Abstract
Background
In Italy, a growing number of people with severe mental illness (SMI) require care in residential facilities (RFs), a key component of the care pathway. However, despite their development, studies about resident samples have been very few.
Aims
This study, the VALERE-REC Study (eVALuation of outcomE in Residential—use of clinical data with REsearch objeCtives) aims to identify the characteristics that increase the probability to move patients living in RFs to a more independent setting.
Methods
A survey involved 167 patients hosted in 25 RFs of the Verona Mental Health Department. Forty-five patients were residents (27%) in Comunità Terapeutico Riabilitativa Protetta (CTRP); 56 (34%) in Comunità Alloggio (CA), 14 (8%) in Gruppo Appartamento Protetto (GAP), 52 (31%) in Comunità Alloggio Estensiva (CAE). They were assessed for their care pathway after 30-months. The Quality Indicators for Rehabilitative Care—Supported Accommodation (QuIRC-SA) evaluated the quality of 19/25 (76%) RFs. Descriptive analyses were done.
Results
According to the mission stated by the Veneto Region guidelines, RFs hosted patients with different needs and clinical profiles. The mean stay was longer than expected, most patients were unemployed, unmet needs were related to self-management and patient’s social contacts, and recovery-oriented practices were not implemented.
Conclusions
Despite the appropriate admission of patients in different RFs considering their psychopathology, functioning, and needs, the progressive step care pathway did not result effectively pursued. To improve the effectiveness of residential interventions a major task should be to focus on the acquisition of the necessary skills to live independently.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Since the mid-twentieth century, European countries have gone through different processes of deinstitutionalization. This has led to a broad range of services characterized by a strong emphasis on mental health community-based care.
In most European countries, while the number of psychiatric hospital beds has decreased [1] since 1970, there has been an increasing implementation of housing services, so that patients who would have been long-term hospitalized before the de-institutionalization process could live independently or with a variable degree of support. Since 2005, the development of dignituous and respectful of human rights and fundamental freedoms took place in mental health community services, as recommended in the Declaration on Mental Health for Europe [2], the European Commission’s Green Paper [3], the United Nations Convention on the Rights of Persons with Disabilities (CRPD) [4] and has been considered a priority across Europe [5].
Literature reports that moving patients from psychiatric institutions to mental health supported accommodation services, also called in Italy ‘residential facilities’ (RFs), brought positive outcomes in wellbeing and psychological, physical health and higher social functioning [6, 7].
Research in the field proved that the group of people who mostly live in RFs has got a social disability and a Severe Mental Illness (SMI) [8]. People with SMI (about the 4% of people with some mental disorders) showed complex needs, low long-term functioning [9], and the need to receive support to learn how to manage daily activities [10] and to be integrated into the community [11,12,13].
In some European countries, RFs, working in a ‘care pathway’ [14, 15], aim at supporting people with SMI in gaining necessary skills to live an independent and autonomous life [16] and achieving personal recovery—living their life as much satisfying as possible. Rehabilitation programs are usually shared between staff and patients to achieve aims consonant with real patients’ needs [17,18,19]. Unfortunately, in other countries, RFs mostly become long-term permanence, perpetuating the so-called process of ‘trans-institutionalization’ [20,21,22].
Despite the clinical relevance of RFs after the European deinstitutionalization, only few studies [23,24,25,26,27,28] have investigated their performance, quality and effectiveness in supporting people with SMI in effectively achieving independent living and personal recovery, avoiding processes of ‘re-institutionalization’ and/or ‘trans-institutionalization’.
The main aim of this study is to identify the characteristics that increase the probability to move patients living in RFs to a more independent setting and to achieve patient skills that favour personal recovery.
[15, 29]. In detail, this study was developed in the catchment area of the Verona Department of Mental Health (DMH).
Residential facilities in Italy and, particularly, in the Veneto Region
Actually, in Italy around 31,000 people live in RFs at a substantial cost to DMH and taxpayers. The Italian mean of places in RFs is equal to 0.6/10,000 inhabitants [30], resulting in higher than in other high-income European countries, probably because most of them still have psychiatric hospitals and less developed mental health community-based care [1]. The mission of these services is to promote the personal recovery of people with SMI, accounting for difficulty and disability, in the effort to achieve independent tenancy and life. Rehabilitative programs are expected to be tailored to individual needs, personalized and periodically updated, and should address not only practical daily care and nursing but also engage patients in meaningful daily activities and societal participation [16, 29].
Overall, in the Veneto Region in 2017, there were more than 200 mental health RFs, with a total of almost 1900 beds, and of 1989 patients with a diagnosis of SMI who received residential treatment for a total amount of 668,674 days, corresponding to a mean of 336 days/year spent in the Veneto RFs.
This study is focused on the subgroup of RFs in the city of Verona, where the percentage of patients receiving residential treatment represents 3.4% of those in charge of the Verona DMH (catchment area of 472,816 inhabitants with 392,119 people aged 18 years or older). Based on 2016 estimates, residential services are responsible for about 33.7% of the DMH costs [31].
Mission and main features of Italian and Venetian RFs are explained in the National Action Plan for Mental Health 2013–15 (PANSM), and ‘the law 1616’ (the ‘Legge 1616’) [32, 33], whose main characteristics are summarized in Table 1.
The main aim of RFs should be moving residents gradually to more independent accommodations as they gain skills and confidence [16].
The optimal care pathway should thus be characterized by moving from high-intermediate intensity of support (Comunità Terapeutico Riabilitativa Protetta, CTRP, with 24 h/7 staff available) to intermediate support (Comunità Alloggio, CA, with 12 h/day staff) and, finally, to residentials receiving minimal support and aimed to increase self-management (Gruppo Appartamento Protetto, GAP, with 4 h/day staff). Comunità Alloggio Estensiva (CAE) is instead designed for residents with chronic, severe, and stable mental illness.
Material and methods
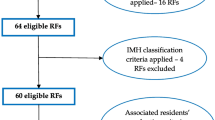
The VALERE-REC Study (eVALuation of outcomE in Residential—use of clinical data with REsearch objeCtives) [16, 34] is a survey aimed to evaluate clinical, social, and rehabilitative outcomes of patients who lived in RFs of the Verona MHD. The extent of patients’ moving on step progressive care pathways was studied having as a baseline six months period from June to December 2014. The moves in the subsequent 30 months were explored (Fig. 1), together with the assessments of the RFs quality.
The graphic shows 158 patients’ (42 CTRP patients, 54 CA patients, 13 GAP patients, and 49 CAE patients) moving from each type of RFs to the same RF and/or other RFs and/or the independent living (IL) after 30 months from the recruitment. Red arrows indicate a moving towards a less independent setting
All these study procedures comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975 (version 2008), and those involving patients were approved by the University Hospital Trust of Verona Research Ethics Committee (reference 34950, 13/11/2018). Written informed consent was obtained from all patients.
Twenty-five out of the 30 RFs in Verona MHD accepted to participate in the study: 5 (20%) CTRP, 6 (24%) CA, 8 (32%) GAP, and 6 (24%) CAE. All patients hosted in one of these RFs in the baseline period were included in the study. Overall, 167 patients were enrolled: 45 (27%) were residents in CTRP, 56 (34%) in CA, and 14 (8%) in GAP, 52 (31%) in CAE.
After accounting for deaths (n = 3) and moves to other facilities (e.g. prison or nursing home) (n = 6), 158 out of 167 (94.6%) patients were assessed at 30-months follow-up using the Verona Mental Health Department database and South-Verona Psychiatric Case Register-PCR [35] (42 of CTRP, 52 of CA, 13 of GAP, 49 of CAE).
Furthermore, the quality of RFs was evaluated for 19/25 (76%) RFs participating in the VALERE-REC study: 4 (21%) CTRP, 6 (32%) CA, 4 (21%) GAP, and 5 (26%) CAE.
Assessments
VALERE-REC data were collected using face-to-face interviews with staff and patients and any other source of reliable information.
Socio-demographic, service use and clinical data were obtained by the PCR. Psychosocial functioning, psychopathology, needs for care, rehabilitative goals as assessed by the staff, service satisfaction and quality of life as assessed by the patients were measured.
The Global Assessment of Functioning Scale (GAF) was used to assess the level of global functioning of the patient, regardless of the nature of the psychiatric disorder [36].
The Personal and Social Performance (PSP) scale, a modified version of the DSM-IV Social and Occupational Functioning Assessment Scale-SOFAS [37] was used.
Psychopathology was assessed with the Italian version of the Brief Psychiatric Rating Scale, expanded version-BPRS [38], which consists of 23 items rated on a seven-point Likert scale (from 1 = no symptom to 7 = extremely severe symptom). Through algorithms from 3 to 6 items of the 24 BPRS items are compacted into 5 main BPRS areas (anxiety-depression, negative symptoms, positive symptoms, mania/excitement, cognition) [39].
Care needs were assessed using the Italian version of the Camberwell Assessment of Need-staff version-CAN-S [40, 41], which comprises 22 items grouped into five conceptual domains: health (physical health, psychotic symptoms, drugs, alcohol, safety to self, safety to others, psychological distress), basic (accommodation, food, daytime activities), social (sexual expression, social networks, intimate relationships), service (information, telephone, transport, benefits) and functioning (basic education, money, childcare, self-care, looking after the home).
The ‘Valutazione Attività e Definizione di Obiettivi’, VADO-AR [42] was used to define and monitor psychiatric goals of rehabilitations in residential contexts.
Subjective quality of life (QoL) was assessed using the Manchester Short Assessment of Quality of Life-MANSA that explores the patient’s perception about its living situation and health [43].
Satisfaction with mental health supported accommodation services was assessed by the patients using—in a context where the privacy of the patients was fully preserved—the Verona Service Satisfaction Scale-Residential Facilities (VSSS-RF), that investigates 6 main areas (Overall satisfaction, Professionals’ skills, and behaviour, Efficacy, Types of intervention, Information, Access) on the 7 areas investigated by other VSSS versions (not having the area related to relatives’ involvement) [44].
This is the first Italian study that assessed the RFs quality using the Italian version of the Quality Indicator for Rehabilitative Care—Supported Accommodation (QuIRC-SA) (translated by Alessandra Martinelli). The QuIRC-SA is the first European standardized tool for quality assessment of RFs. It was developed as part of the English QuEST study (Quality and Effectiveness of Supported Tenancies for people with mental health problems) and adapted, changing some items, from an existing quality assessment tool, the QuIRC [45]. The QuIRC-SA is completed by RFs managers via a webpage that immediately produces a report (https://quirc.eu/quirc-sa/). The questionnaire consists of 143 items, 88 of which contribute to the seven domain scores that range from 0% (the worst quality as possible) to 100% (the best quality as possible). The seven domains explored are living environment (LE) (not for GAP type); therapeutic environment (TE); treatments and interventions (TI); self-management and autonomy (SMA); social interface (SI); human rights (HR); recovery-based practice (RBP) [46]. The remained 55 questionnaire items furnish descriptive data that were not used in our research.
Statistical analysis
The data were analyzed using Stata 15 for Windows.
Frequencies and percentages for categorical variables and mean values (standard deviations) for continuous variables were provided. Comparisons among the groups of patients living in different RFs were performed by using the Chi-square test for categorical variables and the ANOVA with Bonferroni posthoc for continuous variables. All p-values were two-tailed with a significance level of 0.05. No correction for multiple testing was performed due to the explorative nature of the study.
Results
Patients’ characteristics
Differences in sociodemographic, clinical, and psychopathological, and functional characteristics of patients living in different RFs are reported in Table 2. Half of the whole sample shows a diagnosis of schizophrenia, and most patients have an invalidity pension (92.8%). The most three significant differences among patients are found in age, years of contact with mental health services (p = 0.006), and psychopathological symptoms (BPRS, p = 0.005).
Specifically, looking at different RFs, patients living in CTRP show the lowest level of functioning (GAF, p = 0.026) and the highest severity of positive (p = 0.031), negative (p < 0.001), and cognitive symptoms (p = 0.016), while GAP patients are the youngest with the shortest period of contact with mental health services, the lowest number of previous admissions to acute wards (p = 0.031), the best functioning, and the lowest severity of psychopathological symptoms.
Out of 167 patients receiving residential treatment, 74 had medical comorbidity (44.8%). The most frequent comorbidities were diabetes, obesity, hypertension, mental retardation and alcoholism or liver diseases. Some specific patterns of comorbidity were observed: diabetes affected more frequently patients with hypertension and obesity and vice-versa. According to literature, patients with severe psychiatric disorders living in RF had higher medical comorbidities compared to outpatients [34]. In detail, CAE host the oldest patients with the highest number of organic comorbidities (p = 0.015) (Table 2).
Needs for care and staff rehabilitation interventions
Most needs for care in the whole sample are found in the ‘health needs’ domain. Most met needs have been found in the areas of ‘basic needs’ (ratio met/unmet = 5.5), and ‘service needs’ (ratio met/unmet = 4), while the worst ratio is found in the ‘social needs’ area (ratio met/unmet = 1.2) that is indeed the worst ratio of all domains. The ratio between met and unmet needs is unfavourable also in the ‘functioning needs’ area, and this is true in each type of RF, except CA (ratio = 6.8). Overall, the highest number of needs for care is found in CA, where most needs is met (ratio = 4.7), while the ratio between met and unmet needs is more negative in CTRP (ratio = 1.8). In comparison with CA and CAE, CTRP is the setting with the significantly lowest number of met needs and the highest number of unmet needs in each area except for ‘health’ and ‘service’ areas (see Table 3).
Rehabilitative interventions (VADO-AR) are more frequently provided in CTRP (about 60%) and less frequent in GAP (about 40%). Compared to the other RFs, staff interventions in CTRP are mostly related to safety (p < 0.001), social networks (e.g. family life participation p = 0.008), use of transports (p < 0.001), telephone (p = 0.0013), mental health (p = 0.007) and crisis management (p = 0.000); in CA most interventions are focussed on mental health management (85.2%) and daily activities (70.4%); in GAP most interventions are based on management of daily, occupational and employment activities (about 70%); in CAE most interventions are focussed on health care (89.8%) and psychopathology (95.9%).
Quality of life and satisfaction with RF
As shown in Table 4, on average, QoL perceived by patients of the sample is satisfactory (MANSA, mean score 4.9 (SD 0.8) on a 7-point Likert scale from 1 = negative extreme to 7 = positive extreme). The lowest satisfaction of the sample is in ‘sexual life’ (3.3; SD: 1.4), while the highest in ‘personal safety’ (5.7; SD: 1.0).
Specifically, considering the main differences among different RFs, we found that the lowest satisfaction of the sample in ‘friendship’ (n.s.), ‘living situation’ (n.s.) and ‘physical health’ (p = 0.044) are reported in CAE, the most institutionalized setting. While the highest satisfaction for each explored area is found in GAP except for the ‘financial situation’, where patients show the lowest satisfaction of the sample (3.9; SD: 1.7).
No significant differences are detected across the four groups in satisfaction with RFs, with a mean score of 3.8 (SD: 0.5) on the 5-point Likert scale of the VSSS-RF (see Table 4).
The move to a more independent setting for patients living in RFs
Patients’ length of stay in RFs is on average 2–3 times longer than the Regional Government’s established maximum period of the stay [33].
As shown in Supplementary Table 1, most CTRP patients were coming from another RF (63.6%), while 50% of GAP patients lived in independent housing, alone or with others before the current RF (50.0%). After 30 months, only a quarter of patients (39/156, 24.7%) successfully moved to a more independent setting (RF or independent living), while most patients remained in the same RF, and only about 15% moved to a less independent setting.
Around 46% GAP patients after 30 months had moved to independent housing, while most CAE patients remained in the same typology of service (81.6%) (p < 0.001). Furthermore, 47.6% of CTRP patients and 57.4% of CA patients remained in the same RF, while 28.6% CTRP patients and 22.2% CA patients moved to a more independent setting, and around a quarter moved to a less independent setting (23.8% for CTRP; 20.4% for CA). Data show a prevalence of stabilization in CTRP and CA, although the regional recommendations have proposed as optimal a one-two years and three years of stay, respectively.
More details about patients’ moves after 30 months are given in Fig. 1. Overall, the graphic shows that only a minor proportion of patients is moving in the expected step care pathway (CTRP CA GAP independent living).
After 30 months, 7.2% CTRP patients moved to CA and 21.4% moved to independent living, while none moved to GAP. In CA, despite the move of 22.3% patients in the adequate direction (5.5% to GAP and 16.8% to independent living), 20.3% moved to RFs with a lower level of independence (5.5% to CTRP and 14.8% to CAE).
Around 30% of GAP patients after 30 months were still in the same place, while 23% moved to CA, 46.2% moved to independent living, none moved to CTRP or CAE.
In CAE, after 30 months, no patients moved to CTRP/GAP, while 6.2% moved to CA and only 12.2% to independent living.
Unfortunately, except for English data from the QuEST Study [25], no other comparable studies are available in the EU context. A comparison of Italian and English data about moving to a more independent setting after 30 months has shown a slightly more favourable moving in the UK (38% Verona vs 41% the Uk) [16].
Quality of RFs—QuIRC-SA
Information collected using QuIRC-SA from RFs managers shows that on a range of qualitative performance from 0% (minimum) to 100% (maximum), overall, the worst performance is in the ‘recovery-based practice’ area (44.9%), while the best performance is in the ‘human rights’ domain (59.0%) (see Fig. 2).
The graphic shows the quality of the performance of RFs in each QuIRC-SA domain. The performance is reported in means of percentages with SD in the range from 0% (the worst quality as possible) to 100% (the best quality as possible). The seven explored domains are: LIVING environment (LE); therapeutic environment (TE); treatments and interventions (TI); self-management and autonomy (SMA); social interface (SI); human rights (HR); recovery-based practice (RBP). The whole RFs sample is compounded by 19 RFs of which 4 (21%) CTRP, 6 (32%) CA, 4 (21%) GAP, and 5 (26%) CAE
We found that the areas ‘social interface’ and ‘human rights’ show the widest range of performance going from the lowest score in CTRP (44.0% and 48.2%, respectively) to the highest one in GAP (63,9% and 72.7%, respectively).
This kind of data collected by managers may be considered interesting but not completely reliable because of the lack of external control during the questionnaire completion.
Discussion
This is the first Italian study that investigates the effectiveness of RFs for people with SMI in pursuing the outcome of moving to more independent living conditions and to achieve recovery.
Data suggest that, overall, the level of given interventions in different types of RFs is appropriately matched to service patients’ psychopathology, functioning, and basic needs. However, the performance of each type of RF shows that most patients do not move in the right direction of the care pathway but are stuck in the same RF, or, in some cases, cross the care pathway in the opposite direction than expected.
Results show that GAP, despite representing only a small percentage of the whole sample, obtains the best performance. CAE performs adequately considering its mission for SMI. The RFs that should be more capable to generate movement in the care pathway (CTRP and CA) according to our data appear unable to adequately pursue their missions.
Particularly, in CTRPs, that hosted patients with the most severe psychopathology and functioning, about a quarter of patients moved directly to independent living but—contrary to the expected care pathway—few to CA and none to GAP. This might be due to heterogeneity in the given mission of this RF. In fact, CTRPs often admit patients with different needs (e.g. patients with subacute psychopathology after crisis or patients with severe and chronic disorders) thus unexpectedly impacting the linearity of the care pathway.
This study data allows identifying five main obstacles in providing patients living in RFs the necessary skills to live independently and to be re-integrated in the community, as follows.
(1) Length of stay longer than expected. The length of stay in RFs is longer than the Regional Veneto Government’s short-term guidelines [33], considering that, after 30 months, most patients were still residents in the same typology of RF. This phenomenon risks to result in a new ‘re-institutionalization’ process where RFs become ‘houses for life’, thus limiting the patients’ possibility to return to an independent living [20, 22, 47]. The high stability in the system might be explained by:
(a) insufficient implementation of personalized, evidence-based and recovery-oriented practices focused on the improvement of personal and social functioning [48]; (b) people with SMI might need more time than expected to recover adequately to move to a more independent setting [16].
(2) Low attention to the employment rate. On average only 7.3% of patients of the whole sample work, an average that is much lower than the European one that shows an employment rate of about 15% [49]. Positively, 21.4% of patients in GAP are employed, which might indicate that the goal to achieve employment can be pursued in the most independent RF setting. However, the employment rate of the whole sample is extremely low, proving that for most patients an independent life in the community is not financially affordable. This is might due to:
(a) greater barriers to entering into the work market for people with SMI because of stigma and the disability itself [50]; (b) the presence of executive and cognitive impairments, which often affect people with SMI, particularly those living in CAE, in the absence of tailored interventions focused on cognitive rehabilitation [51]; (c) difficulties in structuring adequate relationships between the public services and the B-type social cooperatives, that, in Italy, represent the major employment catalyst for people with SMI [52]; (d) the poor implementation of the Individual Placement Support (IPS) or the Clubhouse models, recognized as the evidence-based and recovery-oriented interventions to place SMI in the competitive market [53, 54].
Thus, mental health services must develop: (i) adequate rehabilitation programs aimed to obtain and keep competitive employment (e.g., IPS/Clubhouse models or B-Type social cooperatives); (ii) favour occupational and pre-employment programs with adequate financial rewards for patients with difficulties to be enrolled in the competitive market.
The involvement of patients in some sort of employment and the provision of support with occupational activities should be relevant indicators of quality in the RFs interventions.
(3) Inadequate response to needs related to self-management. Results show that patients’ needs are similarly high in all RFs, while there is a discrepancy for met needs between the high ratio in ‘basic’ and ‘service’ areas, and the low ratio in ‘functioning’ area. These data might indicate that despite the high level of support on daily activities, the patients’ functioning is not implemented properly. This could be due to:
(a) insufficient implementation of rehabilitative interventions that can be generalized in the real community life; (b) an excess of protection by the staff with the tendency to act in place of the patients in those activities that result difficult for people with SMI. This staff generous attitude paradoxically becomes an obstacle to implement skills needed to live an independent life [55].
The satisfaction of the real needs of patients thanks to more specific, personalized, and innovative rehabilitation interventions might result in the capacity to progressively move patients to the appropriate RF recovery pathway, to reduce ongoing health-related costs, and ameliorate patients’ subjective quality of life [56, 57], that, in our study, results to be mostly good but not excellent.
(4) Social isolation and the patient’s dependency on staff. Results show that social networks are strongly reduced in all RFs, with a higher social network in GAP and a lower in CAE. Possible reasons for this are:
(a) friendship and intimate relationships are difficult to be tackled by the staff [58]; (b) most patients of the sample have a mental health disorder that boosts to social isolation; (c) frequently, most patients of RFs found more attractive day center activities than those in the community, probably because in mental health services they feel less stigmatized, more protected, and welcomed than ‘outside’[59, 60]; (d) whilst there are regular contacts with staff and fellow patients in the services, many patients had only limited contact with friends outside (see Table 3 and 4); (e) social participation interventions for people with mental health problems are limited [61]. Thus, patients might develop real and strong feelings towards staff members to compensate for their social isolation. This might create a safe and therapeutic environment from which patients could acquire the necessary safety to take responsibilities for their lives but also further reduce opportunities to create new social contacts [62, 63]. A negative side effect of strong bonds with staff, is that patients might experience stigma from the staff itself as highlighted in a ‘Perceived Stigma Questionnaire’ developed in Verona, administered to 70 patients that in 40% felt to be treated by staff with paternalism, low trust on their possibility to achieve personal recovery, and the capacity to cover all important adulthood roles (unpublished data available from Department of Neurosciences, Biomedicine and Movement Sciences, University of Verona).
It would be necessary to implement a stronger community network (e.g., mapping all activities of the catchment area) to be able to boost patients at the adequate stage in also using community opportunities, what might fight social isolation and develop a feeling of community belonging.
(5) Scarcity of recovery-oriented practice and risk of transinstitutionalization. Since the Declaration on Mental Health for Europe in 2005, one of the main objective for mental health in Europe has been to provide recovery-oriented practices, as gold-standard for the rehabilitation of people with SMI [18, 48]. However, the worst score at QuIRC-SA in the related-area, and the enlisted four obstacles suggest that most patients in RFs live in a low requesting setting where they take little responsibilities for their lives and face smaller obstacles in daily living than if they lived independently. This might increase the risk for the patients to spend most of their life-changing from one RF to another, thus being exposed to ‘transinstitutionalization’[20].
From these elements, we can infer that the implementation in RFs of care pathways towards recovery and self-awareness represents a current challenge. Staff, stakeholders, and organizations should, therefore, work more towards personal recovery, which allows, through the restitution of individual and personal dignity, to achieve objectives not only oriented to the main patient’s needs of care but also to overcome self-stigma and to increase empowerment.
Strengths and limitations
A limitation of the study is the relatively small sample size and the local area of recruitment (the Verona DMH) that does not allow to use the data for a reliable generalization in the wider Italian context. However, the study design and the systematic approach to obtaining representative data in a specific index period allows making some general considerations that might be comparable to the overall Italian mental health population [30, 64].
Another possible limitation is the naturalistic unbalance found between genders with most males in the RFs. This is probably because women with SMI are still more autonomous and independent than men for socio-cultural reasons and consequently they are less frequently admitted to RFs.
Another limitation is the transversal design, that makes it difficult to infer causality between variables that are associated with each other; however, this is partly overcome with the investigation of patients’ care pathway after 30 months.
Another weak point is that the gathered information is not comprehensive of all the RFs of the area. Some services were contacted but did not respond to the request, introducing a selection bias.
Conclusions
This is the first Italian study on the identification of the characteristics that are more likely to increase recovery and the move to a more independent setting for patients living in RFs. Results show that the services enrolled in the study seem to be able to provide an acceptable environment and meet the fundamental primary needs of most patients, and that, patients are, overall, adequately assigned to RF according to their needs.
However, data show also that there is room to rethink RFs to certain instances. Only a small subgroup of patients moves on progressively in the intended care pathway. There are still major problems in facilitating an increase of autonomy in people with SMI in RFs.
Particularly, five main obstacles have been highlighted in providing the optimal treatment, care, and rehabilitative interventions to supply patients with necessary skills to live independently: (i) length of stay longer than expected; (ii) low attention to the employment rate; (iii) inadequate response to needs related to self-management; (iv) social isolation, patients’ dependency on staff; (v) scarcity of recovery-oriented practice and risk of transinstitutionalization.
Luckily, the understanding of these challenges led to the development of a new Regional Document [65] that configures, as a standard public provision, apartments with a floating outreach organization [25]. This new type of RF, thought as places with minimum staff support and strong involvement in the community living, might develop those specific rehabilitation interventions to support patients to gain those necessary skills to live independently.
Future evaluation of the care provided in RFs and the new floating outreach model must be carried on to better understand which quality standards should be implemented to ensure appropriate and personalized interventions according to patients’ needs to adequately recover.
References
WHO (2018) Monitoring mental health systems and services in the WHO European Region: Mental Health Atlas, 2017. Regional Office for Europe of the World Health Organization, Geneva
Who Europe (2005) WHO European ministerial conference on mental health: facing the challenges, building solutions. Helsinki, Finland, 14 January 2005. http://www.euro.who.int/document/mnh/edoc06.pdf. Accessed 3 Mar 2018
European Commission (2005) Green paper: improving the mental health of the population: towards a strategy on mental health for the European Union. Belgium, Brussels
UN General Assembly (2007) Convention on the rights of persons with disabilities (CRPD): resolution/adopted by the General Assembly, 24 January 2007, A/RES/61/106, available at: https://www.refworld.org/docid/45f973632.html. Accessed 9 Nov 2020
de Almeida C, Killaspy JMH (2011) Long-term mental health care for people with severe mental disorders. Report for the European Commission, Luxembourg
Leff J, Trieman N (2000) Long-stay patients discharged from psychiatric hospitals. Social and clinical outcomes after five years in the community. The TAPS Project 46. Br J Psychiatry 176:217–223
McNamara M, Eichholz PE, Vitale A, Jourdan D (2012) Experiences of clients who have made the transition from the psychiatric hospital to community service provision: a phenomenological approach. Int J Ment Heal Promot 14(1):44–56
Sheridan Rains L, Zenina T, Dias MC, Jones R, Jeffreys S, Branthonne-Foster S et al (2019) Variations in patterns of involuntary hospitalisation and in legal frameworks: an international comparative study. Lancet Psychiatry [Internet] 6(5):403–417. https://doi.org/10.1016/S2215-0366(19)30090-2
Parabiaghi A, Bonetto C, Ruggeri M, Lasalvia A, Leese M (2006) Severe and persistent mental illness: a useful definition for prioritizing community-based mental health service interventions. Soc Psychiatry Psychiatr Epidemiol 41(6):457–463
Holloway F (2005) The forgotten need for rehabilitation in contemporary mental health services. A position statement from the executive committee of the faculty of rehabilitation and social psychiatry. Royal College of Psychiatrists, London
McPherson P, Krotofil J, Killaspy H (2017) Specialist mental health supported accommodation services: A systematic review of mental health and psychosocial outcomes. Manuscr Submitt Publ 18(1):1–15. Available from: http://www.ncbi.nlm.nih.gov/pubmed/29764420. Accessed 17 May 2018
De Girolamo G, Picardi A, Micciolo R, Falloon I, Fioritti A, Morosini P (2002) Residential care in Italy: National survey of non-hospital facilities. Br J Psychiatry 181:220–225
Boardman J, Currie A, Killaspy H et al (2010) Social inclusion and mental health. RC Psychiatry 2010:359
Killaspy H (2016) Supported accommodation for people with mental health problems. World Psychiatry [Internet] 15(1):74–75. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26833612. Accessed 03 Mar 2016
Barbato A, Civenti G, D’Avanzo B (2017) Community residential facilities in mental health services: a ten-year comparison in Lombardy. Health Policy (New York) 121(6):623–628
Martinelli A, Iozzino L, Ruggeri M, Marston L, Killaspy H (2019) Mental health supported accommodation services in England and in Italy: a comparison. Soc Psychiatry Psychiatr Epidemiol 54(11):1419–1427. https://doi.org/10.1007/s00127-019-01723-9
Department of Health (2009) Towards a shared vision for mental health. Consultation. New Horizons, London
Martinelli A, Ruggeri M (2020) The impact on psychiatric rehabilitation of recovery oriented-practices. J Psychopathol 26:189–195
Wolfson P, Holloway F, Killaspy H (2009) Enabling recovery for people with complex mental health needs. A template for rehabilitation services [Internet]. FR/RS/1 F report, editor. Vol. FR/RS/1, Faculty of Rehabilitation and Social Psychiatry Working Group Report. Royal College of Psychiatrists. Available at: http://www.rcpsych.ac.uk/college/faculties/rehabilitationandsocialpsyc/resourcecentre.aspx (retrieved 11 October 2010). England, Wales, Scotland: Royal College of Psychiatrists, Faculty of Rehabilitation and Social Psychiatry 1–46 p. Available from: Enabling recovery for people with complex mental h.pdf
Chow WS, Priebe S (2013) Understanding psychiatric institutionalization: a conceptual review. BMC Psychiatry [Internet] 13(1):1
Priebe S, Frottier P, Gaddini A et al (2008) Mental health care institutions in nine European countries, 2002 to 2006. Psychiatr Serv 59(5):570–573
Taylor Salisbury T, Killaspy H, King M (2016) An international comparison of the deinstitutionalisation of mental health care: development and findings of the mental health services deinstitutionalisation measure (MENDit). BMC Psychiatry 16(1):1–10. https://doi.org/10.1186/s12888-016-0762-4
Picardi A, Lega I, Candini V, Dagani J, Iozzino L, de Girolamo G (2014) Monitoring and evaluating the Italian mental health system: the “Progetto Residenze” study and beyond. J Nerv Ment Dis 202(6):451–459
Neri G, Guzzetta F, Pazzi L, Bignami R, Picardi A, De Girolamo G (2011) How does the residential care system change? A longitudinal survey in a large region of Italy. Community Ment Health J 47(2):201–208
Killaspy H, Priebe S, Bremner S, McCrone P, Dowling S, Harrison I et al (2016) Quality of life, autonomy, satisfaction, and costs associated with mental health supported accommodation services in England: a national survey. The Lancet Psychiatry 3(12):1129–1137
Killaspy H, White S, Taylor TL, King M (2012) Psychometric properties of the mental health recovery star. Br J Psychiatry 201:65–70
Cardoso G, Papoila A, Tomé G, Killaspy H, King M, Caldas-de-Almeida JM (2016) Living conditions and quality of care in residential units for people with long-term mental illness in Portugal—a cross-sectional study. BMC Psychiatry 16(1):1–10. https://doi.org/10.1186/s12888-016-0743-7
Kalisova L, Pav M, Winkler P, Michalec J, Killaspy H (2018) Quality of care in long-term care departments in mental health facilities across the Czech Republic. Eur J Public Heal 28(5):885–890
Ministero Italiano della Salute (2013) Accordo Conferenza Unificata 17 ottobre 2013. Le Strutture Residenziali Psichiatriche. Ministero della Salute, Italy
Ministero Italiano della Salute (2018) Rapporto salute mentale, Analisi dei dati del Sistema Informativo per la Salute Mentale (SISM), Anno 2017. SISM, editor
Starace F, Mungai F (2017) La salute mentale in Italia Analisi delle strutture e delle attività dei. Dipartimenti di Salute Mentale Quaderni di Epidemiologia Psichiatrica, vol 1. SIEP, Italia
Inter-regional Group on Mental Health (GISM) (2013) Piano di Azioni Nazionale per la Salute Mentale (PANSM) Available from: http://www.agenas.it/images/agenas/oss/assistenza/salutementale/1_Piano_di_azioni_nazionale_salute_mentale.pdf. Accessed 1 Oct 2017
Repubblica Italiana (2008) Deliberazione della giunta regionale n. 1616, Approvazione dei requisiti e degli standard per le unità di offerta nell’ambito della salute mentale (L.R. 16 agosto 2002, n. 22 “Autorizzazione e accreditamento delle strutture sanitarie, socio sanitarie e sociali”). In: Bollettino Ufficiale Regione Veneto. Venezia, Italy
Iozzino L, Cristofalo D, Bovo C, Bonetto C, Ruggeri M (2018) Medical comorbidities in patients receiving residential treatment: results from the VALERE (eVALuation of outcomE in REsidential facilities) project. J Psychosom Res 109:110
Amaddeo F (2018) Using large current databases to analyze mental health services. Epidemiol Prev 42(1):98–99
American Psychiatric Association (2000) Diagnostic and statistical manual of mental disorders, fourth edition: DSM-IV-TR. United States of America: American Psychiatric Association, Washington, DC
Pedrini L, Lanfredi M, Ferrari C, Andreose S, Basso P, Beneduce R et al (2018) Development and validation of the health of the nation outcome scales-residential facility (HoNOS-RF). Psychiatr Q 89(2):461–473
Ruggeri M, Koeter M, Schene A, Bonetto C, Vazquez-Barquero JL, Becker T et al (2005) Factor solution of the BPRS-expanded version in schizophrenic outpatients living in five european countries. Schizophr Res 75(1):107–117
Shafer A (2005) Meta-analysis of the brief psychiatric rating scale factor structure. Psychol Assess 17(3):324–335
Phelan M et al (1995) The Camberwell Assessment of Need: the validity and reliability of an instrument to assess the needs of people with severe mental illness. Br J Psychiatry 167(5):589–595
Ruggeri M, Lasalvia A, Nicolaou S, Tansella M (1998) Camberwell assessment of need (CAN) (Italian version). In: Slade M, Loftus L et al (eds) Dipartimento di Medicina e Sanità Pubblica, Sezione di Psichiatria, Ospedale Policlinico. Università di Verona, Verona
Gigantesco A, Vittorielli M, Pioli R, Falloon IRH, Rossi G, Morosini P (2006) The VADO approach in psychiatric rehabilitation. Psychiatr Serv 57(12):1778–1783
Priebe S, Knight S, Huxley P (1999) Application and results of the Manchester short assessment of quality of life (MANSA). Int J Soc Psychiatry 45:7–12
Ruggeri M, Dall’Agnola R, Bisoffi G et al (1996) Factor analysis of the Verona Service Satisfaction Scale-82 and development of reduced versions. Int J Methods Psychiatr Res 6:23–38
Killaspy H, White S, Wright C, Taylor TL, Turton P, Kallert T et al (2012) Quality of longer term mental health facilities in Europe: validation of the quality indicator for rehabilitative care against service users’ views. PLoS ONE 7(6):1–8
Killaspy H, White S, Dowling S, Krotofil J, McPherson P, Sandhu S et al (2016) Adaptation of the quality indicator for rehabilitative care (QuIRC) for use in mental health supported accommodation services (QuIRC-SA). BMC Psychiatry 16(1):1–8. https://doi.org/10.1186/s12888-016-0799-4
Killaspy H, Priebe S, McPherson P, Zenasni Z, Greenberg L, McCrone P et al (2019) Predictors of moving on from mental health supported accommodation in England: national cohort study. Br J Psychiatry 216(6):331–337
Martinelli A, Ruggeri M (2020) An overview of mental health recovery-oriented practices: potentiality, challenges, prejudices, and misunderstandings. J Psychopathol 26:1–8
Viering S, Bärtsch B, Obermann C, Rusch N, Rössler W, Kawohl W (2013) The efectiveness of individual placement and support for people with mental illness new on social benefits: a study protocol. BMC Psychiatry 13:195
Battiloro V, Martini A, Mocostabella L, Nava L (2016) Disabili psichici e inserimento lavorativo: Un percorso di ricerca Documento di Valutazione n. 5. Sen. ASVAPP (Associazione per lo Sviluppo della Valutazione e l’Analisi delle Politiche Pubbliche)
Wykes T, Huddy V, Cellard C, McGurk S, Czobor P (2011) A meta-analysis of cognitive remediation for schizophrenia: methodology and effect sizes. Am J Psychiatr 168:472–485
Borzaga C, Poledrini S, Galera G (2017) Social enterprise in Italy: typology, diffusion and characteristics. SSRN. https://doi.org/10.2139/ssrn.3036384
McKay C, Nugent KL, Johnsen M, Eaton WW, Lidz CW (2018) A systematic review of evidence for the clubhouse model of psychosocial rehabilitation. Adm Policy Ment Heal Ment Heal Serv Res 45(1):28–47
Pelizza L, Lorena M, Elisabetta F, Simona V, Maria A, Franzini C et al (2020) Implementation of individual placement and support in Italy: the Reggio emilia experience. Community Ment Health J 56(6):1128–1138. https://doi.org/10.1007/s10597-020-00603-w
Lasalvia A, Ruggeri M, Mazzi M, Dallgnola R (2000) The perception of needs for care in staff and patients in community-based mental health services. The South Verona outcome project 3. Acta Psychiatr Scand 102:366–375
Valdes-Stauber J, Kilian R (2015) Is the level of institutionalisation found in psychiatric housing services associated with the severity of illness and the functional impairment of the patients? A patient record analysis. BMC Psychiatry 15(1):1
Ruggeri M, Leese M, Slade M, Bonizzato P, Fontecedro L, Tansella M (2004) Demographic, clinical, social and service variables associated with higher needs for care in community psychiatric service patients. The South Verona Outcome Project 8. Soc Psychiatry Psychiatr Epidemiol 39:60–68
Bonavigo T, Sandhu S, Pascolo-Fabrici E, Priebe S (2016) What does dependency on community mental health services mean? A conceptual review with a systematic search. Soc Psychiatry Psychiatr Epidemiol 51(4):561–574
Claassen D, Priebe S (2007) Ethical aspects of assertive outreach. Psychiatry 6(2):45–48
Priebe S (2004) Institutionalization revisited—with and without walls. Acta Psychiat Scand 110(2):81–82
Webber M, Fendt-Newlin M (2017) A review of social participation interventions for people with mental health problems. Soc Psychiatry Psychiatr Epidemiol 52(4):369–380
Burti L (2016) Thirty-five years of psychosocial rehabilitation in Italy. Int J Ment Health 45(1):7–14. https://doi.org/10.1080/00207411.2015.1119374
Nelson G, Laurier W (2010) Housing for people with seriousmental illness: approaches, evidence, and transformative change. J Soc Soc Welf 37:123–146
Regione Veneto (2017) Settore Salute Mentale e Sanità Penitenziaria La residenzialità psichiatrica nel Veneto. Regione Veneto, Veneto
Repubblica Italiana (2018) Deliberazione della Giunta Regionale n. 1673 del 12 novembre 2018 Programmazione del sistema di offerta residenziale extra-ospedaliera per la salute mentale. Italia: Bollettino Ufficiale della Regione del Veneto n. 118, p. 94–106
Acknowledgements
The Authors thank Dr. Marco Colizzi for the contribution given in the revision of the final version.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Martinelli, A., Iozzino, L., Pozzan, T. et al. Performance and effectiveness of step progressive care pathways within mental health supported accommodation services in Italy. Soc Psychiatry Psychiatr Epidemiol 57, 939–952 (2022). https://doi.org/10.1007/s00127-021-02128-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-021-02128-3