used to examine for independent predictors of PIIHM. First, univariate logistic regression was performed. Then variables for the multivariable logistic regression model were selected using bootstrapping, which involved analyzing a large number (500 independent replicates) of subsamples with replacement from the full sample followed by application of a stepwise logistic model to each sample with a backward-forward selection procedure at the 0.05 level. Covariates that were selected in more than 60% of the 500 samples were included in the final set of covariates and were fitted together [27]. We considered p values less than 0.05 statistically significant. The absence of a significant increase in the likelihood value upon omission of each of the remaining variables was checked. The results are expressed as the odds ratios with their 95% confidence intervals.
To determine homogeneous subgroups of PIIHM risk (i.e., low-risk <5% or high-risk >30%), we performed classification and regression tree (CART) analysis with variables identified as prognostic factors at the last step of the logistic regression analysis [28]. The first step consists in creating a model (building the tree) that includes all the variables (full model). In the second step the tree is pruned to a simpler tree that fits the information. The main advantage of CART is that no assumptions are made regarding the underlying distribution of values of the predictor variables. All statistical tests were two-tailed. CIs are presented with a 5% risk of type I error. Statistical analysis was performed using SAS 8.02 (SAS, Cary, N.C., USA) and S-plus 2000 (MathSoft, Seattle, Wash., USA) software packages for PCs.
Results
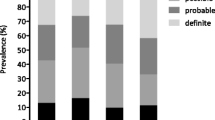
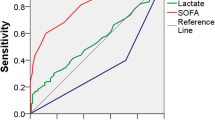
Figure 1 presents data on the cumulative incidence of death. Most deaths occurred during the first month after ICU discharge; some patients remained in hospital for a long period or time (>3 months). As shown in Tables 1, 2, and 3, several variables differed significantly between the patients who died after ICU discharge on the ward and those who were discharged alive from the hospital. Using bootstrap selection of these variables, we first introduced in the model those variables significantly associated with PIIHM in at least 60% of the selected samples. This identified ten variables independently associated with PIIHM by multivariable analysis (Table 4). Nine variables were associated with higher PIIHM: older age, immunocompromised status, cirrhosis, chronic respiratory failure, nonsurgical status, more severe disease (SAPS II) on the day of infection onset, more severe organ dysfunction (LOD score) on the day of ICU discharge, hospital-acquired infection, and microbiologically documented infection. The only protective variable was pulmonary infection compared to infection at other sites. Duration of mechanical ventilation, renal replacement therapy, and use of inotropic agents/vasopressors were not independently associated with PIIHM.
The final CART analysis (Fig. 2) used five of the ten predictors (LOD at ICU discharge, age, SAPS II at infection onset, origin of infection and immunosuppression). It successfully classified 91% of the patients. For each branch the mortality rate and the number of patients (in parentheses) are reported. The tree selected LOD at ICU discharge as the first variable, and the best split was a value of 4 which identified the patients with the highest PIIHM (threefold the overall value) as those who were also older than 50 years of age, had a SAPS II at onset of infection equal to or than 69 and a hospital-acquired infection. Hospital mortality of 56% was observed in the oldest and the most severely ill patients at onset of infection in ICU. The branch for LOD≤4 indicated the patients with the lowest PIIHM (tenfold less than overall) as those who either had an SAPS II at infection onset no greater than 27 or a SAPS II at infection onset greater than 27 but without immunodepression and with an age of 50 years or younger.
Discussion
This is the first international study focusing specifically on in-hospital death after ICU discharge of patients with infection. There are two major findings. First, PIIHM in patients treated for infection while in the ICU was within the ranges of PIIHM reported in overall ICU populations [15, 17, 29, 30, 31], but persistent organ dysfunction at ICU discharge was closely associated with PIIHM. Second, risk factors for PIIHM were similar to those reported previously for long-term mortality. The data from this study should help intensivists identify patients with infection who are at highest risk for PIIHM, and who consequently may be more likely to benefit from preventive strategies such as further ICU treatment, discharge to a step-down unit, or follow-up on the ward by the ICU team.
ICU mortality is higher in patients with infection than in other patients [4, 5, 32]. Our data suggest that this difference does not extend to the stay on the ward after ICU discharge. PIIHM was 10.4% in our study of patients with infection while in the ICU, which is within the PIIHM values in studies of overall ICU populations [15, 17, 29, 30, 31].
Mechanical ventilation, renal replacement therapy, and use of inotropic agents/vasopressors were not independently associated with PIIHM. Nevertheless, the LOD score at ICU discharge independently predicted PIIHM. A LOD score greater than 4, although implying a wide difference from a clinical point of view, discriminated between patients with and without PIIHM. However, the range of LOD scores at ICU discharge indicated that some patients were still critically ill and may have been discharged as an end-of-life decision [17, 33]. For instance, a switch to less aggressive treatment and ICU discharge may have been decided because acute organ dysfunctions had become chronic, indicating failure of ICU management or terminal disease [2]. In keeping with this possibility, PIIHM was higher in older patients and in those with severe comorbidities or with a poor chronic health status, as indicated by the McCabe scale. We have no evidence that any of the participating ICUs discharged patients prematurely to make room for other patients or discharged their patients from the ICU inappropriately, i.e., too early, at night, or on the weekend. However, the variable “discharged on the week-end” was not identified as a risk factor for PIIHM.
Risk factors for PIIHM in our study were similar to those previously reported to affect long-term mortality after ICU discharge, i.e., age, severe comorbidities (immunodepression, cirrhosis, and chronic respiratory failure), SAPS II on the day of infection, and LOD score on the day of ICU discharge. Previous research showed that severe underlying disease and preexisting organ dysfunction were associated with 28-day PIIHM in 1,052 patients meeting criteria for severe sepsis [34]. Similarly, Perl et al. [35] found that 6-month mortality was influenced by the severity of underlying illness and number of active comorbidities. In another study acute physiological derangement remained strongly associated with mortality up to 1 month after hospital discharge but was not predictive of 3-month mortality, in contrast to severe comorbidities [36]. Infection-related variables associated with PIIHM in our study, namely microbiological documentation and acquisition in the hospital, are related to disease severity and extent of organ dysfunction [4]. The absence of ICU-acquired infection among risk factors for PIIHM may be due to limited of statistical power or to death of a large majority of these patients in the ICU. Because the value of the sepsis classification has been challenged [4], we focused on infection itself. Our finding that older patients (surprisingly, starting at only 50 years of age) and those with comorbidities had higher PIIHM rates suggests that PIIHM may increase in the near future as ICUs increasingly provide care to the oldest and sickest members of the community [37].
None of the risk factors for PIIHM identified in this study are amenable to modification, with the possible exception of acute organ dysfunction severity at ICU discharge, for which further ICU management might improve the post-ICU outcome. Daly et al. [22] suggested that PIIHM in high-risk patients could be reduced by 39% by prolonging the ICU stay by 48 h. However, we do not know the proportion of patients who were discharged from the ICU as an end-of-life decision, i.e., who were expected to die on the ward. Without this information we cannot conclude from our data that further ICU management to improve organ dysfunction before ICU discharge would decrease PIIHM [17]. Thus our data are useful mainly for identifying patients at higher risk of death after ICU discharge.
A limitation of the study is the exclusion of patients who stayed in the ICU more than 28 days after onset of their infection. However, these patients had more severe disease at infection onset, suggesting that their longer ICU stay reflected a need for longer treatment to improve their organ dysfunctions. Their PIIHM rate was 15%, slightly higher than in the study patients, so that inclusion of these patients would probably have provided further support for the prognostic value of LOD at ICU discharge. The CART analysis has also some limitations. It requires the absence of correlation among independent variables and the multiplicative or additive role of the variables on the response variable. However, the variables selected by the CART analysis are these independently associated with PIIHM in multivariable logistic regression. Moreover, we did not use Bonferroni’s reduction for multiple testing.
In conclusion, our study provides useful data for identifying patients at high risk for PIIHM. These patients may be particularly likely to benefit from careful timing of ICU discharge, discharge to step-down units, follow-up by the ICU team on the ward, and efforts to improve communication with the team on the ward. Studies are needed to determine whether these strategies reduce PIIHM in patients with infection.
References
Friedman G, Silva E, Vincent JL (1998) Has the mortality of septic shock changed with time. Crit Care Med 26:2078–2086
Angus DC, Wax RS (2001) Epidemiology of sepsis: an update. Crit Care Med 29:S109–S116
Centers for Disease Control (1990) Increase in national hospital discharge survey rates for septicemia: United States, 1979–1987. MMWR Morb Mortal Wkly Rep 39:31–34
Alberti C, Brun-Buisson C, Burchardi H, Martin C, Goodman S, Artigas A, Sicignano A, Palazzo M, Moreno R, Boulme R, Lepage E, Le Gall R (2002) Epidemiology of sepsis and infection in ICU patients from an international multicentre cohort study. Intensive Care Med 28:108–121
Angus DC, Linde-Zwirble WT, Lidicker J, Clermont G, Carcillo J, Pinsky MR (2001) Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit Care Med 29:1303–1310
Calandra T (2001) Pathogenesis of septic shock: implications for prevention and treatment. J Chemother 13 [suppl 1]:173–180
Brun-Buisson C, Doyon F, Carlet J (1996) Bacteremia and severe sepsis in adults: a multicenter prospective survey in ICUs and wards of 24 hospitals. French Bacteremia-Sepsis Study Group. Am J Respir Crit Care Med 154:617–624
Bernard GR, Vincent JL, Laterre PF, LaRosa SP, Dhainaut JF, Lopez-Rodriguez A, Steingrub JS, Garber GE, Helterbrand JD Ely EW, Fisher CJ Jr (2001) Efficacy and safety of recombinant human activated protein C for severe sepsis. N Engl J Med 344:699–709
Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, Knoblich B, Peterson E, Tomlanovich M (2001) Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med 345:1368–1377
Annane D, Sebille V, Charpentier C, Bollaert PE, Francois B, Korach JM, Capellier G, Cohen Y, Azoulay E, Troche G, Chaumet-Riffaut P, Bellissant E (2002) Effect of treatment with low doses of hydrocortisone and fludrocortisone on mortality in patients with septic shock. JAMA 288:862–871
Zeni F, Freeman B, Natanson C (1997) Anti-inflammatory therapies to treat sepsis and septic shock: a reassessment. Crit Care Med 25:1095–1100
Abraham E (1999) Why immunomodulatory therapies have not worked in sepsis. Intensive Care Med 25:556–566
Keenan SP, Dodek P, Chan K, Hogg RS, Craib KJ, Anis AH, Spinelli JJ (2002) Intensive care unit admission has minimal impact on long-term mortality. Crit Care Med 30:501–507
Weinstein MC, Siegel JE, Gold MR, Kamlet MS, Russell LB (1996) Recommendations of the Panel on Cost-effectiveness in Health and Medicine. JAMA 276:1253–1258
Goldhill DR, Sumner A (1998) Outcome of intensive care patients in a group of British intensive care units. Crit Care Med 26:1337–1345
Rowan KM, Kerr JH, Major E, McPherson K, Short A, Vessey MP (1993) Intensive Care Society’s APACHE II study in Britain and Ireland. II. Outcome comparisons of intensive care units after adjustment for case mix by the American APACHE II method. BMJ 307:977–981
Azoulay E, Adrie C, de Lassence A, Pochard F, Moreau D, Thierry G, Cheval C, Moine P, Garrouste-Orgeas M, Alberti C, Cohen Y, Timsit J (2003) Determinants of post ICU mortality: a multicentre study. Crit Care Med 31:428–432
Bion J (1995) Rationing intensive care. BMJ 310:682–683
Ridley S, Purdie J (1992) Cause of death after critical illness. Anaesthesia 47:116–119
Wallis CB, Davies HT, Shearer AJ (1997) Why do patients die on general wards after discharge from intensive care units? Anaesthesia 52:9–14
Goldfrad C, Rowan K (2000) Consequences of discharges from intensive care at night. Lancet 355:1138–1142
Daly K, Beale R, Chang RW (2001) Reduction in mortality after inappropriate early discharge from intensive care unit: logistic regression triage model. BMJ 322:1274–1276
Le Gall JR, Lemeshow S, Saulnier F (1993) A new Simplified Acute Physiology Score (SAPS II) based on a European/North American multicenter study. JAMA 270:2957–2963
Knaus WA, Draper EA, Wagner DP, Zimmerman JE (1985) APACHE II: a severity of disease classification system. Crit Care Med 13:818–829
Le Gall JR, Klar J, Lemeshow S, Saulnier F, Alberti C, Artigas A, Teres D (1996) The Logistic Organ Dysfunction system. A new way to assess organ dysfunction in the intensive care unit. ICU Scoring Group. JAMA 276:802–810
Garner JS, Jarvis WR, Emori TG, Horan TC, Hughes JM (1988) CDC definitions for nosocomial infections, 1988. Am J Infect Control 16:128–140
Sauerbrei W, Schumacher M (1992) A bootstrap resampling procedure for model building: application to the Cox regression model. Stat Med 11:2093–2109
Marshall RJ (2001) The use of classification and regression trees in clinical epidemiology. J Clin Epidemiol 54:603–609
Rowan KM, Kerr JH, Major E, McPherson K, Short A, Vessey MP (1993) Intensive Care Society’s APACHE II study in Britain and Ireland. I. Variations in case mix of adult admissions to general intensive care units and impact on outcome. BMJ 307:972–977
Latour J, Lopez-Camps V, Rodriguez-Serra M, Giner JS, Nolasco A, Alvarez-Dardet C (1990) Predictors of death following ICU discharge. Intensive Care Med 16:125–127
Munn J, Willatts SM, Tooley MA (1995) Health and activity after intensive care. Anaesthesia 50:1017–1021
Vincent JL, Moreno R, Takala J, Willatts S, De Mendonca A, Bruining H, Reinhart CK, Suter PM, Thijs LG (1996) The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med 22:707–710
Fried TR, Bradley EH, Towle VR, Allore H (2002) Understanding the treatment preferences of seriously ill patients. N Engl J Med 346:1061–1066
Brun-Buisson C, Doyon F, Carlet J, Dellamonica P, Gouin F, Lepoutre A, Mercier JC, Offenstadt G, Regnier B (1995) Incidence, risk factors, and outcome of severe sepsis and septic shock in adults. A multicenter prospective study in intensive care units. French ICU Group for Severe Sepsis. JAMA 274:968–974
Perl TM, Dvorak L, Hwang T, Wenzel RP (1995) Long-term survival and function after suspected gram-negative sepsis. JAMA 274:338–345
Sasse KC, Nauenberg E, Long A, Anton B, Tucker HJ, Hu TW (1995) Long-term survival after intensive care unit admission with sepsis. Crit Care Med 23:1040–1047
Dodek P, Herrick R, Phang PT (2000) Initial management of trauma by a trauma team: effect on timeliness of care in a teaching hospital. Am J Med Qual 15:3–8
Acknowledgements
The authors are indebted to A. Wolfe MD for her assistance in rewriting the manuscript.
Author information
Authors and Affiliations
Consortia
Additional information
Supported by an educational grant from Roche.
An erratum to this article is available at http://dx.doi.org/10.1007/s00134-004-2532-x.
Electronic Supplementary Material
Rights and permissions
About this article
Cite this article
Azoulay, É., Alberti, C., Legendre, I. et al. Post-ICU mortality in critically ill infected patients: an international study. Intensive Care Med 31, 56–63 (2005). https://doi.org/10.1007/s00134-004-2484-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-004-2484-1