Abstract
Background
The purpose of this study was to determine the incidence of candiduria in critically ill patients admitted to intensive care medical units (ICUs), to identify risk factors for candiduria and to assess the frequency distribution of different Candida spp.
Subjects and methods
This was a prospective cohort observational and multicenter study. A total of 1,765 patients older than 18 years of age who were admitted for at least 7 days to 73 medical-surgical ICUs of 70 Spanish hospitals were included in the study. Urine cultures were performed once a week.
Results
In 389 patients (22%), Candida spp. in one or more urine samples were isolated. In the multivariate analysis, independent risk factors for candiduria included: age >65 years, female sex, length of hospital stay before ICU admission, diabetes mellitus, total parenteral nutrition, mechanical ventilation and previous use of antimicrobials. Candida albicans was recovered in 266 cases (68.4%), followed by C. glabrata (32 cases, 8.2%) and C. tropicalis (14 cases, 36%). Previous use of antifungal agents was the only risk factor for the selection of Candida non-albicans candiduria (OR 2.64, 95% CI 1.35–5.14, P =0.004). In-hospital mortality was 48.8% in patients with candiduria compared to 36.6% in those without candiduria ( P <0.001). Significant differences were also found for ICU mortality (38.% vs. 28.1%, P <0.001).
Conclusions
Twenty-two percent of critically ill patients admitted for more than 7 days in the ICU developed candiduria. C. albicans was the most frequent causative pathogen. Previous use of antifungals was the only risk factor for the selection of Candida non-albicans.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Detection of Candida spp. in urine samples from the healthy population is uncommon. However, candiduria is increasingly being an important problem in patients admitted to hospitals and long-stay institutions, particularly in subjects with altered immunological mechanisms, such as diabetes mellitus or neoplasms, carriers of permanent urinary catheters and those periodically receiving broad-spectrum antibiotics or steroids [1, 2, 3, 4, 5].
In patients admitted to intensive care units (ICUs), the presence of candiduria has increased in recent years, especially among patients requiring prolonged urinary catheterization or receiving broad-spectrum antibiotics. At the present time, between 10 and 15% of urinary tract infections in ICU patients are caused by Candida spp. [6, 7, 8]. In these patients, concurrent factors that contribute to the selection of these pathogens, including disorders prior to ICU admission (underlying illness), impaired natural defense barriers, multiple manipulations by health care personnel and altered bacterial flora as a result of the use of antibiotics for long periods of time, are usually present. In recent years, detection of different Candida spp. has become a standard in daily practice of clinical microbiology laboratories, which in turn has allowed progressively increasing detection of species of Candida non-albicans. Some of these non-albicans strains are resistant to azoles compounds, the class of drugs of first choice for the treatment of this infection [9].
The purpose of this study was to determine the incidence of candiduria in critically ill patients admitted to ICUs for more than 7 days, to identify risk factors for candiduria and to assess the frequency distribution of different Candida spp. as well as factors influencing the selection of a particular species.
Subjects and methods
Study population
A total of 1,765 patients older than 18 years of age who were admitted for at least 7 days to 73 medical-surgical Intensive Care Units (ICUs) of 70 Spanish hospitals between May 1998 to January 1999 were included in the study.
Design
This was a prospective, cohort, observational and multicenter study. In all patients, urine cultures were performed once a week. In order to assess the spread of Candida spp. to other mucosa, samples from tracheal aspirates, pharyngeal exudates and gastric aspirates were obtained. The initial urine sample was obtained 8 days after admission to the ICU, and once a week thereafter. Other samples from the peripheral blood, intravascular lines, feces, wound exudates, surgical drains or other infectious foci were obtained at the discretion of the attending physician.
Samples were processed by the different reference clinical microbiology laboratories of the participating hospitals according to standard procedures including Sabouraud agar culture and BACTEC method (Becton Dickinson Diagnostic Instrument Systems, Paramus, N.J.) for the isolation of species. The A20C system (Byomerieux, Lyon, France) was used for species identification.
For each patient, the following data were recorded: demographic features, underlying disease, concomitant infections, previous treatment with antibiotics, antifungals or immunosuppressive agents and presence and duration of risk factors (urinary bladder catheter, intravascular catheters and mechanical ventilation). Patients were followed until discharge from the ICU or death during ICU stay for the detection of candiduria, or otherwise until discharge from the hospital for assessment of the in-hospital mortality rate. According to diagnoses at the time of ICU admission, patients were classified: medical, surgical, trauma, ischemic heart disease, burns, organ transplantation and hematological. The severity of illness on ICU admission was calculated by the APACHE II score system [10]. Surgery prior to ICU admission was divided into urgent or elective. Only insulin-treated patients were considered as having diabetes mellitus (insulin-dependent diabetes mellitus, IDDM). Chronic bronchitis was defined as the presence of a productive cough or expectoration for more than 90 days a year (although on separate days) and for more than 2 consecutive years provided that a specific disorder responsible for these symptoms was not present. In patients with signs of portal hypertension, such as esophageal varices or ascites, chronic liver disease was confirmed by liver biopsy. Histological evidence was required for the diagnosis of solid tumor and a definitive diagnosis for the diagnosis of hematological malignancy. Human immunodeficiency virus (HIV) infection was defined in HIV-positive carriers and immunosuppression as an altered immune status according to the Centers for Disease Control (CDC) revised classification [11], or in case of a previous diagnosis (congenital or acquired). Neutropenia was defined as total leukocyte count ≤500/mm3. Renal failure was considered in patients requiring hemodialysis or peritoneal dialysis at the time of admission to the hospital. Severe heart failure was defined as grades III and IV of the NYHA classification [12]. Transplant recipients were those patients with solid organ or bone marrow transplantation. Use of steroids was considered in patients treated with a daily dose equivalent to 20 mg prednisone at least for 2 weeks, or 30 mg at least for 1 week before isolation of Candida in urine cultures. Chemotherapy was defined as use of cytotoxic agents for the treatment of a neoplasm or an autoimmune disease within 30 days prior to ICU admission. Alcohol abuse was defined as daily consumption of more than 80 g ethanol. Selective decontamination of the gastrointestinal tract was considered in patients receiving non-absorbable antimicrobials effective against potentially pathogenic microorganisms or fungi by the oropharyngeal or gastric (or both) routes.
Definitions
Candiduria was defined as the presence of >104 colony-forming units (cfu) of Candida spp. in urine, candidemia as recovery of Candida spp. from blood samples (in one or more culture bottles) and invasive candidiasis as growth of Candida spp. in normally sterile cavities or tissues (>105 cfu per gram of tissue). A definitive diagnosis of invasive candidiasis was established by positive culture of tissue specimens, endophthalmitis, peritoneal fluid culture and obstruction of the urinary tract by fungal balls.
Statistical analysis
Qualitative variables are expressed as the percentage of distribution of each category and quantitative variables as the mean and standard deviation (SD) in normally distributed variables, or median and range when distribution departed from normality. The chi-square (χ2) test and the Student's t test or the Mann-Whitney U test were used for the comparison of categorical and normally distributed and non-normally distributed variables, respectively. The bivariate analyses included the comparison of patients with candiduria versus patients without candiduria, patients with candiduria and systemic candidiasis or candidemia versus patients with candiduria only and patients with C. albicans versus patients with Candida non-albicans candiduria. Significant variables in the bivariate analysis were included in three logistic regression models with a forward stepwise selection procedure, in which isolation candiduria, candiduria with systemic candidiasis or candidemia and Candida non-albicans candiduria were the independent variables, respectively. Results are expressed as odds ratio (OR) and 95% confidence interval (CI). Statistical significance was set at P <0.05.
Results
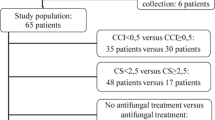
Candida spp. were isolated in at least one urine sample in 389 out of 1,765 patients during their stay in the ICU, with an incidence rate of candiduria of 22 per 100 patients who stay in the ICU for more than 7 days (range among the different participating ICUs 0–80%). In 1,730 cases (98%), patients had a urinary catheter inserted, with a total of 40,273 days of having a urinary catheter in place. The incidence density of candiduria in patients with urinary catheter was 9.5 episodes per 1,000 days of urinary catheter. In 204 cases (11.6%), Candida spp. were isolated in the first urinary sample obtained. In the population at risk, there was a progressive increase in the isolation of Candida spp. in urine cultures according to the duration of ICU stay (the more prolonged the stay, the greater the frequency of positive urine cultures for Candida spp.) (Table 1).
Patients with candiduria had a mean (SD) age of 61.20 (15.70) years. Fifty-one percent of patients were males. The mean APACHE II score at the time of ICU admission was 19.45 (7.17). The mean length of hospital and ICU stays since the identification of candiduria was 23.37 (18.86) and 16.26 (13.77) days, respectively. The duration of having a urinary catheter prior to diagnosis of candiduria was 16.35 (14.04) days. Underlying diseases were classified as medical in 55% of the patients, surgical in 38.6% and trauma in 14.6%.
Risk factors significantly associated with recovery of Candida spp. in urine included female sex, older age, particularly over 65 years, surgery as ICU diagnosis on admission, diabetes mellitus, use of total parenteral nutrition, central venous catheters, arterial lines, mechanical ventilation and previous use of antibiotic therapy (Table 2, Table 3). In the multivariate analysis, independent factors significantly associated with candiduria were age over 65 years (OR =1.47, 95% CI 1.15–1.86, P =0.001), female sex (OR =2.36, 95% CI 1.85–2.99, P =0.001), length of stay in hospital before ICU admission (OR =1.01, 95% CI 1.003–1.02, P =0.007), diabetes (OR =1.87, 95% CI 1.37–2.54, P =0.001), total parenteral nutrition (OR =1.82, 95% CI 1.43–2.32, P =0.001), mechanical ventilation (OR =2.74, 95% CI 1.50–5.00, P =0.001) and previous use of antibiotics (OR =2.48, 95% CI 1.28–6.01, P =0.04).
In 25 cases (5.9%), isolation of fungi in urine cultures was accompanied by isolation of bacteria, predominantly Enterococcus faecalis ( n =5), Pseudomonas aeruginosa ( n =5) and Escherichia coli ( n =3).
Candida albicans was isolated in 266 cases (68.4%), followed by C. glabrata in 32 (8.2%) and C. tropicalis in 14 (36%). In 55 cases (14%) species of Candida were not identified. Urinary tract infections caused by C. albicans predominated independently of the study week in which the first isolation was obtained. Different Candida species in the same urinary sample were isolated in only three cases. On the other hand, initial strains of C. albicans were replaced in subsequent weeks by C. tropicalis in six cases, C. glabrata in four, C. parapsilosis in two and C. krusei in one. In 10 of these 13 cases, previous treatment with antifungal agents was recorded.
In 105 (5.9%) out of 1,765 patients, an invasive infection caused by Candida spp. was diagnosed (candidemia, n =55; invasive candidiasis, n = 50). Candiduria was detected in 48 (45.7%) of all cases classified as infection, in 26 cases of candidemia and in 22 cases of invasive candidiasis. In 9 of the 26 cases of candidemia (34.6%), the episode was considered catheter-related. Differential characteristics of patients with candiduria with and without associated systemic candidiasis or candidemia are shown in Table 4. In the logistic regression analysis, independent factors significantly related to candiduria with systemic candidiasis or candidemia were as follows: urgent surgery (OR =2.5; 95% CI 1.128–4.085), extrarenal depuration procedures (OR =2.46; 95% CI 1.156–5.262, P =0.020) and total parenteral nutrition (OR =2.13; 95% CI 1.008–4.508, P = 0.048).
Candida non-albicans (excluding Candida spp.) was recovered in 76 (19.5%) cases in the group of patients with candiduria (63 on the initial specimen and 13 in subsequent samples). There were no differences between patients with candiduria due to C. albicans compared to patients with Candida non-albicans, except for previous treatment with antifungals ( P =0.003). In the logistic regression analysis, previous treatment with antifungal agents was the only independent risk factor significantly associated with Candida non-albicans candiduria.
Patients with candiduria compared to those without candiduria showed a significantly higher in-hospital mortality (48.8% vs. 36.6%, P <0.001) and ICU mortality (38.1 vs. 28.1%, P <0.001) rates. After adjusting for APACHE II at admission and underlying illnesses, candiduria remained as a risk factor for both ICU mortality (OR =1.48, 95% CI 1.16–1.90, P =0.002) and in-hospital mortality (OR =1.58, 95% CI 1.25–2.0, P <0.001).
Discussion
The present clinico-epidemiological study allowed us to establish that 22% of patients admitted to the ICU for a period longer than 7 days developed candiduria. In addition, risk factors for candiduria in this population were determined.
To our knowledge, there are no reference studies assessing the presence of candiduria in the subgroup of critically ill patients selected in our study. The National Nosocomial Infection Surveillance System (NNIS) identified Candida spp. as the major causative agent of urinary tract infection in patients admitted to medical and mixed (medical-surgical) ICUs [13, 14]. A surveillance study of nosocomial infection in ICU patients carried out in our country in 1994 [8] showed that Candida spp. was the second most frequent causative microorganism of urinary tract infection in patients with urinary catheters, ranging between 12–23% of the total causative pathogens of these infections. The rates of candiduria expressed as incidence density ranged from 0.7 to 1.6 episodes per 1,000 days of urinary catheter (data not shown). In another prevalence study, candiduria was diagnosed in 7% of the patients included [15]. Rates found in our study were 9.5 episodes per 1,000 days of urinary catheter, which are substantially higher than those previously reported due to, among other reasons, the highly selected population that was studied compared to surveillance studies; in these, all patients admitted to ICUs were included and patients with ICU length of stay <7 days predominanted. Therefore, probabilities of developing urinary infections caused by Candida spp. were very low.
One of the main limitations of our study was the lack of urinary control testing on ICU admission, so that the number of cases of candiduria already present compared to those acquired in the ICU is not known. On the other hand, there is a large variability in the rates of candiduria among the participating hospitals (between 0% and 80%), probably in relation to the characteristics of patients at each center. However, disparity in the rates of candiduria is counterbalanced by the high participation rate, and this allows to extrapolate the mean rate of candiduria obtained as a national reference rate for this type of population.
Prolonged use of urinary catheter is one of the risk factors related to candiduria reported in the literature [1, 2, 3, 4, 5, 16, 17, 18). All urinary catheters become colonized if left in place for prolonged periods; however, in our study, most patients included had a urinary catheter in place, so that the effect of this risk factor could not be evaluated. By contrast, in our study, like others [3, 4, 5], age older than 65 years, diabetes and female sex were identified as independent risk factors for candiduria. The effect of previous use of antibiotic therapy has been extensively documented in the literature [1, 2, 3, 4, 5, 14, 15, 16, 17, 18, 19]; moreover, it is the only factor to which interventions aimed at reducing this complication can be programmed. It is likely that antibiotics contribute to Candida spp. colonization by suppressing endogenous bacterial flora, primarily in the gut and lower genital tract, and then possibly in superficial areas adjunct to the uretral meatus [1]. Rational use of antibiotics and, particularly, early discontinuation of antimicrobials has been related to the decrease of non-bacterial emerging flora. Other risk factors identified in our study, such as mechanical ventilation or parenteral nutrition, are markers of the severity of illness in patients at risk, although they have no direct relationship in the selection or dissemination of fungi.
It should be noted that there was an important group of patients with candiduria in which Candida spp. was not identified. This finding may be explained in part by the opinion of some physicians who consider candiduria as a type of colonization without clinical implications, of benign nature, and infrequent as an origin of secondary candidemia [20, 21]. Other authors [7, 22], however, have recognized candiduria as a risk factor for invasive or disseminated candidiasis. For this reason, treatment with systemic antifungal agents, especially in high-risk patients, such as the majority of ICU patients, is highly recommended. In the present study, candiduria has been significantly associated with candidemia and/or invasive candidiasis, probably because our patients presented other concomitant risk factors for developing this infectious complication. Recently, risk factors for developing candidema in ICU patients have been prospectively identified [23] and included previous surgery, acute renal failure and use of parenteral nutrition. These factors were also frequently detected in our series.
Fisher et al. [24] have classified patients with candiduria in relation to the presence of predisposing factors for systemic candidiasis, making a differentiation between previously healthy and asymptomatic patients from those with risk factors for invasive candidiasis. In the present study, urgent surgery, extrarenal depuration procedures and total parenteral nutrition were identified as independent risk factors for candiduria in association with systemic candidiasis or candidemia. In this subgroup of patients, it is essential to perform further studies such as funduscopic examination as well as skin, vascular lines and blood cultures in order to establish an early diagnosis of this severe infectious complication. In the meantime, systemic antifungal agents should be administered in these patients with clinical signs of sepsis.
In our study, like others [4, 5, 9], C. albicans has been the predominant species in patients with candiduria, both in cases with an early diagnosis (within the 1st week) and in cases in which candiduria was detected in the subsequent weeks. Candida non-albicans was highly prevalent in the urine, probably in relation to the chemical composition of the urine and selectivity because of its pH for species of Candida non-albicans. In the present study, Candida non-albicans were isolated in more than 30% of cases, with C. glabrata as the most common. The increasing importance of these species, with a well-known resistance against commonly used antifungal agents (fluconazole), justifies typing of all Candida spp recovered in urine from ICU patients.
Previous treatment with antifungals was the only independent risk factor for isolation of Candida non-albicans; therefore, history of antifungal therapy should be adequately assessed to select the antifungal treatment of choice [7]. Nguyen et al. [25] in a study of candidemias have shown an important increase in Candida non-albicans in cases in which candidemia developed during antifungal therapy. C. parapsilosis and C. krusei were more frequent in patients previously given fluconazole, whereas C. glabrata was more common in patients previously given amphotericin B. In our study, the particular antifungal agent administered prior to isolation of Candida non-albicans was not recorded.
ICU patients with candiduria had a high mortality rate, which was greater than the mortality rate of ICU patients without this complication, probably in relation to greater severity of illness and complexity of these patients. However, the diagnosis of candiduria in a patient admitted to the ICU should be considered a marker of poor prognosis.
In summary, the present study has quantified and defined the profile of critically ill patients admitted to the ICU in which candiduria was developed. The only risk factor significantly associated with selection of the Candida non-albicans strain was the previous administration of antifungal agents.
References
Fisher JF, Chew WH, Shadomy S, Duma RJ, Mayhall CG, House WC (1982) Urinary tract infections due to Candida albicans. Rev Infect Dis 4:1107–1118
Stamm WE (1991) Catheter-associated urinary tract infections: epidemiology, pathogenesis, and prevention. Am J Med 91 [Suppl 3B]: 65–71
Gubbins PO, Piscitelli SC, Danziger LH (1993) Candidal urinay tract infections: a comprehensive review of their diagnosis and management. Pharmacotherapy 13:110–127
Storfer SP, Medoff G, Fraser VJ, Powderly WG, Dunagan WC (1994) Candiduria: retrospective review in hospitalized patients. Infect Dis Clin Pract 3:23–29
Kauffman CA, Vazquez JA, Sobel JD, Gallis HA, McKinsey DS, Karchmer AW, Sugar AM, Sharkey PK, Wise GJ, Mangi R, Mosher A, Lee JY, Dismukes WE (2000) Prospective multicenter surveillance study of funguria in hospitalized patients. The National Institute for Allergy and Infectious Diseases (NIAID) Mycoses Study Group. Clin Infect Dis 30:14–18.
Center for Infectious Diseases (2000) National Nosocomial Infections Surveillance (NNIS) System Report, data summary from January 1992-April 2000, issued June 2000. Am J Infect Control 28:429–448
Chabasse D (2001) Yeast count in urine. Review of literature and preliminary results of a multicenter prospective study carried out in 15 hospital centers. Ann Fr Anesth Reanim 20:400–406
Olaechea P, Alvarez Lerma F, de la Cal MA, Palomar M, Insausti J, y Grupo de Estudio de Vigilancia de Infección Nosocomial en UCI (2000) Evolución de la etiología de las infecciones urinarias relacionadas con sondaje uretral (abstract P131). Med Intensiva 24 [Suppl 1]:63
Harris AD, Castro J, Sheppard DC, Carmeli Y, Samore MH (1999) Risk factors for nosocomial candiduria due to Candida glabrata and Candida albicans. Clin Infect Dis 29:926–928
Knaus WA, Draper EA, Wagner DP, Zimmerman JE (1985) APACHE II: a severity of disease classification system. Crit Care Med 13:818–829
Center for Diseases Control (1992). 1993 revised classification system for HIV infection and expanded surveillance case definition for AIDS among adolescents and adult. MMWR 41 (RR-17):1–19
Goldman L, Hashimoto B, Cook EF, Loscalzo A (1981) Comparative reproducibility and validity of systems for assessing cardiovascular functional class: advantages of a new specific activity scale. Circulation 64:1227–1234
Richards MJ, Edwards JR, Culver DH, Gaynes RP, the National Nosocomial Infections Surveillance System (2000) Nosocomial infections in combined medical-surgical Intensive Care Units in the United States. Infect Control Hosp Epidemiol 21:510–515
Richards MJ, Edwards JR, Culver DH, Gaynes RP, and the National Nosocomial Infections Surveillance System (1999) Nosocomial infections in medical Intensive Care Units in the United States. Crit Care Med 27:887–892
Alvarez Lerma F, Cerda E, Jorda R, Palomar M, Bermejo B and ICU (EPIFUCI) Fungal Infection Study Group (2000) Fungal isolates in critically ill patients admitted to intensive care units (abstract 75). Intensive Care Med 26 [Suppl 3]: S235
Hamory BH, Wenzel RP (1978) Hospital-associated candiduria: predisposing factors and review of the literature. J Urol 2:444–448
Rivett AG, Perry JA, Cohen J (1986) Urinary candidiasis: a prospective study in hospital patients. Urol Res 14:183–186
Klimek JJ, Sayers R, Kelmas BW, Quintiliani R (1979) Statistical analysis of factors predisposing to candiduria. Conn Med 43:364–365
Golberg PK, Kozinn PJ, Wise GJ, Nouri N, Brooks RB (1979) Frequency and significance of candiduria. JAMA 241:582–584
Schönebeck J (1972) Asymtomatic candiduria. Scand J Urol Nephrol 6:136–146
Jacobs LG, Skidmore EA, Freeman K, Lipschultz D, Fox N (1996) Oral fluconazole compared with bladder irrigation with amphotericin B for treatment of fungal urinary tract infection in elderly patients. Clin Infect Dis 22:30–35
Nassoura Z, Ivatury RR, Simon RJ, Jabbour N, Stahl WM (1993) Candiduria as an early marker of disseminated infection in critically ill surgical patients: the role of fluconazole therapy. J Trauma 15:290–295
Blumberg HM, Jarvis WR, Soucie JM, Edwards JE, Patterson JE, Pfaller MA, Rangel-Frausto MS, Rinaldi MG, Saiman L, Wiblin RT, Wenzel RP (2001) Risk factors for candidal bloodstream infections in Surgical Intensive Care Unit patients: The NEMIS prospective multicenter study. The National Epidemiology of Mycosis Survey. Clin Infect Dis 33:177–186
Fisher JF, Newman CL. Sobel JD (1995) Yeast in the urine: solutions for a budding problem. Clin Infect Dis 20:183–189
Nguyen MH, Peacock JE Jr, Morris AJ, Tanner DC, Nguyen ML, Snydman DR, Wagener MM, Rinaldi MG, Yu VL (1996) The changing face of candidemia: emergence of non-Candida albicans species and antifungal resistance. Am J Med 100:617–623
Acknowledgements
We thank Marta Pulido, MD, for editing the manuscript and editorial assistance.
Author information
Authors and Affiliations
Corresponding author
Additional information
This study was carried out with the EPCAN Study Group: J. Nolla, F. Álvarez-Lerma, M Salvadó (Hospital del Mar, Barcelona); N. Carrasco, A. Bueno (Hospital de la Princesa, Madrid); F. Bobillo, P. Ucio (Hospital Clínico, Valladolid); M.A. León, M. Nolla, R.A. Díaz (Hospital General de Cataluña, Barcelona); J.R. Iruretagoyena, K. Esnaola, I. Andetxaga (Hospital de Cruces, Bilbao); A. Blanco, F. Taboada, R. Fernández (Hospital Nuestra Señora de Covadonga, Oviedo); M. Nieto, R. Diego, F. Ortuño (Hospital Clínico San Carlos, Madrid); P. Marcos, E. Mesalles (Hospital Germans Trias i Pujol, Badalona, Barcelona); A. Martínez, M. Fernández, F. Jaime (Hospital Virgen de la Arrixaca, Murcia); H. Sancho, N. Izquierdo (Hospital Reina Sofía, Córdoba); M. Ulibarrena, F. Labayen (Hospital Santiago Apóstol, Vitoria); F. Barcenilla, M.J. Gil, B. Balsera (Hospital Arnau de Villanova, Lleida); R. Jordá, M. Jurado, J. Pérez (Hospital Son Dureta, Palma de Mallorca); E. Zavala, A. Alcón, N. Fabregues (Hospital Clínic i Provincial, Barcelona); M.V. de la Torre, M.A. Estecha, A. Soler (Hospital Virgen de la Victoria, Málaga); M. Bodí, D. Castander (Hospital Joan XXIII, Tarragona); A. Mendía, J. Artaetxebarría, C. Reviejo (Hospital Nuestra Señora de Aránzazu, San Sebastián); M. Sánchez, A. Casamitjana, C. Pérez (Hospital Insular, Las Palmas de Gran Canaria); M.J. López, E. Robles (Hospital General de Segovia, Segovia); Y. Insausti, J.A. Tihistsa (Hospital de Navarra, Pamplona); C. García, J.M. Rubio (Hospital 12 de Octubre, Madrid); R. Oltra, O. Rodríguez (Hospital Clínico Universitario, Valencia); P. Olaechea, R. de Celís (Hospital de Galdakao, Bizkaia); J.M. Soto, J. Pomares (Hospital San Cecilio, Granada); J. Luna, G. Masdeu (Hospital Virgen de la Cinta, Tarragona); R. Sierra, A. Gordillo (Hospital Puerta del Mar, Cádiz); R. Rodríguez, J. Fajardo (Hospital Virgen de la Macarena, Sevilla); M.A. Herranz, J.I. Gómez (Hospital Río Hortega, Valladolid); R.M. García, M.J. Espina (Hospital de Cabueñes, Gijón); J. Garnacho, C. Ortiz (Hospital Virgen del Rocío, Sevilla); M. Palomar, J. Montero J (Hospital Vall d'Hebron, Barcelona); C. Cisneros, A. Sandiumenje (UCI de Traumatología, Hospital 12 de Octubre, Madrid); M. Sánchez, M. Álvarez (Hospital Príncipe de Asturias, Madrid); V. López, R. Julve (Hospital de Sagunto, Valencia); J. Solé, M. Valerón (Hospital Nuestra Señora del Pino, Las Palmas de Gran Canaria); M.A. Blasco, S. Borrás (Hospital Dr. Peset, Valencia); E. Maraví, J.M. Urtasun (Hospital Virgen del Camino, Pamplona); C. Sánchez-Díaz (Hospital San Pedro de Alcántara, Cáceres); L.M. Tamayo (Hospital Río Carrión, Palencia); J. Blanco (Complexo Hospitalario Xeral-Calde, Lugo); P. Galdós (Hospital General de Móstoles, Madrid); F. Barredo (Hospital de Torrecárdenas, Almería); A. Rodríguez (Hospital Santa María del Rosell, Cartagena); J. Castaño (Hospital Virgen de las Nieves, Granada); A. Bonet (Hospital Josep Trueta, Girona); M. Cerdá (Hospital de la Creu Roja, L'Hospitalet de Llobregat, Barcelona); A. Torres (UVIR, Hospital Clínic i Provincial, Barcelona); F. Pérez F (Fundación Jiménez Díaz, Madrid); J.M. Flores (UCI Traumatología, Hospital Virgen del Rocío, Sevilla); R. Diego (Hospital General Universitario, Valencia); C. Fernández (Complejo Hospitalario Insalud, León); A. Mas (Centre Hospitalari i Cardiologic, Manresa, Barcelona); F. Ruiz (Hospital Ciudad de Jaén, Jaén); C. León, (Hospital Nuestra Señora de Valme, Sevilla); M. Casanovas (Hospital de Igualada, Igualada, Barcelona); E.A. Sanz (Hospital Santa Ana, Motril, Granada); J.A. Artola (Hospital Naval de San Carlos, Cádiz); M.P. Luque (UCI de Traumatología, Hospital Clínico Univresitario, Zaragoza); C. Palazón (Hospital General Universitario, Murcia); C. Sotillo (Hospital Gregorio Marañón, Madrid); A. Bisbal (Policlínica Miramar, Palma de Mallorca); M.J. Huertos (Hospital de Puerto Real, Cádiz); F. Esteban (Hospital Sant Joan de Reus, Reus, Tarragona); P. Ugarte (Hospital Marqués de Valdecilla, Santander); R. Giral (Hospital General Yagüe, Burgos); V. González (Hospital Miguel Servet, Zaragoza); M.J. Serralta (Hospital San Juan, Alicante); A. Cercas (Hospital de Jerez, Cádiz); A. Nebra (Hospital Clínico Universitario, Zaragoza); C. Castillo (Hospital Txagorritxu, Vitoria-Gasteiz); A. Cercas (Hospital de Jerez, Cádiz); A. Nebra (Hospital Clínico Universitario, Zaragoza); C. Castillo (Hospital Txagorritxu, Vitoria), A. Tejada (UCI Traumatología, Hospital Miguel Servet, Zaragoza) and J.I. Gómez (REA, Hospital Río Ortega, Valladolid), Spain.
Rights and permissions
About this article
Cite this article
Álvarez-Lerma, F., Nolla-Salas, J., León, C. et al. Candiduria in critically ill patients admitted to intensive care medical units. Intensive Care Med 29, 1069–1076 (2003). https://doi.org/10.1007/s00134-003-1807-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-003-1807-y