Abstract
Objectives
To quantify the strength of association between passive and active forms of screen time and adolescent major depressive episode and anxiety disorders.
Methods
Data from the 2014 Ontario Child Health Study, a representative sample of 2,320 adolescents aged 12–17 years in Ontario (mean age = 14.58, male = 50.7%) were used. Screen time was measured using adolescent self-report on time spent on screen-based activities. Past 6-month occurrence of DSM-IV-TR defined major depressive episode, social phobia, generalized anxiety disorder, and specific phobia which were assessed using the Mini International Neuropsychiatric Interview for Children and Adolescents.
Result
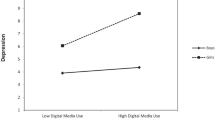
Adolescents reporting 4 or more hours of passive screen time per day, compared to those reporting less than 2 h, were three times more likely to meet the DSM-IV-TR criteria for major depressive episode [OR = 3.28(95% CI = 1.71–6.28)], social phobia [OR = 3.15 (95% CI = 1.57–6.30)] and generalized anxiety disorder [OR = 2.92 (95% CI = 1.64–5.20)]. Passive screen time continued to be significantly associated with increased odds of disorders, after adjusting for age, sex, low income, active screen time use, sleep and physical activity. A small-to-moderate attenuation of the estimated ORs was observed in the fully adjusted model. In contrast, associations between active screen time use and depression and anxiety disorders were smaller in magnitude and failed to reach statistical significance.
Conclusions
Passive screen time use was associated with mood and anxiety disorders, whereas active screen time was not. Further research is needed to better understand the underlying processes contributing to differential risk associated with passive versus active screen time use and adolescent mood and anxiety disorders.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Adolescence is a vulnerable developmental period for the emergence of mental disorders, with half of lifetime mental disorders initially presenting before age 14 [1]. Based on a recent meta-analysis, 13.4% of children and adolescents in high-income countries have a mental disorder, with rates of anxiety and depressive disorders estimated at 6.5% and 2.6%, respectively [2]. Among adolescents in Canada, the prevalence of a major depressive episode (4.8%) and any anxiety disorder (11.0%) is high [3] and has increased over the past 30 years [4], consistent with US evidence [5, 6]. The early emergence of depressive and anxiety disorders and temporal trends suggestive of increasing prevalence, signify a need to identify and mitigate modifiable risk factors for these conditions.
The risk of excessive screen time on mental health represents an emerging public health concern for adolescents [7,8,9]. While current evidence suggests that overall screen time is significantly associated with increased mental health problems [10, 11], it remains unclear whether specific forms of screen time are differentially associated with mental health problems. In addition to the actual amount of time youth spend on screens, many have argued for the importance of considering the types of activities youth are engaged in while on their screens [12,13,14,15,16,17]. Accordingly, in the present study, we distinguished between active versus passive forms of screen time. Active screen time refers to cognitively, socially or physically engaging in screen-based activities that may be reciprocal in nature, such as video gaming, chatting and working on a computer [12]. In contrast, passive screen time refers to passively receiving screen-based information, such as watching TV, videos or movies [12]. To date, most studies examining the association between screen time and adolescent mental health problems have not differentiated between active versus passive forms [10]. Previous studies have either combined both forms of screen time or focused exclusively on one form. When combined, passive and active screen time is associated with anxiety, depression and psychopathological symptoms [18,19,20,21]. The few studies that differentiated between these forms have documented associations between excessive TV watching and low self-esteem [22], depression and anxiety symptoms among adolescents [23, 24]. Similarly, studies have documented a positive association between active screen time and depressed mood, anxiety, low self-esteem, and externalizing behaviours [25, 26]. While informative, these studies focus exclusively on only one form of screen time and fail to account for other types. It is currently unclear whether these different forms of screen time each contribute independently to the prediction of mental health problems when examined concurrently in the same analytic models. This is particularly important given the high co-occurrence of multiple forms of screen use [9, 27]. To our knowledge, there is only one study to date that differentiated between multiple forms of screen time (i.e. social, passive, interactive, educational, or other) and examined their independent associations with developmental outcomes among youth [17]. Passive screen time was associated with poorer physical health, quality of life, socio-emotional outcomes, and school achievement, while other forms of screen time were not. This study, however, did not include a comprehensive approach for assessing and classifying adolescent mental disorders. As such, the extent to which different forms of screen time are independently associated with DSM-IV-TR defined mental disorders among adolescents remains unclear.
With much of the evidence to date on screen time and adolescent well-being arising from correlational studies [15, 28], it is difficult to determine a clear causal association and potential mechanisms of effect. In a recent review paper, Twenge [29] proposed several possible mechanisms through which excessive screen use may be associated with lower psychological well-being among adolescents, including sleep disruption, displacement or disruption of face-to-face social interaction or physical activity, social comparison or cyberbullying. Sleep and physical activity represent well-established correlates of excessive screen time use and adolescent mental health outcomes. Previous studies indicate that excessive screen time is associated with poor sleep among adolescents [24, 30,31,32,33,34,35]. This may be explained by the displacement of sleep time later into the night [34, 36], the excitement produced from the media, and the effects of light exposure at night, especially the highly stimulating blue light waveform emitted by most electronic device screens [32]. There is also strong evidence that physical activity is inversely associated with time spent on screens [24, 37] and symptoms of depression and anxiety [38, 39].
To date, only a limited number of studies have considered sleep and physical activity when examining associations between screen time and adolescent mental health [15]. Barlett, Gentile [40] found in their longitudinal study that total sleep time mediated the positive association between screen time use and inattention and physical aggression in children (mean age = 9.6). This study, however, did not differentiate between active and passive forms of screen time use, nor did it consider the role of physical activity in the association. In contrast, Herman, Hopman [41] found that physical activity and screen time were each independently associated with self-reported mental health and overall health in Canadian adolescents; however, this study did not consider the role of sleep and it too, did not differentiate between passive and active forms of screen time use. To the best of our knowledge, only two studies have examined associations between screen time—an indicator that combined passive and active forms—and mental health problems, physical activity and sleep [42, 43]. Using samples of college students in China, both studies found that higher screen time use and lower levels of physical activity were each independently associated with self-reported mood and anxiety symptoms and their co-occurrence produced synergistic, adverse effects [42, 43]. Both studies were based on a sample of college students and relied on non-clinical measures of mental health problems, limiting their generalizability and clinical utility. In sum, given the state of existing evidence [15, 29], the possibility of bidirectional and reciprocal associations between screen time, adolescent mood and anxiety disorders, sleep and physical activity can not be ruled out [29, 44, 45]. As such, the current study quantified the strength of association between different forms of screen time use, namely passive and active forms, and adolescent mood and anxiety disorders, before and after statistically adjusting for physical activity and sleep.
The present study adds to the current literature by (i) differentiating between active versus passive forms of screen time use and examining their independent contributions to mood and anxiety disorders in a representative sample of adolescents, (ii) using a well-validated, fully structured diagnostic interview to classify DSM-IV-TR major depressive episode, social phobia, generalized anxiety disorder, and specific phobia, administered independently to a primary caregiver and adolescent, (iii) examining well-established correlates of screen time and adolescent mood and anxiety disorders to determine their impact on the associations of interest, and (iv) using a household-based, general-population sample of adolescents and their primary caregiver.
Methods
Participants and procedures
This study uses data from the 2014 Ontario Child Health Study (2014 OCHS), a province-wide, cross-sectional study on child and adolescent mental disorders in Ontario, Canada. A probability sample of 6537 households (50.8% response) with 10,802 children, 4- to 17-year olds, participated in the study. Households were selected based on cluster sampling of residential areas and stratification by residency (urban, rural) and income (areas and households cross-classified by three levels of income including < 20th to > 80th percentiles). Data were collected in home by trained Statistics Canada interviewers from the person most knowledgeable about the child (98.6% identified as the parent of the child and, therefore, hereafter referred to as parent) and adolescents themselves. Data collection occurred from October 2014 to October 2015. Detailed accounts of the survey design, content, training and data collection are available elsewhere [46, 47].
The present study included adolescents aged 12–17 years and their parents, who each independently completed the mini international neuropsychiatric interview for children and adolescents (MINI-KID). Among the 2728 eligible adolescents, 15% (n = 408) were excluded from this analysis due to missing responses. The final sample for analyses includes, 2,320 adolescents (mean age = 14.58, male = 50.7%). No statistically significant differences were observed when comparing those included versus excluded from the analyses in all study variables. The 2014 OCHS was a voluntary survey conducted under the Statistics Act, which provides respondents with guarantees of their privacy, confidentially and informed consent. The study procedures were approved by the Hamilton Integrated Research Ethics Board at McMaster University and Research Ethics Committees at participating school boards. The study has been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Measures
Independent variables
Screen time: Adolescents were asked to report on screen time use. Passive screen time was assessed using the following item: “Over the past seven days, on average how many hours per day did you sit and watch TV, movies or videos, including on YouTube?” Active screen time was assessed using the following item: “Over the past seven days, on average, how many hours per day did you spend outside of school on a computer, laptop, tablet or smart-phone (working, playing games, emailing, chatting, surfing the Internet, etc.)?” Response options for both questions included no use to less than 1 h (0), 1 h to less than 2 h (1), 2 h to less than 3 h (2), 3 h to less than 4 h (3), 4 h to less than 5 h (4), 5 h or more (5). Response options were then collapsed into the following categories: less than 2 h (= 0, reference), 2 to less than 4 h (= 1), and 4 or more hours (= 2). The categorization of response options was informed by the Canadian 24-h movement guideline that recommends adolescents to spend less than 2 h of screen time per day [48] and from an empirical evaluation of the distribution of the data.
Physical activity: Adolescents were provided with a definition of physical activity, “Physical activity is any activity that increases your heart rate and makes you get out of breath some of the time. It can be done in sports, school activities, playing with friends, walking to school or playing active video games such as Wii Sports or Wii Fit. Please include both school and non-school activities.” and then asked the following question: “Over a typical or usual week, on how many days are you physically active for a total of at least 60 min per day?” Responses were combined into the following three categories: 6–7 days (= 0, reference), 4–5 days (= 1), 0–3 days (= 2). The categorization of response options was informed by the Canadian 24-h movement guideline that recommends adolescents be involved in rigorous physical activity for at least an hour, 3 days per week or more [48] and from an empirical evaluation of the distribution of the data.
Sleep: Adolescents were asked about three aspects of sleep over the past 6 months: sleep delay, sleep interruption, and sleep duration. Adolescents reported: (1) how long it takes them to fall asleep [sleep delay: Less than 5 min, 5–10 min, 11–30 min, More than 30 min], (2) how often they usually wake up during the night [sleep interruption: Almost every night (5–7 times/week), Several times a week (1–4 times a week), every now and then (2–3 times a month), Almost never, Never)], and (3) the typical amount of time spent asleep on school nights, excluding any time spent awake in bed (sleep duration). Responses were collapsed into the following categories for each of the 3 indicators of sleep: sleep delay [ten minutes or less (= 0, reference), more than 10 min (= 1)], sleep interruption [never to almost never (= 0, reference), every now and then to several times a week (= 1), almost every night (= 2)], and sleep duration [more than 8 h (= 0, reference), 7 to 8 h (= 1), less than 7 h (= 2)]. The categorization of these indicators of sleep was informed by the Pittsburgh sleep quality index [49] and by the distribution of the variables in our data.
Socio-demographic characteristics. Standard Statistics Canada questions were administered to the PMK about the child’s age (in years), sex (0 = male, 1 = female), and household income below the low-income measure (0 = not low income, 1 = low income) based on 2013 before tax cut-offs [47].
Dependent variable
Past 6-month DSM-IV-TR major depressive episode and anxiety disorders: A modified version of the Mini International Neuropsychiatric Interview for Children and Adolescents (MINI-KID), a fully structured diagnostic interview was administered by trained interviewers to the parent about the child (MINI-KID-P) and separately to adolescents (12–17 years) (MINI-KID) [50, 51]. Training of Statistics Canada interviewers on the administration of the MINI-KID included an in-depth review of an interviewer manual and training videos with example interviews and practice assessments. Disorder classifications derived from the MINI-KID demonstrate adequate test–retest reliability across disorders, informants and samples, and convergent and discriminant validity [50, 51]. DSM-IV-TR anxiety disorders assessed include generalized anxiety disorder, separation anxiety, social phobia and specific phobia. All classifications were made using DSM-IV-TR distress or impairment criteria and were assessed for the past 6 months. The Wald χ2 was used to test for statistically significant differences in the strength of association between screen time use (passive and active) and adolescent- versus parent-reported classifications of mood and anxiety disorders. The results indicated no statistically significant differences between parent and youth informants (see Table 3 in Appendix). Based on these results, disorder classification was based on both parent and youth assessments. If either parent or youth assessments met DSM-IV-TR criteria for the disorder, the youth was classified as having the disorder (i.e., ‘or’ rule at the disorder level).
Statistical analyses: Bi-variate distributions of major depressive episode and anxiety disorders by passive and active screen time, physical activity, sleep, and socio-demographic correlates were examined. Furthermore, a series of binary, logistic regression models were used to determine the strength of associations between different forms of screen time and adolescent MDE and anxiety disorders. Model 1 included age, sex, low income, and active and passive forms of screen time use (referred to as ‘partial adjustment’), while Model 2 also included the addition of indicators of sleep quality and duration and physical activity (referred to as ‘full adjustment’). Adjusted odds ratios (ORs) and 95% confidence intervals (CIs) are reported. Logistic regression analyses were performed using statistical software STATA version 15.0 [52]. Sampling weights were applied to obtain population estimates, and the bootstrap method was used to obtain accurate variance estimation by taking into account the design features of the study and weight adjustments [47].
Results
Table 1 presents the past 6-month prevalence of major depressive episode, social phobia, generalized anxiety disorder, and specific phobia by passive and active forms of screen time use, physical activity, sleep and socio-demographic covariates. Notably, the prevalence of major depressive episode was significantly higher among adolescents who endorsed 4 or more hours per day of active or passive screen time, compared to those who endorsed less than 2 h per day. While the prevalence of major depressive episode was 5.0% among those endorsing less than 2 h of passive screen time per day, it was 14.3% among those endorsing 4 or more hours of passive screen time per day [OR = 3.28 (95%CI = 1.71–6.28). Comparable estimates for active screen time and major depressive episode were 6.4% versus 11.4%, respectively, [OR = 2.00 (95% CI = 1.02–3.91)]. While associations between 4 or more hours of passive screen time use per day and social phobia and generalized anxiety disorder were statistically significant [OR = 3.15 (95% CI = 1.57–6.30) and OR = 2.92 (95% CI 1.64–5.20) respectively], but associations between active screen time use and social phobia and generalized anxiety disorder were not statistically significant.
Table 2 presents partially (Model 1) and fully adjusted (Model 2) associations between different forms of screen time use and adolescent major depressive episode, social phobia, generalized anxiety disorder and specific phobia. Under partial adjustment, adolescents who endorsed passive screen time use for 4 or more hours per day were 3.33 times more likely to meet the criteria for major depressive episode (95%CI = 1.50–7.40), 4.58 times more likely to meet the criteria for social phobia (95%CI = 1.83–11.47) and 3.26 more likely to meet criteria for generalized anxiety disorder (95%CI = 1.65–6.43), compared to adolescents endorsing less than 2 h per day of passive screen time. In contrast, associations between active screen time use and mood and anxiety disorder were smaller in magnitude and did not reach statistical significance after partial adjustment.
The inclusion of sleep and physical activity in the fully adjusted models (Model 2) led to a small-to-moderate attenuation in the strength of association between 4 or more hours of passive screen time per day and adolescent mood and anxiety disorders. However, the odds of major depressive episode and anxiety disorder remained roughly 2.7–3.3 times higher. For example, the odds of major depressive episode associated with 4 or more hours of passive screen time per day went from 3.33 in Model 1 to 2.73 in Model 2, with a reduction of 18%. Comparable estimates for social phobia and generalized anxiety disorder include reductions in the odds ratio from Model 1 to Model 2 in the magnitude of 28% and 14%, respectively. Sleep delay, sleep interruptions and reduced sleep duration were each significantly and independently associated with increased odds of major depressive episode, social phobia, and generalized anxiety disorder among adolescents. Physical activity was no longer significantly associated with major depressive episode and anxiety disorders after adjusting for covariates.
Discussion
This study identified that 4 or more hours of passive screen time use per day, significantly and consistently increased the likelihood of being classified with a major depressive episode, social phobia, and generalized anxiety disorder. These associations persisted over and above statistical adjustments for physical activity and sleep. In contrast, few associations were found between active screen time use and these disorders.
The current results align with past studies documenting a positive association between screen time use and self-reported depression and anxiety symptoms [22, 24, 53, 54]. Physical activity was not associated with major depressive episode and anxiety disorders after adjusting for demographic covariates, screen time and sleep. These findings conflict with past studies that document a negative association between physical activity and adolescent depression and anxiety symptoms [38, 39, 55]. The shared variance between adolescent reports of passive and active screen time use and physical activity may explain our findings. When screen time was removed from our models, 0–3 days of physical activity per week was significantly associated with increased odds of a major depressive episode, social phobia, and generalized anxiety disorder. Similarly, in unadjusted models, adolescents endorsing 0–3 days of physical activity per week were 2–3 times more likely to be classified with major depressive episode, social phobia and generalized anxiety disorder, compared to those adolescents endorsing 6–7 days/week of rigorous, physical activity (Table 1).
Four or more hours per day of passive screen time was associated with a 3–4fold increase in the odds of major depressive episode, social phobia, and generalized anxiety disorder in adolescents, compared to less than 2 h per day. Adjusting for sleep and physical activity led to a small-to-moderate attenuation in odds, although passive screen time continued to be independently associated with disorder. Given the cross-sectional nature of our study design and the existing state of the literature [15, 28], it is impossible to determine the precise role that these variables play (i.e., mediators vs confounders) in the association between passive screen time and adolescent mood and anxiety disorders. The magnitude of the attenuation in the odds ratios, which ranged from 14% for generalized anxiety disorder to 28% for social phobia, however, suggests that they may play an important role in this association [56, 57]. Future longitudinal studies examining the inter-dynamic and reciprocal nature of the associations between sleep, physical activity, screen time, and adolescent mood and anxiety disorders are warranted.
In contrast, associations between active screen time and adolescent mood and anxiety disorders were small in magnitude and failed to reach statistical significance. While our findings on the association between passive screen time and major depressive episode is consistent with previous studies documenting associations between passive screen time and adolescent depressive symptoms [16, 17, 23, 24], associations with active screen time conflict with others that have documented positive associations between active screen time and adolescent depressive and anxiety symptoms [15, 25, 26]. It is important to note, however, that previous studies failed to examine different types of screen time use simultaneously. Therefore, they are not directly comparable to the current findings.
Active screen time (e.g. chatting, video gaming, working, surfing the internet) is interactive and cognitively engaging while the passive screen time (e.g. watching TV, video, YouTube) is more static and solitary. The social displacement model may help explain the differential associations between passive and active forms of screen time and adolescent major depressive episodes and anxiety disorders reported in the current study [58, 59]. The theory posits that the time spent on screens will displace the opportunity to interact with other people. Therefore, engaging in passive screen time may reduce possible opportunities to interact with others. Notably, our finding that 4 or more hours of passive screen time was significantly associated with major depressive episode, social phobia and generalized anxiety disorder while no association was found with specific phobias which provides support for this explanation. In other words, the static and solitary aspect of passive screen time may be linked with internalizing disorders that reflect a lack of social interaction. To this end, our findings may help inform guidelines that consider the differential impact of passive versus active screen time on adolescent mental health to prevent internalizing disorders. However, given the cross-sectional nature of our study, replication and extension of our findings using longitudinal designs are warranted to evaluate the possibility of reverse causation, whereby individuals who are depressed are more likely to engage in passive forms of screen time.
There are several limitations to the current study. The cross-sectional design precludes our ability to understand the temporal ordering between screen time and adolescent major depressive episode and anxiety disorders, and the exact role of physical activity and sleep in these associations. Second, the sole reliance on one self-reported item to assess each of passive and active screen time may reduce measurement sensitivity and contribute to measurement error [15]. For instance, it is possible that adolescents multi-task (e.g. texting while watching TV) which may be more challenging to capture through self-reports of average hours spent on passive and active screen time. More digitalized approaches to measuring screen time should be used in future studies. Lastly, our approach for measuring screen time lacked specificity, with respect to the different types of screen and media content (i.e. access Social Network Sites, video gaming, internet surfing) or failed to differentiate adolescents spending more than 4 h per day on screen.
Despite the aforementioned limitations, our findings add to the current literature by examining the differential association of active versus passive screen time use on adolescent mood and anxiety disorders in a representative sample. Adolescent mental health is highly contingent upon their social lifestyle, which is characterized by the integrated use of devices with screens into their daily lives. Hence, understanding the differential role of active and passive screen time use in adolescent mood and anxiety disorders is critical. Currently, the American Academy of Pediatrics [60] and Canadian guidelines for sedentary activity [61]recommend that adolescents engage in no more than 2 h of screen time per day. However, in Canada, less than 20% of youth meet these guidelines [62, 63], spending 7–8 h daily in front of screens [64]. Evidence arising from the current study can help inform guidelines directed to youth, parents and practitioners around the risks associated with different forms of screen time.
References
Kessler RC et al (2005) Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry 62(6):593–602
Polanczyk GV et al (2015) Annual research review: a meta-analysis of the worldwide prevalence of mental disorders in children and adolescents. J Child Psychol Psychiatry 56(3):345–365
Georgiades K, Duncan L, Wang L, Comeau J, Boyle MH, 2014 Ontario Child Health Study Team (2019) Six-month prevalence of mental disorders and service contacts among children and youth in Ontario: evidence from the 2014 Ontario Child Health Study. Can J Psychiatry 64(4):246–255
Comeau J, Georgiades K, Duncan L, Wang L, Boyle MH, 2014 Ontario Child Health Study Team (2019) Changes in the prevalence of child and youth mental disorders and perceived need for professional help between 1983 and 2014: evidence from the Ontario child health study. Can J Psychiatry 64(4):256–264
Mojtabai R, Olfson M, Han B (2016) National trends in the prevalence and treatment of depression in adolescents and young adults. Pediatrics 138(6):e20161878. https://doi.org/10.1542/peds.2016-1878
Twenge JM, Martin GN, Campbell WK (2018) Decreases in psychological well-being among american adolescents after 2012 and links to screen time during the rise of smartphone technology. Emotion 18(6):765–780
Owen N et al (2010) Sedentary behavior: emerging evidence for a new health risk. Mayo Clin Proc 85(12):1138–1141
Atkin AJ et al (2014) Prevalence and correlates of screen time in youth: an international perspective. Am J Prev Med 47(6):803–807
Sigman A (2012) Time for a view on screen time. Arch Dis Child 97(11):935–942
Hoare E et al (2016) The associations between sedentary behaviour and mental health among adolescents: a systematic review. Int J Behav Nutr Phys Act 13(1):108
Stiglic N, Viner RM (2019) Effects of screentime on the health and well-being of children and adolescents: a systematic review of reviews. BMJ Open 9(1):e023191
Sweetser P et al (2012) Active versus passive screen time for young children. Australas J Early Child 37(4):94–98
Martinez-Gomez D et al (2009) Associations between sedentary behavior and blood pressure in young children. Arch Pediatr Adolesc Med 163(8):724–730
Wang X, Perry AC (2006) Metabolic and physiologic responses to video game play in 7-to 10-year-old boys. Arch Pediatr Adolesc Med 160(4):411–415
Orben A (2020) Teenagers, screens and social media: a narrative review of reviews and key studies. Soc Psychiatry Psychiatr Epidemiol. https://doi.org/10.1007/s00127-019-01825-4
Boers E et al (2019) Association of screen time and depression in adolescence. JAMA Pediatr 173(9):853–859
Sanders T et al (2019) Type of screen time moderates effects on outcomes in 4013 children: evidence from the Longitudinal Study of Australian Children. Int J Behav Nutr Phys Act 16(1):117
Wu X et al (2013) Prevalence and factors of addictive Internet use among adolescents in Wuhan, China: interactions of parental relationship with age and hyperactivity-impulsivity. PLoS ONE 8(4):e61782
Hayward J et al (2016) Lifestyle factors and adolescent depressive symptomatology: associations and effect sizes of diet, physical activity and sedentary behaviour. Aust N Z J Psychiatry 50(11):1064–1073
Houghton S et al (2018) Reciprocal relationships between trajectories of depressive symptoms and screen media use during adolescence. J Youth Adolesc 47(11):2453–2467
Twenge JM, Campbell WK (2018) Associations between screen time and lower psychological well-being among children and adolescents: Evidence from a population-based study. Prev Med Rep 12:271–283
Martins N, Harrison K (2012) Racial and gender differences in the relationship between children’s television use and self-esteem: A longitudinal panel study. Commun Res 39(3):338–357
Domingues-Montanari S (2017) Clinical and psychological effects of excessive screen time on children. J Paediatr Child Health 53(4):333–338
Costigan SA et al (2013) The health indicators associated with screen-based sedentary behavior among adolescent girls: a systematic review. J Adolesc Health 52(4):382–392
Vernon L, Modecki KL, Barber BL (2018) Mobile phones in the bedroom: Trajectories of sleep habits and subsequent adolescent psychosocial development. Child Dev 89(1):66–77
Woods HC, Scott H (2016) # Sleepyteens: social media use in adolescence is associated with poor sleep quality, anxiety, depression and low self-esteem. J Adolesc 51:41–49
Twenge JM, Martin GN, Spitzberg BH (2019) Trends in US Adolescents’ media use, 1976–2016: The rise of digital media, the decline of TV, and the (near) demise of print. Psychol Pop Media Culture 8(4):329
Twenge JM (2020) Why increases in adolescent depression may be linked to the technological environment. Curr Opin Psychol 32:89–94
Twenge JM (2019) More time on technology, less happiness? Associations between digital-media use and psychological well-being. Curr Direct Psychol Sci 28(4):372–379
Hysing M et al (2015) Sleep and use of electronic devices in adolescence: results from a large population-based study. BMJ Open 5(1):e006748
Vallance JK et al (2015) Associations of overall sedentary time and screen time with sleep outcomes. Am J Health Behav 39(1):62–67
Hale L, Guan S (2015) Screen time and sleep among school-aged children and adolescents: a systematic literature review. Sleep Med Rev 21:50–58
Twenge JM, Krizan Z, Hisler G (2017) Decreases in self-reported sleep duration among US adolescents 2009–2015 and association with new media screen time. Sleep Med 39:47–53
Twenge JM (2018) Amount of time online is problematic if it displaces face-to-face social interaction and sleep. Clin Psychol Sci 6(4):456–457
Przybylski AK (2018) Digital screen time and pediatric sleep: evidence from a preregistered cohort study. J Pediatr 205:218–223
Falbe J et al (2015) Sleep duration, restfulness, and screens in the sleep environment. Pediatrics 135(2):e367–e375
Melkevik O et al (2010) Is spending time in screen-based sedentary behaviors associated with less physical activity: a cross national investigation. Int J Behav Nutr Phys Act 7(1):46
Lautenschlager NT et al (2008) Effect of physical activity on cognitive function in older adults at risk for Alzheimer disease: a randomized trial. JAMA 300(9):1027–1037
Sallis JF, Prochaska JJ, Taylor WC (2000) A review of correlates of physical activity of children and adolescents. Med Sci Sports Exerc 32(5):963–975
Barlett ND et al (2012) Sleep as a Mediator of Screen Time Effects on US Children's Health Outcomes. J Child Media 6(1):37–50
Herman KM, Hopman WM, Sabiston CM (2015) Physical activity, screen time and self-rated health and mental health in Canadian adolescents. Prev Med 73:112–116
Feng Q et al (2014) Associations of physical activity, screen time with depression, anxiety and sleep quality among Chinese college freshmen. PLoS ONE 9(6):e100914
Wu X et al (2015) Low physical activity and high screen time can increase the risks of mental health problems and poor sleep quality among Chinese college students. PLoS ONE 10(3):e0119607
Wang J-L et al (2018) The reciprocal relationship between passive social networking site (SNS) usage and users’ subjective well-being. Soc Sci Computer Rev 36(5):511–522
Orben A, Przybylski AK (2019) The association between adolescent well-being and digital technology use. Nat Hum Behav 3(2):173
Statistics Canada (2017) Microdata user guide 2014 Ontario Child Health Study
Boyle MH, Georgiades K, Duncan L, Comeau J, Wang L, 2014 Ontario Child Health Study Team (2019) The 2014 Ontario Child Health Study—methodology. Can J Psychiatry 64(4):237–245
Tremblay MS et al (2016) Canadian 24-hour movement guidelines for children and youth: an integration of physical activity, sedentary behaviour, and sleep. Appl Physiol Nutr Metab 41(6):S311–S327
Buysse DJ et al (1989) The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res 28(2):193–213
Sheehan DV et al (2010) Reliability and validity of the mini international neuropsychiatric interview for children and adolescents (MINI-KID). J Clin Psychiatry 71(3):313–326
Duncan L et al (2017) Psychometric evaluation of the Mini International Neuropsychiatric Interview for Children and Adolescents (MINI-KID). Psychol Assess 30(7):916–928. https://doi.org/10.1037/pas0000541
StataCorp S (2018) Stata Statistical Software: Release 14. College Station, TX: StataCorp LP
Twenge JM et al (2018) Increases in depressive symptoms, suicide-related outcomes, and suicide rates among US adolescents after 2010 and links to increased new media screen time. Clin Psychol Sci 6(1):3–17
Jelenchick LA, Eickhoff JC, Moreno MA (2013) “Facebook depression?” Social networking site use and depression in older adolescents. J Adolesc Health 52(1):128–130
Fox KR (1999) The influence of physical activity on mental well-being. Public Health Nutr 2(3a):411–418
Skelly AC, Dettori JR, Brodt ED (2012) Assessing bias: the importance of considering confounding. Evid Spine-Care J 3(01):9–12
Kleinbaum DG et al (1988) Applied regression analysis and other multivariable methods, vol 601. Duxbury Press Belmont, CA
Kraut R et al (1998) Internet paradox: A social technology that reduces social involvement and psychological well-being? Am Psychol 53(9):1017
Twenge JM, Spitzberg BH, Campbell WK (2019) Less in-person social interaction with peers among US adolescents in the 21st century and links to loneliness. J Soc Pers Relatsh 36(6):1892–1913
Strasburger VC et al (2013) Children, adolescents, and the media. Pediatrics 132(5):958–961
Tremblay MS et al (2016) Canadian 24-hour movement guidelines for children and youth: an integration of physical activity, sedentary behaviour, and sleep. Appl Physiol Nutr Metab 41(6 Suppl 3):S311–S327
Lenhart A et al. (2010) Social Media & Mobile Internet Use among Teens and Young Adults. Millennials. Pew Internet and American life project
Mark AE, Boyce WF, Janssen I (2006) Television viewing, computer use and total screen time in Canadian youth. Paediatr Child Health 11(9):595–599
Leatherdale S, Ahmed R (2011) Screen-based sedentary behaviours among a nationally representative sample of youth: are Canadian kids couch potatoes. Chronic Dis Inj Can 31(4):141–146
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Appendix
Appendix
See Table 3.
Rights and permissions
About this article
Cite this article
Kim, S., Favotto, L., Halladay, J. et al. Differential associations between passive and active forms of screen time and adolescent mood and anxiety disorders. Soc Psychiatry Psychiatr Epidemiol 55, 1469–1478 (2020). https://doi.org/10.1007/s00127-020-01833-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-020-01833-9