Abstract
Objectives
Because respiratory muscle weakness appears to play an important role in weaning from mechanical ventilation, we developed an animal model of mechanical ventilation with appropriate controls in order to determine whether 24 h of mechanical ventilation already affected diaphragmatic function.
Design and interventions
Fifty-two male Wistar rats were randomized into three groups: a non-anesthetized control group (C, n=10), an anesthetized spontaneously breathing group (SB, n=9 out of 26), and an anesthetized and mechanically ventilated group (MV, n=12 out of 16).
Results
After 24 h, in vitro diaphragmatic force was decreased in SB group but even more so in MV group (i.e., 80 Hz: −15% in SB, P<0.005 vs C and −34% in MV group, P<0.005 vs C and SB). This was associated with a significant decrease in the diaphragm type I and type IIa dimensions in the SB group, which was more pronounced in the MV group. Interestingly, diaphragm IGF-I mRNA was decreased in the SB group (−14%, P<0.05 vs C), but more so in MV group (−29%, P<0.001 vs C and P<0.01 vs SB). Moreover, there was a significant correlation between diaphragm force and IGF-I mRNA (at 80 Hz r=0.51, P=0.0056).
Conclusions
We conclude that 24 h of mechanical ventilation in rats, independently of anesthesia, already significantly reduced diaphragm force, fiber dimensions, and its IGF-I mRNA levels.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Weaning from mechanical ventilation is a serious and frequent problem occurring in 20–50% of the patients under mechanical ventilation [1, 2, 3]. Evidence suggests that weaning problems are related to the respiratory muscle dysfunction induced by mechanical ventilation since weaning difficulties have been reported to be related to impaired inspiratory muscle force and endurance [4, 5, 6]. Mechanical ventilation represents a form of muscle disuse in which the diaphragm is made inactive and unloaded while phasically rhythmically shortened by passive lung inflation. This may induce muscular atrophy and result in alterations in contractile properties similar to the disuse atrophy seen in peripheral muscle during immobilization or unloading. On the other hand, mechanical ventilation may lead to biotrauma by inducing mechanical stress to the lungs, initiating thereby lung injury and inflammation (for a review see [7]).
At present, several studies have examined the effects of mechanical ventilation on muscle function in animals [8, 9, 10, 11, 12, 13, 14]. These data showed that diaphragm force was already decreased after 12 h of controlled mechanical ventilation and this worsened with prolongation of mechanical ventilation [12]. In addition, diaphragm fiber atrophy was already present such that the cross-sectional area of all the fibers was decreased [12]. Enhanced hybrid fiber co-expressing MHC-I+II at the expense of the MHC-I population was also described in the diaphragm after up to 4 days of controlled mechanical ventilation. Loss in diaphragm mass was reported after 48 h of controlled mechanical ventilation [9] while 3-day mechanical ventilation was associated with diaphragmatic myofibril damage in rabbits [13]. In addition, in vivo transdiaphragmatic pressure was reduced after 5 days of mechanical ventilation although nerve conduction and neuromuscular junction transmission were intact [11]. A longer duration of mechanical ventilation (11 days) also resulted in reduced endurance capacity [8]. All these studies clearly showed that mechanical ventilation exerted detrimental effects on diaphragm function.
In order to further examine to what extent short-term mechanical ventilation would lead to alterations in the diaphragm's intrinsic properties, the present study was designed to examine whether the local production of IGF-I would be impaired after mechanical ventilation. Local production of IGF-I has been shown to play an important role in muscle hypertrophy and atrophy [15, 16, 17, 18]. Knowing that IGF-I, by inhibiting the proteasome ubiquitin system, is an important anti-proteolytic agent [19], any decrease in its expression is expected to result in muscle atrophy. As Shanely et al. [14] recently demonstrated increased protein degradation along with elevated calpain and proteasome activity in the diaphragm of rats after 18 h of mechanical ventilation, we hypothesized that mechanical ventilation may induce these alterations by decreasing the IGF-I expression in the diaphragm. The latter may also be the early sign of muscle phenotype adaptation, as changes in local IGF-I have been shown to play a role in muscle fiber conversion [20].
Materials and method
Study design
The study was performed on 52 male Wistar rats (14 weeks old) randomly divided into three groups:
-
1.
A control group consisting of awake animals free of intervention (C, n=10).
-
2.
A group of anesthetized and spontaneously breathing rats in whom the same surgical procedures were performed as in animals under mechanical ventilation (SB, n=9 out of 26).
-
3.
A group of anesthetized rats under mechanical ventilation (MV, n=12 out of 16).
Randomization of the animals took into account the expected mortality such that, from a group of ten animals, two were assigned to the control group, five to the spontaneously breathing group and three to the mechanically ventilated group. The SB group was chosen as the appropriate control group for the MV group in order to separate the effects of surgical procedures, anesthesia, and associated effects from the effects due to mechanical ventilation. This SB group is not appropriate to examine the mechanisms by which anesthesia and/or surgical procedures affect diaphragm function. The study was approved by the Animal Experiments Committee of the Medical Faculty of the Katholieke Universiteit, Leuven.
Spontaneously breathing rats and rats under mechanical ventilation were initially anesthetized with sodium pentobarbital (60 mg/kg ip), and then tracheotomized while their body temperature was continuously maintained at 37 °C using a heating blanket. During the 24 h, continuous infusion of both anesthesia (sodium pentobarbital 2–3 mg/100 g/ml/h) and heparin (2.8 U/ml/h) was given via the right jugular vein and carotid, respectively, using osmotic pumps (Pilot A2, Fresenius, Schelle, Belgium). The flow of the heparin infusion was adapted in order to maintain the arterial blood pressure within the normal range. For the animals breathing spontaneously, the level of anesthesia was adapted to avoid hypo- or hyperventilation. Anesthesia depth was controlled throughout the experiment by evaluating foot reflex, corneal reflex, arterial blood pressure, and breathing pattern (for the SB group). Animals also received enteral nutrition including vitamins and minerals (Liquid diet 821338, SDS, Essex, UK) that was administered via a gastric tube (daily administration of 69 Kcal). SB and MV animals both breathed humidified air enriched with O2 and maintained at 37 °C. Mechanically ventilated animals were ventilated with a respiratory rate of 55–60 breath/min. During the 24 h of SB or MV, continuing care of the animals was performed including expressing the bladder, lubricating the eyes, rotating the animal, and passive movement of the limbs.
Upon completion of the 24 h of SB or MV, blood gases analysis of anesthetized animals was performed while control animals were anesthetized with sodium pentobarbital (60 mg/kg ip) and tracheotomized. Segments of the costal diaphragm were removed for measurement of in vitro contractile properties as previously described [21], and blood samples were taken for further analysis of electrolytes, creatinine, and total protein serum levels. Part of the remaining costal diaphragm was frozen in liquid nitrogen to examine mRNA levels of insulin-like growth factors I by RT-PCR while the other part was folded, cut transversely, and frozen in isopentane cooled with liquid nitrogen. In addition, the weights of scalenus medius and parasternal intercostals (respiratory muscles), and selected locomotor muscles (gastrocnemius plantaris, soleus, and extensor digitorum longus) were measured. Animals were killed by injecting a bolus of sodium pentobarbital into the heart.
Fiber type analysis
Serial sections of the costal diaphragm were cut at 10-µm thickness with a cryostat kept at −20 °C. Sections were stained for adenosine triphosphatase (ATPase) after acid preincubation at pH 4.5 and 4.3. Based on their histochemical reactions, fibers were identified as slow-twitch type I, fast-twitch type IIa or fast-twitch type IIx/b fibers. CSAs were determined from the number of pixels within the outlined borders using a Leitz Laborlux S. microscope (Wetzlar, Germany) at ×20 magnification, connected to a computerized image system (Quantimet 500, Leica, Cambridge, UK). Around 200 fibers were used to calculate CSA of all fiber types and proportion. To correct fiber cross-sectional areas for the muscle shortening occurring after excision, measured cross-sectional areas were divided by the ratio optimal length/excised length.
RNA extraction and RT-PCR
Total RNA was isolated using a modified guanidinium isothiocyanate-cesium chloride method [22]. Approximately 0.2 g of tissue was homogenized using an Ultra-Turrax homogenizer (Janke & Kunnel, Germany) in a solution containing 50% (w/v) guanidinium thiocyanate, 25 mM EDTA, 0.5% lauryl sarcosine, and 0.1 M 2-mercaptoethanol. The homogenate was layered on top of a solution containing 5.7 M cesium chloride, 25 mM sodium acetate (pH 5.0), and 10 mM EDTA. After ultracentrifugation at 20 °C in a SW41 rotor (Beckman, Germany) at 100,000 g for approximately 16 h the supernatant was removed, the RNA pellet was dissolved in water, the solution was adjusted to 0.3 M sodium acetate (pH 5.2), and the RNA was precipitated with 2.5 volumes of absolute ethanol. RNA was then rinsed in 70% ethanol, vacuum dried, and redissolved in water. Quality and quantity of the RNA preparations were determined by measurement of absorbance at 260 nm and 280 nm.
For the reverse transcriptase reaction, samples of 2 µg of total RNA from the diaphragm were subjected to oligo (dT)-primed first-strand cDNA synthesis in a volume of 20 μl (Gibco BRL thermoscript kit, Life Technologies, Merelbeke, Belgium). A 2-µl portion of the first-strand cDNA mixture was subjected to PCR (Perkin Elmer kit, Lennik, Belgium) under the conditions specified in Table 1. The number of PCR cycles was adjusted to avoid saturation of the amplification system. Amplification products were identified by their sizes. The amplification products were analyzed by electrophoresis on 6% (w/v) acrylamide gels. The amplified DNA fragments were stained with Vistra Green and the fluorescence levels of the bands were quantified by means of a PhosphorImager model 425 (Molecular Dynamics, Sunnyvale, Calif., USA). Band intensities of the amplified fragments were normalized to the corresponding L32 amplification signals. For each primer, PCR amplification was performed at least in duplicate.
Data analysis
Statistical analysis was performed using the SAS Statistical package (SAS Institute Cary, N.C., USA). Comparisons between the three groups were performed using a one-way analysis of variance. Differences between means were assessed using Gabriel post hoc test. Data are expressed as means and standard deviation (SD). Correlation was determined with Pearson's correlation coefficient.
Results
Mortality
In the MV group, 12 animals out of the 16 studied survived the 24 h while only nine out the 26 studied survived in the SB group. Thus, while mortality was 25% in the MV group, mortality was much higher in the SB group (65%). The reason why mortality was higher in the SB animals was related to the fact that in order to control the breathing pattern of these animals, the level of anesthesia infusion was adapted. However, because the safety dose of sodium pentobarbital is extremely narrow, the animals could be easily overdosed. There were, however, no significant differences in the amount of anesthesia infusion received by the SB animals and the MV rats (2–2.4 mg/100 g/ml/h).
Blood gases and arterial blood pressure
Blood gas analysis showed that PaO2 was in normal range for the anesthetized animals (SB: 123±33 mmHg and MV: 142±44 mmHg), as was PaCO2 (SB: 31±11 mmHg and MV: 33±15 mmHg) and pH (SB: 7.38±0.08 and MV: 7.45±0.14). Individual data showed that none of the animals was hypoxemic (PO2 range: 104–188 mmHg and 94–187 mmHg in the SB and MV group, respectively), hypercapnic (PCO2 range: 29–69 mmHg and 24–53 mmHg in the SB and MV group, respectively) or in acidosis (pH range: 7.25–7.45 and 7.28–7.56 in the SB and MV group, respectively). Arterial blood pressure averaged 129±22 mmHg and 104±30 mmHg in the SB and MV group, respectively.
Serum levels of electrolytes, creatinine, and total protein
There were no changes in serum levels of sodium, potassium, phosphate, and creatinine between the three groups (Table 2). Calcium plasma levels were significantly decreased in anesthetized animals compared to C but this decrease was similar in the SB and MV groups (−21%, P<0.001). Similarly, total protein content in plasma was decreased to the same extent in the SB and MV groups (−43 and −49%, respectively, P<0.001 vs C).
Body and muscle weight
Body weight was significantly different between the three groups such that the muscle mass was expressed as a percentage of body weight to allow for comparison (Table 3). When done in this way, then the mass of either the respiratory or the peripheral muscles was similar between the three groups. The reason why the starting body weight was different between the three groups was related to the fact that we did not make an attempt to match body weight between the groups, especially because the study was spread over time.
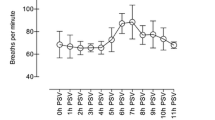
Diaphragm contractile properties
In vitro diaphragmatic twitch tension was significantly decreased in the MV group (−30%, P<0.05 vs C) as was tetanic tension (−33%, P<0.002 vs C) while twitch characteristics (time to peak tension and half-relaxation time) were not altered. Forces generated by the diaphragm during the force-frequency curve were significantly lower at 25 Hz and 50 Hz in SB (P<0.05 vs C), at all frequencies in MV rats compared to C (Fig. 1A) and at 80 Hz compared to SB (−34%, P<0.005). When force was expressed as a percentage of maximal tetanic tension, these effects persisted for both SB and MV except for twitch stimulation (Fig. 1B). Along the same lines, force generation during the low-frequency fatigue run was similarly lower in SB and MV diaphragms compared to C (Fig. 2A). However, when force was expressed as a percentage of initial values, force remained lower in MV diaphragms but only at the beginning of the run, while thereafter, a similar decline was present in all groups (Fig. 2B).
Force-frequency relationship expressed in A absolute values and B as a percentage of interposed 160 Hz stimulations in control (closed circles), spontaneous breathing (open squares), and mechanically ventilated rats (closed squares). Values are means and standard deviation. *P<0.05 MV vs C, #P<0.001 SB and MV vs C, **P<0.01 MV vs others, ##P<0.001 SB vs C
Fatigue curve expressed in A absolute values and B as a percentage of initial force. Same symbols as in Fig. 1. Values are means and standard deviation. *P<0.01 SB and MV vs C, #P<0.05 SB and MV vs C
Diaphragm fiber type analysis
Compared to C, a significant decrease in diaphragm type I and type IIa cross-sectional area was present in SB (−18 and −23%, respectively, P<0.05) and MV (−24 and −29%, respectively, P<0.05) (Fig. 3). In the latter group, also type IIx/b cross-sectional area was decreased by 25% but this decrease failed to reach statistical significance (Fig. 3). There were no significant differences in diaphragm fiber dimensions between the SB and MV group although the magnitude of the effects was more pronounced in the MV animals. Fiber distribution did not change whatever the condition.
Diaphragm IGF-I mRNA levels
Primers were designed to amplify a 151 bp fragment for IGF-I mRNA. Compared to C, IGF-I mRNA levels were significantly reduced in SB diaphragms (−14%, P<0.05 vs C) and more particularly in MV diaphragms (−29%, P<0.001 vs C) (Fig. 4). Interestingly, the downregulation of IGF-I in MV diaphragms was significantly more pronounced than that seen in SB rats (P<0.01) (Fig. 4). Moreover, there was a significant positive correlation between the diaphragm IGF-I mRNA expression and its force production (i.e., at 80 Hz r=0.51, P=0.0056) (Fig. 5).
Upper part. Representative gel of individual diaphragm from each group where insulin-like growth factor-I (IGF-I) and house-keeping gene (L32) mRNA levels were determined by RT-PCR. Lower part. Mean values and standard deviation of IGF-I amplified fragment normalized to the corresponding L32 amplification signals in controls (C, solid bar), anesthetized and spontaneously breathing rats (SB, open bar), and mechanically ventilated rats (MV, hatched bar). *P<0.05 and #P<0.001 vs C, **P<0.05 MV vs SB
Discussion
The present study showed that 24-h mechanical ventilation reduced diaphragmatic force and fiber dimensions. This was associated with the onset of an atrophy process as suggested by the decrease in IGF-I mRNA in this muscle that would probably lead to muscle wasting over time. We previously showed that a decrease in diaphragm IGF-I mRNA was associated with diaphragm atrophy induced by corticosteroid treatment [18]. Furthermore, a relationship between diaphragm force and IGF-I mRNA was also observed, suggesting a potential role for IGF-I in the alterations induced in the diaphragm by mechanical ventilation.
The data reported in the present study are unlikely to be related to effects other than mechanical ventilation itself. Indeed, since blood gases were maintained in the normal range, neither acidosis nor alkalosis were present in our model and may have contributed to the observed alterations. Along the same lines, electrolyte disturbances, that are known to affect muscle force production, did not occur in the present study. In particular, hypophosphatemia and hypokalemia were not present either in spontaneous breathing rats or in mechanically ventilated animals. Only plasma levels of calcium and total protein content were decreased in spontaneous breathing animals and in rats under mechanical ventilation. In fact, if the decreased calcium had affected the diaphragm force in the present study, the magnitude of this effect would have been very small. Indeed, in dogs, it has been shown that a 16% decrease in calcium serum levels induced by EGTA infusion was associated with a 4% decrease in the diaphragm force generated at 10 Hz and no changes at higher frequency [23]. Furthermore, because the decrease in calcium serum levels was similar in the two anesthetized groups, it was unlikely to have contributed to the differences observed in diaphragm alterations between spontaneous breathing and mechanically ventilated rats. In fact, the same decrease in calcium serum levels seen in the two anesthetized groups is probably related to the anesthesia/surgical procedure. In humans undergoing surgery under general anesthesia, hypocalcemia has been shown to be proportional to the severity of the anesthesia and surgical procedure [24]. On the other hand, because anesthetized animals (spontaneously breathing or mechanically ventilated) were receiving enteral nutrition during the 24-h duration of the study, they were unlikely to suffer from undernutrition. It is well known that acute undernutrition may alter diaphragm force. In fact, we previously demonstrated that while short-term undernutrition reduced diaphragmatic force in rats, it did not alter IGF-I mRNA levels in this muscle [18]. Thus, decreased diaphragmatic force and IGF-I mRNA as shown in the present study are unlikely to result from undernutrition. Finally, due to the fact that study duration was limited to 24 h, the potential development of infection is unlikely as confirmed by the absence of fever.
In agreement with previous studies of animal models of mechanical ventilation [12, 14, 13, 10], the present study further confirmed that although the effects of anesthesia and its consequences were significantly less pronounced than those observed after mechanical ventilation, they were, however, significantly different from true controls. In fact, pentobarbital anesthesia is well known to induce a reduction in skeletal muscle force [25, 26], including the diaphragm [27]. This inhibitory effect of pentobarbital might be related to the impairment of excitation-contraction coupling and/or the decrease in blood flow to the diaphragm [27]. In addition, anesthesia may have altered respiratory mechanics and diaphragm geometry, which, in turn, may have contributed to the diaphragm dysfunction seen in the present study. In humans, anesthesia has been shown to alter functional residual capacity by affecting the rib cage rather than diaphragm position (for a review see [28]). A comprehensive discussion of the exact mechanisms involved in this process is, however, beyond the scope of the present study.
Interestingly, the effects of mechanical ventilation reported in the present study were not solely due to anesthesia and associated effects in accordance with the data of others [10, 12, 14, 13], as significant differences were obtained between spontaneously breathing animals and mechanically ventilated animals. Importantly, these differences were also not related to differences in anesthesia infusion since animals were receiving the same amount of anesthesia. As previously reported, the safety dose of sodium pentobarbital is extremely narrow and the animals could be easily overdosed [26] resulting in a large mortality in our study. These differences were also not related to differences in breathing pattern since blood gases were similar between spontaneously breathing animals and mechanically ventilated animals. Finally, although mortality was high especially in spontaneous breathing rats, it seems unlikely that mortality did affect the selection of the animals and hence, the present data. Therefore, it seems reasonable to assume that the effects of mechanical ventilation on the diaphragm's intrinsic properties observed in our study are related to mechanical ventilation itself.
Several attempts have been made to examine the effects of mechanical ventilation on muscle function in animals and interest in these models has been recently revived. These animal studies showed that, in rats, diaphragm force was already reduced after 12 h of mechanical ventilation, the magnitude of these effects increasing with the time spent on the ventilator [12]. Along the same lines, a time-dependent decline in rabbit diaphragmatic function was also reported such that transdiaphragmatic pressure during phrenic nerve stimulation already decreased after 1 day of controlled mechanical ventilation while myofibril damage was observed after 3 days [13]. In none of these studies, was loss of diaphragm mass present. The data of the present study further confirmed that short-term mechanical ventilation, independently of anesthesia and surgical procedure, significantly altered diaphragm function while diaphragm mass remained the same. However, when mechanical ventilation was prolonged up to 4 days, and was combined with antibiotics and paralyzing agents, diaphragm weight was reduced and diaphragm fibers co-expressing MHC-I and II increased at the expense of the MHC-I population [10]. In models where anesthesia and surgical procedure effects on diaphragm function were not controlled, similar results were observed. Thus, in rats, diaphragmatic force and mass were reduced after 48 h of mechanical ventilation [9] while in piglets, 5 days mechanical ventilation was shown to affect diaphragm activation with no changes in nerve conduction and neuromuscular transmission in addition to decreased diaphragm contractility [11]. Finally, 11 days of mechanical ventilation in baboons were associated with a decrease in maximal diaphragmatic strength and endurance capacity [8].
Concerning intrinsic adaptations of the diaphragm to mechanical ventilation, a decrease in the cross-sectional area of all diaphragm fiber types was first described by Shanely et al. [14]. Because type II fibers were mainly affected, the relative contribution of type I to total cross-sectional area was increased. This effect was already observed after 18 h of controlled mechanical ventilation and fiber distribution remained unchanged. In our study, similar results were obtained after 24 h except that atrophy was similarly distributed among the different fiber types. This may suggest that prolongation of mechanical ventilation would homogenize diaphragm fiber adaptation among the different types. However, caution should be excercised as female rats, rather than male rats, were used in the study of Shanely et al. [14] as compared to our study, and in which the species was also different (Sprague-Dawley vs Wistar). Thus, gender and/or species may also have contributed to the differences in the distribution of the effect on diaphragm fiber types. Indeed, we previously reported that both fiber distribution and dimensions were significantly different in male and female rats of the same age within the Wistar species [29].
Neither in the study of Shaneley et al. [14], nor in the present study was this decrease in diaphragm fiber dimensions associated with a decrease in diaphragm mass. However, in the present study a decrease in IGF-I mRNA levels observed in the diaphragm after mechanical ventilation suggests that an atrophy process was already present that would probably result over time in diaphragm muscle wasting. In fact, we previously showed a link between diaphragm mass and local production of IGF-I mRNA such that diaphragm atrophy after corticosteroid treatment was associated with decreased diaphragm IGF-I mRNA [18]. This decrease of IGF-I mRNA in the diaphragm after mechanical ventilation has never been shown before and is of conceptual interest. This decrease shows that early alterations already occur in the diaphragm after only 24 h mechanical ventilation. As IGF-I has been shown to stimulate protein synthesis and to decrease protein degradation [30], any decrease in its expression is expected to lead to enhanced muscle protein breakdown and hence, to muscle atrophy. Our data therefore suggest that mechanical ventilation, by impairing IGF-I expression in the diaphragm, may precipitate diaphragm atrophy, this phenomenon being present after short-term mechanical ventilation. This hypothesis is also supported by the recent data of Shanely et al. [14] showing that after 18 h of controlled mechanical ventilation, diaphragm protein degradation is, indeed, increased and this diaphragmatic proteolysis was mediated by both the calpain and proteasome systems. Interestingly, IGF-I has been shown to exert its anti-proteolytic action by decreasing the expression of the enzymes of the proteasome ubiquitin pathway [19]. Thus, it is possible that the decrease in IGF-I mRNA we observed after mechanical ventilation may lead to decrease in IGF-I peptide such that proteasome activity increases and diaphragmatic proteolysis develops. However, whether the decrease IGF-I mRNA in the diaphragm leads to a decrease in IGF-I peptide within the diaphragm still remains to be determined.
Conversely, the potential role of IGF-I in the diaphragm alterations seen in the present study is further underlined by the fact that a significant positive correlation was found between the levels of IGF-I mRNA in the diaphragm and its force production. The physiological mechanisms to explain how the decreased IGF-I mRNA levels in the diaphragm may cause a decrease in its force production are not known. More specifically the relationship between mRNA levels and force production is not obvious. It should, however, be kept in mind that force production is related to muscle fiber composition. Thus, any alteration in fiber distribution or dimension is likely to result in alterations in force production. For myostatin (another growth factor expressed in skeletal muscle), data exist showing that a relationship between its mRNA levels and muscle contractile protein content is present, suggesting a potential link between growth factor mRNA levels and muscle force [31]. However, the mechanism by which IGF-I may cause diaphragmatic force to be reduced is likely to be related to loss in diaphragm protein content. In fact, IGF-I is known to stimulate protein synthesis and to decrease protein degradation. Thus, it might be possible that the decrease in IGF-I expression seen in the diaphragm after controlled mechanical ventilation may disturb the rate of protein dynamics such that contractile protein may be more degraded and hence diaphragm force may be less. Recently, Shanely et al. [14] demonstrated that in rats 18 h of controlled mechanical ventilation resulted in loss of diaphragmatic protein content with no change in diaphragm mass (as water content increased) and this reduction was likely to contribute to the reduction in diaphragmatic force seen after mechanical ventilation.
The mechanism by which mechanical ventilation may lead to alterations in diaphragm function remains to be established. However, several hypotheses may be suggested. While the aim of mechanical ventilation is to unload the respiratory muscles, resting the diaphragm and thus making the diaphragm inactive probably leads to a certain level of deconditioning that may have contributed to the observed alterations. Moreover, mechanical ventilation, in addition to making the diaphragm inactive, shortens the diaphragm passively and rhythmically. This passive shortening may impair diaphragm function and may therefore be involved in the changes observed in the present study after mechanical ventilation. Along the same lines, biotrauma may have been caused by mechanical ventilation as mechanical stress to the lungs may have led to upregulation of inflammatory response and lung injury (for a review, see [7]). Whether, and to what extent, inactivation of the diaphragm, passive shortening or biotrauma are responsible for the diaphragm alterations seen in the present study after mechanical ventilation still needs to be determined.
The data of the present study are, however, of conceptual interest for clinical medicine as they clearly show that, independently of anesthesia and resulting effects, early alterations in diaphragm function develop after 24 h of mechanical ventilation. In particular, it is important to mention that the present study was performed on rats with normal diaphragm function in whom 24 h of mechanical ventilation already induced pronounced alterations in their normal diaphragm. If mechanical ventilation is applied to animals with already impaired diaphragm function, it would probably result in more severe changes in the diaphragm's intrinsic properties. Whether these alterations are involved in the weaning difficulties seen in patients under mechanical ventilation still needs to be determined.
References
Tahvanainen J, Salmenpera M, Nikki P (1983) Extubation criteria after weaning from intermittent mandatory ventilation and continuous positive airway pressure. Crit Care Med 11:702–707
Jabour ER, Rabil DM, Truwit JD, Rochester DF (1991) Evaluation of a new weaning index based on ventilatory endurance and the efficiency of gas exchange. Am Rev Respir Dis 144:531–537
Krachman SL, Martin U, D'Alonzo GE (2001) Weaning from mechanical ventilation: an update. J Am Osteopath Assoc 101:387–390
Sporn PH, Morganroth M (1988) Discontinuation from mechanical ventilation. Clin Chest Dis 9:113–126
Zakynthinos SG, Vassilakopoulos T, Roussos C (1995) The load of inspiratory muscles in patients needing mechanical ventilation. Am J Respir Crit Care Med 152:1248–1255
Goldstone JC, Green M, Moxham J (1994) Maximum relaxation rate of the diaphragm during weaning from mechanical ventilation. Thorax 49:54–60
Dos Santos CC, Slutsky AS (2000) Cellular responses to mechanical stress. Invited review: mechanisms of ventilator-induced lung injury: a perspective. J Appl Physiol 89:1645–1655
Anzueto A, Peters JI, Tobin MJ, De Los Santos R, Seidenfeld JJ, Moore G, Cox WJ, Coalson JJ (1997) Effect of prolonged controlled mechanical ventilation on diaphragmatic function in healthy adult baboon. Crit Care Med 25:1187–1190
Le Bourdelles G, Viirès N, Boczkowski J, Seta N, Pavlovic D, Aubier M (1994) Effects of mechanical ventilation on diaphragmatic contractile properties in rats. Am J Respir Crit Care Med 149:1539–1544
Yang L, Luo J, Bourdon J, Lin MC, Gottfried SB, Petrof BJ (2002) Controlled mechanical ventilation leads to remodelling in the rat diaphragm. Am J Respir Crit Care Med 166:1135–1140
Radell PJ, Remahl S, Nichols DG, Eriksson LI (2002) Effects of prolonged mechanical ventilation and inactivity on piglet diaphragm function. Intensive Care Med 28:358–364
Powers SK, Shaneley RA, Coombes JS, Koesterer TJ, McKenzie M, Van Gammeren D, Cicale M, Dodd SL (2002) Mechanical ventilation results in progressive contractile dysfunction in the diaphragm. J Appl Physiol 92:1851–1858
Sassoon CSH, Caiozzo VJ, Manka A, Sieck GC (2002) Altered diaphragm contractile properties with controlled mechanical ventilation. J Appl Physiol 92:2585–2595
Shanely RA, Lennon SL, Yimlamai T, Dodd S, Zergeroglu AM, Sugiura T, Enns D, Belcastro A, Powers SK (2002) Mechanical ventilation-induced diaphragmatic atrophy is associated with oxidative injury and increased proteolytic activity. Am J Respir Crit Care Med 165:1369–1374
Adams GR, Haddad F (1996) The relationships among IGF-I, DNA content, and protein accumulation during skeletal muscle hypertrophy. J Appl Physiol 81:2509–2516
Adams GR, McCue SA (1998) Localized infusion of IGF-I results in skeletal muscle hypertrophy in rats. J Appl Physiol 84:1716–1722
Goldspink G (1999) Changes in muscle mass and phenotype and the expression of autocrine and systemic growth factors by muscle in response to stretch and overload. J Anat 194:323–334
Gayan-Ramirez G, Vanderhoydonc F, Verhoeven G, Decramer M (1999) Acute treatment with corticosteroids decreases IGF-I and IGF-II expression in the rat diaphragm and gastrocnemius. Am J Respir Crit Care Med 159:283–289
Chrysis D, Zhang J, Underwood LE (2002) Divergent regulation of proteasomes by insulin-like growth factor I and growth hormone in skeletal muscle of rats made catabolic with dexamethasone. Growth hormone, IGf research 2002:434–441
Yang H, Alnaqeeb M, Simpson H, Goldspink G (1997) Changes in muscle fibre type, muscle mass and IGF-I gene expression in rabbit skeletal muscle subjected to stretch. J Anat 190:613–622
Dekhuijzen PNR, Gayan-Ramirez G, De Bock V, Dom R, Decramer M (1993) Triamcinolone and prednisolone affect contractile properties and histopathology of rat diaphragm differently. J Clin Invest 92:1534–1542
Chirgwin JM, Przybyla AE, McDonald RJ, Rutter WJ (1979) Isolation of biologically active ribonucleic acid from sources enriched in ribonuclease. Biochemistry 18:5294–5299
Aubier M, Viirès N, Piquet J, Murciano D, Blanchet F, Marty C, Gherardi R, Pariente R (1985) Effects of hypocalcemia on diaphragmatic strength generation. J Appl Physiol 58:2054–2061
Lepage R, Légaré G, Racicot C, Brossard J-H, Lapointe R, Dagenais M, D'Amour P (1999) Hypocalcemia induced during major and minor abdominal surgery in humans. J Clin Endocrinol Metab 84:2654–2658
Taylor RG, Abresch RT, Lieberman JS, Fowler WR, Portwood MM (1984) Effect of pentobarbital on contractility of mouse skeletal muscle. Exp Neurol 83:254–263
Ingalls CP, Warren GL, Lowe DA, Boorstein DB, Armstrong RB (1996) Differential effects of anesthetics on in vivo skeletal muscle contractile function in the mouse. J Appl Physiol 80:332–340
Fujii Y, Hoshi T, Takahashi S, Toyooka H (1999) Propofol decreases diaphragmatic contractility in dogs. Anesth Analg 89:1557–1560
Warner DO (1994) Anaesthesia and chest wall function. Ann Acad Med Singapore 23:566–571
Bisschop A, Gayan-Ramirez G, Rollier H, Dekhuijzen PNR, Dom R, De Bock V, Decramer M (1997) Effects of nandrolone decanoate on respiratory and peripheral muscles in male and female rats. J Appl Physiol 82:1112–1118
Ballard FJ, Read LC, Francis GL, Bagley CJ, Wallace JC (1986) Binding properties and biological potencies of insulin-like growth factors in L6 myoblasts. Biochem J 233:223–230
Carlson CJ, Booth FW, Gordon SE (1999) Skeletal muscle myostatin mRNA expression is fiber-type specific and increases during hindlimb unloading. Am J Physiol 277: R601-R606
Acknowledgement
The authors sincerely thank Dr Naima Viirès for her helpful and relevant advice regarding the experimental set-up.
Author information
Authors and Affiliations
Corresponding author
Additional information
G Gayan-Ramirez is postdoctoral fellow of the "Fonds voor Wetenschappelijk Onderzoek-Vlaanderen" (FWO-Vlaanderen). This study was supported by the "Fonds voor Wetenschappelijk Onderzoek-Vlaanderen" grant G.0237.01 and G.0389.03, KULeuven Research Foundation OT 98/27 and 02/44, and AstraZeneca Pharmaceuticals.
Rights and permissions
About this article
Cite this article
Gayan-Ramirez, G., de Paepe, K., Cadot, P. et al. Detrimental effects of short-term mechanical ventilation on diaphragm function and IGF-I mRNA in rats. Intensive Care Med 29, 825–833 (2003). https://doi.org/10.1007/s00134-003-1688-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-003-1688-0