Abstract
Purpose
Deinstitutionalization of persons living with mental illness has led to many patients residing in communities with family members and shifting the burden of care and caregiving from hospitals to homes. The aim of the study was to determine the burden on caregivers of patients with schizophrenia at Edward Francis Small Teaching Hospital (EFSTH).
Methods
This was a descriptive cross-sectional study design with a sample consisting of 161 randomly selected caregivers of patients with schizophrenia. The GHQ-12 questionnaire was used to determine the general health status of the caregivers. The caregivers’ burden was assessed using the Zarit Burden Scale. The data were collected using the researcher-administered method. The collected data were analyzed with IBM SPSS Version 20 using descriptive statistics, mean differences, and the general linear model (GLM).
Results
The main findings of this study were that caregivers experienced a significantly high level of burden. Most of them experienced high levels of physical (70%), psychological (93.2%), social (78.3%) and financial (55.3%) burdens. Employment status, specifically unemployment status and belonging to the Wolof ethnic group, was a significant predictor of the level of financial burden on the caregivers. Similarly, the total score for social burden was also significantly greater among unemployed caregivers. Educational level was a significant predictor of the total score on the psychological and physical burden scale.
Conclusion
The caregivers of patients with schizophrenia at EFSTH are experiencing a high level of burden as a result of their caregiving role, which affects their health, and this calls for urgent intervention.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The World Health Organization has estimated that mental illness incidence is increasing worldwide and is a public health dilemma [1]. Published WHO data also revealed that at least 40 million people globally suffer from mental disorders such as schizophrenia and dementia. Schizophrenia is the most prevalent chronic and severe psychotic disorder and is increasingly recognized as a systemic disorder found in all societies and geographical areas [2, 3] and uniform across cultures [4]. Moreover, the WHO reported that 23 million people suffer from schizophrenic disorders [5]. Approximately, 1% of the global population is affected by schizophrenia, and 60% of those affected range from moderate to severe [6].
Schizophrenic disorders affect how a person thinks, feels, and behaves, and this makes the individual interpret reality abnormally [7]. Many patients living with schizophrenia also suffer from substantial comorbidities and poor overall health habits, including personal neglect as well as alcohol and other psychoactive substance abuse [2]. However, the deinstitutionalization of persons with mental illness has led to many patients residing in communities with family members. Thus, the burden of care and caregiving has shifted from hospitals to homes [8, 9]. People who suffer from schizophrenia are dependent on family members, who are the primary or principal caregivers. These caregivers have multiple needs that are extensive and vary across cultures [10, 11]. According to Chakrabarti and Kulhara, the burden of caregivers in terms of scales and scores is greater for patients with schizophrenia than for those with other chronic psychiatric disorders [12]. A study on caregivers’ burdens revealed concerns about physical, psychological, social, and financial burdens [13].
The psychiatric outpatient department of EFSTH is the only fully functional clinic for patients with psychiatric problems in The Gambia. Schizophrenia is the second highest recorded number of patients seen in this clinic, thus raising concern among hospital authorities (Tanka-Tanka, annual reports from 2014 to 2020). According to a study conducted in The Gambia, the most common disorders leading to admission are substance misuse (most frequently cannabis misuse), schizophrenia, organic psychoses, and affective disorders [14]. Similarly, community data revealed that 48% of mental health burdens are associated with schizophrenia, 23% with epilepsy, 16% with substance misuse, 3.4% with depressive disorders, 4.9% with anxiety disorders, 1.6% with dementia and 0.4% with postmalaria neurological symptoms [13].
Although there is limited information on the burden of caregivers of patients with schizophrenia in the Gambia, clinical observation has shown that caregivers frequently experience psychological breakdowns, societal discrimination, stigmatization, and financial problems (buying medication and other needs) as a result of caring for their patients. Psychiatric/mental health services and treatment are free of charge in The Gambia, but there is usually a frequent shortage of antipsychotics. The caregivers or patients themselves frequently face situations where they are expected to buy antipsychotic medications, which can be very expensive for the average Gambian. In addition, caregivers usually visit the clinic monthly for continuous follow-up appointments, during which many of them have to travel from their homes and pay transportation fares for themselves and their patients. The outdated Suspected Lunatics Detention Act of 1964 is still in use in The Gambia, which does not accommodate all of the patients’ human rights or their primary family caregivers in terms of social, psychological, and financial support. In 2004 and 2015, the Ministry of Health of The Gambia recognized that the Act was outdated, so a new Mental Health Act and Policy and Strategic Action Plan was drafted in 2015, but the updated version has yet to be sent to the parliament for ratification and adaptation. Despite this experience in the Gambia, patients with psychotic disorders and caregivers in the community are not catered for in many areas of the long-term care systems [15]. Hence, this study was conducted to investigate the burden of caregivers of patients with schizophrenia reporting at the polyclinic psychiatric outpatient unit of EFSTH. The findings of this study can be used to guide policy and practice interventions to meet the needs of this vulnerable group.
Methods
Research design and setting
This research used a descriptive cross-sectional study design on caregivers of patients with schizophrenia. The study was conducted at Edward Francis Small Teaching Hospital (EFSTH), Banjul, which is the only teaching and main referral hospital in Gambia. It has seven departments, namely Obstetrics and Gynecology, Pediatrics, Accident and Emergency Unit, Internal Medicine, Surgery, Ophthalmology, and Psychiatry. The Polyclinic is a sub outpatient department of EFSTH and has 17 units with 68 staff, 16 trained staff, and 52 support staff. The polyclinic psychiatric department is the only main referral unit in the country. The outpatient unit of the EFSTH is where patients with psychiatric disorders are seen as outpatients and inpatients are referred to the Tanka-Tank Psychiatric Department for admission when necessary. It operates from 8 am to 2 pm, but only the medical outpatient operates for 24 h.
Research population and eligibility criteria
The research target population was caregivers of registered patients with schizophrenia diagnosed at the polyclinic outpatient psychiatric unit of EFSTH. These patients were diagnosed with schizophrenia according to the criteria established by the International Classification of Disorders-10. The inclusion criteria for participating in this study were a person who was caring for a patient diagnosed with schizophrenia not less than a year, registered in the EFSTH polyclinic psychiatric unit, and have not less than two previous psychotic episodes. The study participant must also be 18 years or older, consented to mental health assessment to exclude any mental illness, have lived with a person diagnosed with schizophrenia for no less than 6 months, and involved in the caregiving activities.
Sample size and sampling technique
Using Cochran’s single population proportion formula [16], the minimum estimated sample size at the 95% confidence interval, 5% level of significance, and 10% for nonresponse was 161 respondents.
Caregivers of patients with schizophrenia were approached to participate in the study. Those who accepted the invitation were screened for mental illnesses before they were recruited. Simple random sampling with a replacement method was used to select the study participants (caregivers).
Research tool
The research tools used were a sociodemographic questionnaire, a 12-item version of the General Health Questionnaire (GHQ-12), and the Zarit Burden Interview (ZBI) scale [17, 18].
The ZBI is a 25-item questionnaire with a five-item response set ranging from 0 = ‘never’ to 4 = ‘nearly always’. Item scores are summed to give a total score ranging from 0 to 100, with higher scores indicating greater burden [19]. A total score lower than 50 was considered to indicate a low burden, and a score ranging from 51 to 100 was considered to indicate a high burden. This scale was further divided into four subscales: the financial burden subscale, which has 6 items; the social burden subscale, which has 7 items; the psychological burden subscale, which has 6 items; and the physical burden subscale, which has 6 items.
The 12-item General Health Questionnaire (GHQ-12) has been widely used for screening and detecting psychological morbidity and mental disorders in caregivers [20,21,22,23]. The GHQ-12 consists of 12 items, each with four responses, typically ‘not at all’, ‘no more than usual’, ‘rather more than usual’, and ‘much more than usual’. The total possible score for general health was 48, a total score lower than 24 was classified as poor, and 24–48 was good health status.
Validity and reliability of the research tool
Several studies have adopted the questionnaire and reported it to be reliable [17, 18, 21, 24]. However, because the questionnaire was modified to suit the study context and objectives, three experts (a psychiatrist, a mental health nurse, and a researcher) were consulted to determine the content and face validity. Each item of the questionnaire was reviewed for clarity, relevance, and cultural sensitivity. In addition, a content validity index formula was used to calculate the validity of the tool:
Since the results of the validity test were above 0.70, the research instrument was considered valid [25].
Sixteen caregivers of patients with schizophrenia at Kanifing General Hospital and Brikama District Hospital were also pilot tested; these patients were not included in the main study. To measure the reliability of the research tool, the Cronbach alpha coefficient was used to test the constructs used to measure the variables under study using the split-half method. The results showed that the Cronbach’s alpha value of the ZBI scale was 0.79 and that of the 12-item General Health Questionnaire was 0.84. The total reliability of the questionnaire was 0.81, which is above the 0.7 acceptable reliability level for a research instrument recommended by Ref. [26].
Data collection procedure
The researchers conducted the interviews together with a research assistant who was trained on how to conduct the interviews. The study respondents were interviewed in Gambian national languages, mainly Mandinka, Wolof, and Fula. The reason why the interview was in the national language is because most Gambians speak at least one of these languages. Thus, there was oral translation from English to these national languages. The data collection lasted for 3 months.
Data analysis
IBM Statistical Package for Social Sciences (SPSS) software, version 20, was used for the data analysis. The results are presented as the frequency for categorical variables and mean and standard deviation for continuous variables. T tests and ANOVAs were used to test for differences in the levels of burden according to the demographic characteristics of the caregivers. The Bonferroni post hoc correction was used to determine where the variability of outcome variables occurred between three or more independent variables. GLM multivariate regression was used to test the sociodemographic variables predicting the level of burden on the caregivers.
Levene’s test was used to test the homogeneity of the independent variables, while the spread versus level plot was used to test for the normal distribution of the data before conducting ANOVA and t tests. Levene’s test results for all the analyses were not significant, indicating that the assumption of homogeneity of variance had been met. Before running the regression analysis, the categorical independent variables (sociodemographic variables) used as predictors of the outcome variables were transformed into dummy variables. The assumptions of normality, linearity, and multicollinearity were tested using the variance inflation factor (VIF) and Pearson correlation tests. The limit for any variable to be added to the model was set at a VIF > 5; when two variables had a correlation coefficient of 0.7 and above, only one was selected for the regression model (Corporate Finance Institute Team 2022). However, all variables were added to the GLM because all of them had VIFs less than 5 and correlation coefficients less than 0.7. The level of statistical significance was set at 95%, with a p value less than 0.05.
Ethical consideration
This research was approved by the Gambia Government/MRCG Joint Ethics Committee and the Research and Ethics Committee (REC) of EFSTH. The Gambia Government/MRCG Joint Project ID/Ethics ref: R021045 (14 June 2022). Research Ethics Committee (REC) Edward Francis Small Teaching Hospital: EFSTH_REC_2022_073 (July 29th, 2022).
Strengths and limitations of the study
The researchers are not aware of a similar study previously conducted in The Gambia; therefore, the findings of this study can serve as evidence and reference for guiding policy review and strategy development to accommodate the needs of the informal caregivers of people with chronic mental illness. The results of this study may be generalized to the entire population because the caregivers, and their patients came from different parts of the most populated areas of both rural and urban Gambia.
This study has some limitations. The effects of the duration of the patient’s illness, time spent with the patient, knowledge and awareness of the mental illness, medication adherence, and the effects of stigma and discrimination due to caregiving were not assessed.
Results
Sociodemographic of the study participants
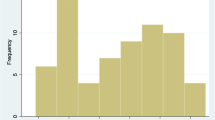
One hundred and sixty-one caregivers of patients with an ICD-10 diagnosis of schizophrenia were enrolled in the study, with a 100% response rate. Of the 161 caregivers interviewed, 84 (52.2%) were males, with a mean age of 44.98 years (SD = 15.294) and an age range of 18 to 82 years. Most of the participants were from the Mandinka tribe (n = 56; 34%), were married (n = 109; 67.7%), and 42 of them (26.1%) were siblings of the patients they were caring for. The majority of the caregivers (83.2%; n = 134) were from urban settlements, and 44% (n = 71) lived in a two-room house. Sixty-four (39.8%) had no formal education (Table 1).
Burden of the caregivers of schizophrenic patients
The burden of caregivers as a result of the caregiving role was measured using four domains as follows:
The physical burden of the caregivers of patients with schizophrenia
The caregivers reported experiencing general body pain (n = 66; 41.0%), exhaustion (n = 68; 42.2%), difficulty sleeping (n = 61; 37.9%), and joint pain (n = 50; 31.1%). In addition, 35.4% (n = 57) of the participants had lost their appetite quite frequently, and 31.1% (n = 50) had headaches sometimes. The majority of them (n = 125; 77.6%) reported experiencing a high level of physical burden (Table 2).
The psychological burden of the caregivers of patients with schizophrenia
The results of the analysis of the psychological burden presented in Table 3 show that the caregivers felt embarrassed because of patient behavior (n = 92; 57.1%), felt guilty about not doing enough (n = 107; 66.5%), felt trapped in a caregiving role (n = 145; 90.1%), were upset about patient change from the former self (n = 143; 88.8%), were worried about the future (n = 145; 90.1%), and were nearly always concerned about mental illness upsetting (n = 138; 85.7%). A high percentage (97.5%, n = 157) of them felt not responsible for causing the patient's illness. In general, 93.2% (n = 150) of the participants experienced a high level of psychological burden.
Social burden of caregivers of patients with schizophrenia
According to the results presented in Table 4, 41.0% (n = 66) of the caregivers indicated that they had less time to spend with friends, 65.8% (n = 106) had neglected other family members’ needs, and 26% (n = 41) experienced family frictions and arguments nearly always. A good number of them said that they cut leisure time (n = 70; 43.5%) and found household routine upsetting (n = 62; 38.5%) quite common. Only 41.0% (n = 66) of the caregivers had never experienced friction with neighbors, friends, or other relatives. In addition, 78.3% (n = 126) experienced high social burdens.
The financial burden of the caregivers of patients with schizophrenia
The results presented in Table 5 show that most of the caregivers (n = 100; 62.1%) had financial problems, 39.1% (n = 63) missed days of work, 37.3% (n = 60) experienced difficulty concentrating on work, and 84.5% (n = 136) experienced unexplained expenditures on treatment nearly always. However, 71.4% (n = 115) and 75.8% (n = 122) of the participants had never planned to take a new job and never lost their job, respectively (Table 4). For their grade of financial burden, 55.3% (n = 89) and 44.7% (n = 72) experienced high and low levels of financial burden, respectively.
General health status of caregivers of patients with schizophrenia
A total of 36% (n = 58) of the caregivers reported having health problems, 15.5% (n = 25) of whom were diagnosed with hypertension, diabetes (n = 5, 3.1%), or both hypertension and diabetes (n = 3, 1.9%). Twenty-nine percent (n = 46) of them reported that their current health status was poorer than that before they started their caring role.
Sociodemographic variables predicting the level of burden among caregivers
The results obtained from the GLM multivariate analysis are presented in Table 6. All the demographic variables were added to the GLM because all of them had VIFs less than 5 and correlation coefficients less than 0.7. However, only the sociodemographic variables that are statistically significant predictors of the total level of burden and general health status are shown in the table. The results showed that after all the demographic variables were included in the model, they accounted for 69% (R2 = 0.69, F = 112.15; p < 0.001) of the variation in the level of burden among the caregivers. Employment status, specifically self-employed status (β = 2.76, p = 0.02, 95% CI = 2.48–6.06), unemployed status (β = 4.27; p < 0.001, 95% CI = 2.48–6.06), and belonging to the Wolof ethnic group (β = 2.64, p = 0.04′ 95% CI = 0.03–5.24), were significant predictors of the level of financial burden on the caregivers. The total score for social burden was also significantly greater for unemployed caregivers (p = 0.02, 95% CI = -5.09 to -0.37), as they were three times more likely (β = 2.73) to report a high burden on them than their self-employed and employed counterparts were. Educational level was a significant predictor of the total psychological and physical burden score. Compared with caregivers with no education, those with a junior secondary school education had significantly lower levels of psychological (β = -2.26, p = 0.04, 95% CI = -5.38 to −0.14) and physical (β = -3.20, p = 0.03, 95% CI = -6.09 to −0.32) burdens.
Discussion
Sociodemographic characteristics of the study respondents
The sociodemographic profiles of the caregivers in this study were compared with those of an earlier study in Nigeria in which similar caregivers’ assessment instruments were utilized [8]. The findings from the study revealed that caregivers were generally older, had fewer years of education, and were unemployed more often. The high number of married caregivers included in this study was similar to that reported in other studies [27, 28]. However, many similar studies reported a greater number of female caregivers [27, 29], contrary to the findings of most of the caregivers being male (52.2%). The greater percentage of male caregivers in this study could be a result of the aggressive nature of most of the patients who need a male caregiver to help them reach the hospital.
Burden of Caregivers
The category with the largest proportion of caregivers’ burden in this study was psychological burden. This is not unforeseen considering the continuous salience of stigma and discrimination toward mental illness in The Gambia. A higher percentage of caregivers with psychological distress have been associated with a heavier caregiving burden [30]. Furthermore, the Gambia still uses outdated terms such as “Lunatic”, which refers to patients with psychotic disorders. Moreover, these findings are in accordance with the stress-process model’s test of caregivers of people living with schizophrenia [31]. Another study in Nigeria reported that caregivers felt depressed, weepy, and irritable [8].
The second largest category of burden recorded was “social burden,” with a high grade of 126 (78.3%). This could be a consequence of the negative societal outlook of people who have mental illness and their families. Society still perceives and believes that mental illness results from bad omens, black magic, witchcraft, a family's dark heritage, and so on. It has been noted that many societies associate the caregiving role with some ‘taboo’ [32]. Caregivers often discern from society and experience grief due to societal issues associated with mental health problems, with repercussions such as feelings of disesteem, embarrassment, and/or guilt [33]. This study revealed that most of the caregivers nearly always neglected other family members’ needs, frequently had less time to spend with friends, and lessened their leisure time. Patients living with schizophrenia are more dependent on their caregivers disrupting family routines [34].
Regarding the physical burden related to the caregiving role, most of them reported feeling exhausted, experiencing general body pain, difficulty sleeping, and experiencing joint pain. Some caregivers also reported headaches and loss of appetite. One study showed that caregivers, especially older caregivers, were significantly more likely to have physical health problems and, notably, physical deterioration [8].
The financial burden reported by caregivers in this study is worrisome. This study revealed the hidden expenditures involved in psychiatric treatment, which are assumed to be free of charge in the Gambia. The majority reported unplanned expenditures on buying antipsychotic drugs and transporting patients for treatment appointments, and more than half reported nearly always missed days of work. The Gambia does not have a national health insurance scheme, and the government does not have any avenue or sector responsible for such caregivers’ needs in providing care to patients living with chronic conditions such as schizophrenia. The out-of-pocket expenses for treatment in nations such as Gambia, where the national health profile is still below the baseline health financing recommended by the WHO and deterioration since the COVID-19 pandemic emerged, are demanding. The present study supports the suggestion that long-term caregiving for patients with schizophrenia could give rise to caregivers’ financial difficulties, which is consistent with the findings of similar studies [8, 29]. In addition, caregivers find it difficult to maintain certain jobs while taking care of patients with schizophrenic disorders whose illness may be life-long, leading to poor financial status [34, 35].
This study revealed that 46 (28.6%) participants had poorer health than they did before they assumed their caregiving role. Although conflicting findings exist [36], several studies have revealed negative consequences of this burden on both the physical and mental health of caregivers [8, 37,38,39]. The stressful effect of caring for a chronically ill relative could be the cause of hypertension and/or diabetes among caregivers. In a case‒control study of schizophrenia spectrum and bipolar disorders and their matched controls, Pittsburgh Sleep Quality Index scores were worse for caregivers of patients with schizophrenia, which could trigger hypertension [40]. A high caregiver burden in terms of general health status is likely associated with a high risk of mental disorders; hence, medical, psychological, and social therapeutic interventions are needed in an attempt to lessen cases of chronic noncommunicable diseases, including mental health problems. This, therefore, requires policies and interventions centered on furnishing and funding programs that will target social and occupational rehabilitation for patients, as well as psychoeducational programs and psychosocial support for their informal caregivers. Synergetic efforts and the dynamic involvement of government agencies, nongovernmental organizations/institutions, and other relevant stakeholders will support fruition.
Associations between sociodemographic variables and caregivers’ burden
This study revealed that sex was significantly correlated with caregivers’ level of burden. Categorically, female caregivers had greater physical burden scores and poorer health status than male caregivers did. However, men had a greater financial burden than women. These results align with those of a similar study [41]. This could be due to females being especially traditional and religiously seen as carers, especially to ill family members. In other studies, sex was significantly correlated with social performance, with males exhibiting greater deficits than females [42]. Sharma et al. [43] stated that globally, women are predominantly caregivers of relatives living with chronic medical conditions or disabilities, including aged individuals and adults with mental illnesses, and in some societies, cultural norms place the burden of caregiving on women. The greater financial burden among men, specifically among those who were self-employed or employed, found in this study may be due to the Gambian culture, which expects men to be the financial providers of their families. Furthermore, the findings from this study indicate that unemployed and self-employed caregivers reported greater burdens of social, psychological, and physical burdens than did employed caregivers, which is contrary to the findings of a study [8], in which employed respondents reported greater burdens than unemployed individuals. The Gambia is a low-resource country, and unemployed caregivers may find it practically impossible to cater to all their patients' needs, which can increase the burden on them.
The presence of Wolof ethnicity was a significant predictor of the level of financial burden on the caregivers in this study. Ethnicity and cultural differences can influence the subjective burden of caregiving [34].
This study examined the association between marital status and caregiver burden and revealed that widowed and divorced caregivers had significantly greater burdens than did their married counterparts. This may be because widowed and divorced caregivers do not have enough support in caregiving for their loved ones. These individuals can be discriminated against by society, which adds to care-related burdens. This study revealed that the relationships of patients, especially those whose offspring or siblings were affected, were more burdensome.
With respect to education level and caregiver burden, this study revealed a significant association between a low level of education (never been to school) and caregiver burden. A lower level of education could account for a lower perception of the complexities of caregiving and the level of understanding of patients’ conditions (diagnosis and prognosis). In addition, individuals who are not educated may find it difficult to have a good pay job (low income); thus, they are unable to finance necessary needs. The low educational status of caregivers may be socially, psychologically and financially disadvantageous. Other studies have shown significant associations between low levels of education and low or inadequate income, caregiver burden, and socioeconomic status [8, 29]. In addition, household income correlated with caregiver burden in another study [44].
Conclusion
This study revealed a high level of burden among the caregivers of patients with schizophrenia at the EFSTH Hospital, The Gambia. This finding shows that schizophrenia affects not only patients but also their vulnerable informal caregivers. Therefore, there is an urgent need for mental healthcare services in the Gambia to provide interventions that will promote the well-being of these caregivers.
Recommendations
The high level of burden found among caregivers of patients with schizophrenia in this study shows that the health systems of The Gambia should conduct a thorough assessment of caregivers’ needs, coping strategies, interpersonal skills, and social resources to develop and implement targeted interventions to decrease this burden. The findings of this study can be used to guide the review of the Mental Health Policy and Act of the Gambia to cater to the needs of caregivers of patients with mental illnesses. Psychosocial education, support groups, and individual caregiver counseling programs should be developed and incorporated into the mental health services of the country. A longitudinal study can be conducted to investigate the effects of the burden and coping mechanisms of caregivers over time. An interventional study testing the effectiveness of family psychoeducation programs in alleviating the burden of caregivers is also recommended.
References
Firoz AH, Karim ME, Alam MF, Rahman AH, Zaman MN, Chandra V. Community Based Multicentric Service Oriented Research on Mental Illness with focus on Prevalence. Medical Care, Awareness and Attitude towards Mental Illness in Bangladesh. Bangladesh Journal of Psychiatry. 2006;20:9–32. Accessed at https://www.researchgate.net/publication/274066561_Prevalence_medical_care_awareness_and_attitude_towards_mental_illness_in_Bangladesh. Accessed date: October 2022.
Šimunović Filipčić I, Filipčić I. Schizophrenia and physical comorbidity. Psychiatria Danubina. 2018 Jul 22;30(suppl. 4):152–7. Accessed at: https://pubmed.ncbi.nlm.nih.gov/29864751/. Accessed date: October 2022.
Owen MJ Sawa A Mortensen PB Schizophrenia. Lancet. 2016; 388: 86-97. https://doi.org/10.1016/S0140-6736(15)01121-6.
Mahariba K, Vijayalakshmi K, Anuradha C, Venkatesan L. Predictors of family burden among patients with schizophrenia. TNNMC J Mental Health Nurs. 2019;7(1):11–6. Accessed at: https://www.indianjournals.com/ijor.aspx?target=ijor:tnnmcjmhn&volume=7&issue=1&article=002. Accessed date: October 2022.
World Health Organization (WHO). (2018). Mental disorders fact sheet. 2016. View at: Publisher Site.
World Health Organization. Mental Health Action Plan 2013–2020. 2013 Geneva World Health Organization https://www.who.int/publications/i/item/9789241506021
Kotwal SB, Shitole SY. Schizophrenia: Its Complications and Treatments. 2019. Accessed at: https://ijisrt.com/assets/upload/files/IJISRT19DEC561.pdf. Accessed date: July, 2022
Lasebikan VO, Ayinde OO (2013) Family burden in caregivers of schizophrenia patients: Prevalence and sociodemographic correlates. Indian J Psychol Med 35(1):60–66. https://doi.org/10.4103/0253-7176.112205
Suro G, Weisman de Mamani AG. Burden, interdependence, ethnicity, and mental health in caregivers of patients with schizophrenia. Family Process. 2013 52(2):299–311. Fam Proc 52:299–311, 2013
Gutiérrez-Maldonado J, Caqueo-Urízar A, Kavanagh DJ (2005) The burden of care and general health in families of patients with schizophrenia. Soc Psychiatry Psychiatr Epidemiol 40:899–904. https://doi.org/10.1007/s00127-005-0963-5
Jagannathan A, Thirthalli J, Hamza A, Hariprasad VR, Nagendra HR, Gangadhar BN (2011) A qualitative study on the needs of caregivers of inpatients with schizophrenia in India. Int J Soc Psychiatry 57(2):180–194. https://doi.org/10.1177/0020764009347334
Chakrabarti S, Kulhara P. Family burden of caring for people with mental illness. The British Journal of Psychiatry. 1999 174(5):463- https://doi.org/10.1192/S0007125000262430
Von Kardorff E, Soltaninejad A, Kamali M, Eslami SM (2016) Family caregiver burden in mental illnesses: The case of affective disorders and schizophrenia–a qualitative exploratory study. Nord J Psychiatry 70(4):248–254. https://doi.org/10.3109/08039488.2015.1084372
Kretzschmar I, Nyan O, Mendy AM, Janneh B (2012) Mental health in the Republic of The Gambia. Intern Psychiatry 9(2):38–40. https://doi.org/10.1192/S1749367600003076
World Health Organization. Mental Health Atlas 2017 member state profile. World Health Organization, Geneva. 2017. Accessed at: https://www.who.int/publications/i/item/9789241514019. Accessed date: October, 2022
Cochran WG. Sampling techniques. John Wiley & Sons; 1977. Accessed at https://www.academia.edu/29684662/Cochran_1977_Sampling_Techniques_Third_Edition. Accessed date: October, 2022
Zarit SH, Reever KE, Bach-Peterson J (1980) Relatives of the impaired elderly: correlates of feelings of burden. Gerontologist 20(6):649–655. https://doi.org/10.1093/geront/20.6.649
Zarit S, Orr NK, Zarit JM. The hidden victims of Alzheimer's disease: Families under stress. NYU Press; 1985.
Yap P. Validity and reliability of the Zarit Burden Interview in assessing caregiving burden. Ann Acad Med Singapore. 2010;39:758–63. Accessed at: https://tsaofoundation.org/doc/Zarit_Validation_Sin.pdf. Accessed date: July, 2022
Dada MU, Okewole NO, Ogun OC, Bello-Mojeed MA (2011) Factors associated with caregiver burden in a child and adolescent psychiatric facility in Lagos, Nigeria: a descriptive cross-sectional study. BMC Pediatr 11(1):1–6. https://doi.org/10.1186/1471-2431-11-110
Goldberg DP (1972). The Detection of Psychiatric Illness by Questionnaire: A Technique for the Identification and Assessment of Non-Psychotic Psychiatric Illness (Maudsley Monograph, 21). Oxford University Press. Accessed at https://www.scirp.org/reference/referencespapers?referenceid=1984248. Accessed date: October, 2022
Lee B, Kim Y. Factor structure of the 12-item General Health Questionnaire (GHQ-12) among Korean university students. Psychiatry Clin. Psychopharmacol. 2020 30(1). https://doi.org/10.5455/PCP.20200518112914
Liang Y, Wang L, Yin X (2016) The factor structure of the 12-item general health questionnaire (GHQ-12) in young Chinese civil servants. Health Qual Life Outcomes 14(1):1–9. https://doi.org/10.1186/s12955-016-0539-y
Anjara SG, Bonetto C, Van Bortel T, Brayne C (2020) Using the GHQ-12 to screen for mental health problems among primary care patients: psychometrics and practical considerations. Int J Ment Heal Syst 14:1–3. https://doi.org/10.1186/s13033-020-00397-0
Hamed Taherdoost. Validity and Reliability of the Research Instrument; How to Test the Validation of a Questionnaire/Survey in a Research. Intern J Acade Res Manage, 2016, 5 (3), 28–36, ISSN: 2296–1747. Accessed at: https://hal.science/hal-02546799/document. Accessed date: September, 2022
Nunnally JC. An overview of psychological measurement. Clinical diagnosis of mental disorders: A handbook. 1978:97–146. https://doi.org/10.1007/978-1-4684-2490-4_4
Shamsaei F, Cheraghi F, Bashirian S. Burden on family caregivers caring for patients with schizophrenia. Iran J Psychiatry. 2015 10(4):239. Accessed at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4801494/. Accessed date: October, 2022
Stanley S, Balakrishnan S, Ilangovan S. Psychological distress, perceived burden and quality of life in caregivers of persons with schizophrenia. J Mental Health. 2017 26(2):134–41 Accessed at: https://research.edgehill.ac.uk/ws/portalfiles/portal/21274725/Psychological_distress_perceived_burden_and_quality_of_life_in_caregivers_of_persons_with_schizophrenia.pdf. Accessed date: October, 2022
Inogbo CF, Olotu SO, James BO, Nna EO (2017) Psychiatric disorders amongst caregivers who are first-degree relatives of patients with schizophrenia. J Psychiatry Human Behav Sci 1(1):1. https://doi.org/10.11604/pamj.2017.28.284.11574
Cw Lam P, Ng P, Tori C (2013) Burdens and psychological health of family caregivers of people with schizophrenia in two Chinese metropolitan cities: Hong Kong and Guangzhou. Community Ment Health J 49:841–846. https://doi.org/10.1007/s10597-013-9622-6
Yu Y, Liu ZW, Li TX, Li YL, Xiao SY, Tebes JK (2020) Test of the stress process model of family caregivers of people living with schizophrenia in China. Soc Sci Med 1(259):113113. https://doi.org/10.1016/j.socscimed.2020.113113
Bastawrous M (2013) Caregiver burden—A critical discussion. Int J Nurs Stud 50(3):431–441. https://doi.org/10.1016/j.ijnurstu.2012.10.005
Kulhara P, Kate N, Grover S, Nehra R (2012) Positive aspects of caregiving in schizophrenia: A review. World J Ppsychiatry 2(3):43. https://doi.org/10.5498/wjp.v2.i3.43
Awad AG, Voruganti LN (2008) The burden of schizophrenia on caregivers: a review. Pharmacoeconomics 26:149–162. https://doi.org/10.2165/00019053-200826020-00005
McEvoy JP. The costs of schizophrenia. J Clin Psychiatry. 2007 68:4. Accessed at: https://pubmed.ncbi.nlm.nih.gov/18284271/. Accessed date: October, 2022
Mitchell D. Stress, coping, and appraisal in an HIV-Seropositive rural sample: a test of the goodness-of-fit hypothesis (Doctoral dissertation, Ohio University). Accessed at: https://www.teachertoolkit.co.uk/wp-content/uploads/2016/10/ohiou1103225821.pdf. Accessed date: October, 2022
Carretero S, Garcés J, Ródenas F, Sanjosé V. The informal caregiver's burden of dependent people: theory and empirical review. Arch Gerontol Geriatrics. 2009 49(1):74–9. Accessed at: https://core.ac.uk/download/pdf/71039891.pdf. Accessed date: May, 2022
Chang HY, Chiou CJ, Chen NS. Impact of mental health and caregiver burden on family caregivers’ physical health. Arch Gerontol Geriatrics. 2010 1;50(3):267–71. Accessed at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7114152/
Tennakoon L, Fannon D, Doku V, O'Ceallaigh S, Soni W, Santamaria M, Kuipers E, Sharma T. Experience of caregiving: relatives of people experiencing a first episode of psychosis. British J Psychiatry. 2000;177(6):529–33. Accessed at: https://pubmed.ncbi.nlm.nih.gov/11102328/. Accessed date: May, 2022
Fekih-Romdhane F, Mhedhbi N, Ben Ali S, Cheour M (2020) Sleep quality in caregivers of older patients with schizophrenia spectrum and bipolar disorders: A case-control study. Clin Gerontol 43(5):533–544. https://doi.org/10.1080/07317115.2019.1680588
Papastavrou E, Kalokerinou A, Papacostas SS, Tsangari H, Sourtzi P (2007) Caring for a relative with dementia: family caregiver burden. J Adv Nurs 58(5):446–457. https://doi.org/10.1111/j.1365-2648.2007.04250.x
Jenkins JH, Schumacher JG (1999) The family burden of schizophrenia and depressive illness: specifying the effects of ethnicity, gender, and social ecology. Br J Psychiatry 174(1):31–38. https://doi.org/10.1192/bjp.174.1.31
Sharma N, Chakrabarti S, Grover S. Gender differences in caregiving among family-caregivers of people with mental illnesses. World J Psychiatry. 2016 6(1):7. Accessed at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4804270/ Accessed date: October, 2022.
Li J, Lambert CE, Lambert VA (2007) Predictors of family caregivers’ burden and quality of life when providing care for a family member with schizophrenia in the People’s Republic of China. Nurs Health Sci 9(3):192–198. https://doi.org/10.1111/j.1442-2018.2007.00327.x
Acknowledgements
We express our sincere appreciation for the support and contributions of the management and staff of Edward Francis Small Teaching Hospital.
Author information
Authors and Affiliations
Contributions
MJM conceived the research idea, designed and collected the data. MJM and HTB analyzed the data. HTB reviewed the data. MJM conducted the literature search. MJM wrote the first draft of the manuscript. All authors reviewed, revised, and approved the final manuscript.
Corresponding author
Ethics declarations
Funding
The authors declare that there was no source of funding.
Availability of data and materials
The data used to support the findings of this study are available from the corresponding author upon request.
Conflict of interest
The authors declare that they have no competing interests. All the authors declare that the submitted work has not been published before (neither in English nor in any other language) and that the work is not under consideration for publication elsewhere.
Ethical approval and consent to participate
The research was approved by the Gambia Government/MRC Joint Ethics Committee. All the study participants signed consent forms and were therefore included in accordance with the ethical standards of the 1964 Declaration of Helsinki and its later amendments.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Marega, J., Bah, H.T. Burdening caregivers of patients with schizophrenia at Edward Francis Small Teaching Hospital, The Gambia. Soc Psychiatry Psychiatr Epidemiol (2024). https://doi.org/10.1007/s00127-024-02634-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00127-024-02634-0