Abstract
Purpose
There is evidence to suggest that both early traumatic experiences and perceived discrimination are associated with later onset of psychosis. Less is known about the impact these two factors may have on conversion to psychosis in those who are at clinical high risk (CHR) of developing psychosis. The purpose of this study was to determine if trauma and perceived discrimination were predictors of conversion to psychosis.
Methods
The sample consisted of 764 individuals who were at CHR of developing psychosis and 280 healthy controls. All participants were assessed on past trauma, bullying and perceived discrimination.
Results
Individuals at CHR reported significantly more trauma, bullying and perceived discrimination than healthy controls. Only perceived discrimination was a predictor of later conversion to psychosis.
Conclusions
Given that CHR individuals are reporting increased rates of trauma and perceived discrimination, these should be routinely assessed, with the possibility of offering interventions aimed at ameliorating the impact of past traumas as well as improving self-esteem and coping strategies in an attempt to reduce perceived discrimination.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In the epidemiological literature, there is growing evidence that certain social risk factors may increase the risk of developing psychosis [1–3]. Over the last decade, several lines of evidence suggest a possible association between a history of trauma in childhood and later psychosis or psychotic like experiences [4–6]. A recent meta-analysis [7] indicated that reported exposure to adverse events in childhood is associated with persistence of psychotic experiences, and other studies have suggested that perceived discrimination is a risk factor for psychosis [8, 9]. Additionally, Janssen and colleagues found that perceived discrimination predicted the incidence of delusional ideation in a dose response fashion, even after controlling for various confounds such as depressive symptoms, low self-esteem and neuroticism [10].
Most studies to date investigating trauma and perceived discrimination have focused on established psychotic disorders or non-clinical samples. Although research interest is increasing in the trauma literature among those considered to be at clinical high risk (CHR) of developing psychosis, little is still known about this relationship, and even less is known about perceived discrimination and those at CHR. A recent meta-analysis reported that childhood trauma is highly prevalent among CHR individuals [6]. Furthermore it has been observed that CHR participants experience their first trauma at an earlier age compared to healthy controls, and that both the incidences of trauma, and the age at which trauma occurred were significant predictors of having a CHR status [11]. Sahin et al. [12] found that not only is the frequency of childhood trauma higher among high-risk participants compared to healthy controls, but also that childhood trauma was related to baseline severity of positive symptoms. Others have found that the intensity of perceptual abnormalities are higher among groups that have experienced physical abuse and other trauma compared to those without a history of trauma [13], and that CHR participants who report experiencing childhood trauma have poorer premorbid functioning compared to controls [14]. Yung et al. [15] recently found that childhood maltreatment, as assessed by the Childhood Trauma Questionnaire [16], was a significant predictor of poor functioning in CHR groups, as well as those who eventually transition.
There are only two high-risk studies that we are aware of that have specifically investigated the relationship between trauma and conversion to psychosis [17, 18]. Both of these studies found that the majority of CHR participants experienced a traumatic event, and that sexual trauma was associated with increased risk of transitioning to psychosis. We have previously reported on childhood trauma among CHR individuals from the first half (N = 540) of the North American Prodromal Study (NAPLS-2). We found that CHR participants reported significantly more bullying and trauma compared to healthy controls, and that those who experienced past trauma and bullying were more likely to have increased levels of depression, anxiety, as well as a poorer sense of self [19].
Much less is available in the literature regarding the experience of perceived discrimination among those at risk for psychosis. One recent population level sample found that perceived discrimination at moderate to high levels predicted self-reported psychotic experiences in a linear dose–response fashion [20]. To the best of our knowledge, the only study investigating perceived discrimination among a CHR sample was also from the first half (N = 540) of the NAPLS-2 cohort. In this study CHR participants endorsed significantly more perceived discrimination compared to healthy controls, and this was associated with negative schemas about the self and others [21].
The goal of this study was to determine whether our preliminary baseline findings for the first half of the NAPLS sample held in the final NAPLS-2 sample and additionally to determine whether trauma and perceived discrimination predict later transition to psychosis.
Methods
Participants
The sample consisted of 764 CHR participants (436 male, 328 female) and 280 healthy controls (141 male, 139 female). All participants were recruited as part of the NIMH funded North American Prodrome Longitudinal Study 2 (NAPLS 2) and were drawn from the participating NAPLS 2 sites (Emory University, Harvard University, University of Calgary, University of California Los Angeles, University of California San Diego, University of North Carolina, Yale University, and Zucker Hillside Hospital). The NAPLS-2 project was established to investigate predictors and mechanisms of conversion to psychosis. All CHR participants met the criteria of psychosis-risk syndromes (COPS) using the structured interview for psychosis-risk symptoms (SIPS) [22]. Participants were excluded if they met criteria for any current or lifetime axis I psychotic disorder, prior history of treatment with an antipsychotic, IQ <70 or past or current history of a clinically significant central nervous system disorder. In addition, control participants were also excluded if they had a first degree relative with a current or past psychotic disorder. Further details on ascertainment, inclusion and exclusion criteria have been described in detail elsewhere [23]. Transition to psychosis was determined by meeting the presence of psychotic symptoms (POPS) [24] criteria. Transition criteria is that at least one of the five SOPS positive symptoms reached a psychotic level of intensity (rated 6) for a frequency of ≥1 h per day for 4 days per week during the past month or that symptoms seriously impacted functioning (e.g., severely disorganized or dangerous to self or others). Comprehensive assessments were conducted in order to determine both the COPS and the POPS criteria. Vignettes were developed for each participant in order to obtain a consensus diagnosis both for study entry and for conversion. Raters from all sites reviewed the information on a weekly conference call, and consensus diagnosis decisions were made. Further information has been provided elsewhere [25].
Measures
The structured interview for psychosis-risk syndromes (SIPS) and the scale of psychosis-risk symptoms (SOPS) [24] were used to determine criteria for a prodromal syndrome and to determine severity of attenuated positive symptoms.
Experience of trauma and abuse was assessed using a Childhood Trauma and Abuse scale [26], a semi-structured interview in which the interviewer enquires about trauma and abuse before the age of 16. The participant is asked about any emotional, physical, psychological or sexual abuse they may have experienced. In addition participants were asked if they had experienced either psychological bullying or physical bullying. A total trauma score was created to include the sum of emotional, physical, psychological and sexual abuse, and a total bullying score was created to include both psychological and physical bullying.
Perceived discrimination was assessed using an adapted self-report measure [10]. Participants answered ‘yes’ or ‘no’ to whether or not they had experienced discrimination in their lifetime because of their skin colour; ethnicity; gender; age; appearance; disability; sexual orientation; religion; or other reason. Total perceived discrimination was calculated as the total number of ‘types of discrimination’ that were endorsed.
Procedures
The study was approved by Institutional Review Boards at all eight sites participating in NAPLS. Participants provided informed consent or assent (parental informed consent for minors). Participants were assigned a clinical rater who conducted semi-structured interviews. Raters were experienced research clinicians who demonstrated adequate reliability at routine reliability checks. Gold standard post-training agreement on the determining the prodromal diagnoses was excellent (kappa = 0.90).
Statistical analysis
Chi square tests were used to compare categorical variables, and independent sample t tests were used to compare continuous variables. Mann–Whitney U tests were used for comparison of total traumas and total perceived discrimination. Associations between type of trauma, total trauma, and total perceived discrimination to symptoms and ethnicity were examined using Spearman correlations. As per our previous analysis [21], ethnicity was divided into two sub-categories (white and other). Each of the individual predictors was then examined via a Cox proportional hazard regression model. The Assumption of proportionality of the hazard function over time was checked and the model satisfied the assumption. We first considered a model which included all the predictors that had a p value <0.25 in the univariate analyses, with an aim to drop the least significant variable, then continue by successively refitting the model and applying the same backward elimination rule until all remaining variables were statistically significant. Statistical analyses were conducted using SAS 9.4.
Results
Control participants were slightly older (M 19.73, SD 4.67 for controls and M 18.50, SD 4.23 for CHR) and had more years of education (M 12.68, SD 3.58 for controls and M 12.28, SD 2.82 for CHR) compared to the CHR participants. The majority of the sample was male (55.3 %), unmarried (94.9 % for CHR, 95.0 % for controls), currently enrolled as students (82.5 % for CHR, 81.1 % for controls), and Caucasian (57.3 % for CHR, 54.3 % for controls). Over the 2-year follow-up period, 86 participants transitioned to psychosis. There were no demographic differences between those who transitioned compared to those who did not. There were no demographic differences between those who did and did not complete the trauma or perceived discrimination assessments. One exception was observed among the control group. There was an observed difference for race between those who did and did not complete the perceived discrimination data (X = 5.29, p < 0.05). More specifically, in both the minority racial status group and the Caucasian group, it would be expected that 9.6 % would have the perceived discrimination data missing, when in fact, 14.1 % of the minority group and 5.9 % of the Caucasian group did not.
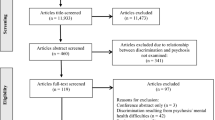
In the NAPLS 2 sample 654 CHR and 224 controls had completed the trauma and bullying questionnaire. 684 CHR and 253 controls completed the perceived discrimination measure. There were various reasons as to why some of the sample did not complete the trauma and perceived discrimination assessments, which included; participant refusal, no show’s for appointments, uncontrollable circumstances, participant drop out, and on rarer occasions, the rater not including the measure. More than half of CHR participants reported experiencing at least one type of bullying (53.3 versus 28.5 % for controls). Nearly half of the CHR participants reported experiencing at least one type of trauma (46.2 versus 11.4 % for controls), and more than half reported experiencing at least one type of discrimination (72.4 versus 57.5 % for controls). Consistent with our past reports on trauma [19] and perceived discrimination [21], CHR participants experienced significantly more overall trauma (z = −6.84, p < 0.0001), bullying (z = −10.58, p < 0.0001) and endorsed significantly more items of discrimination in their lifetime (z = −6.44, p < 0.0001) compared to controls.
Results of the Spearman correlations were that total perceived discrimination was significantly associated with being from an ethnic minority in both the CHR group (r = −0.15, p < 0.0001) as well as in the control group (r = −0.21, p < 0.01). Associations between attenuated psychotic symptoms and trauma and perceived discrimination are presented in Table 1. After applying a Bonferroni correction there were significant relationships between suspiciousness and total bullying and total perceived discrimination. Total perceived discrimination was also positively correlated with disorganized communication. It should be noted however that none of these correlations exceed r = 0.22.
Univariate analyses of potential predictors of conversion are presented in Table 2.
We first considered the combined variable models, which included predictors with univariate hazard ratios that had p values of <0.25. The HRs for the two significant factors in the combined model were re-estimated to yield the final model. In the final model, the individuals at CHR of psychosis who had significantly poorer scores on life time perceived discrimination were more likely to experience conversion to psychosis than people at CHR of psychosis who had good scores on life time perceived discrimination, i.e. for a unit increase in the scores on life time perceived discrimination (i.e. one more life time perceived discrimination question answered by yes), a 52.4 % greater chance of conversion to psychosis (HR 1.101, 95 % CI 1.002–1.209, p = 0.0449). Neither total bullying (HR 1.189, 95 % CI 0.89–1.59, p = 0.24) nor total trauma (HR 1.085, 95 % CI 0.92–1.28, p = 0.34) contributed to the prediction of psychosis in the CHR sample. There were also no significant contributions when each individual item of trauma was assessed; psychological bullying (HR 1.154, 95 % CI 0.71–1.88, p = 0.56), physical bullying (HR 1.544, 95 % CI 0.96–2.49, p = 0.07), emotional neglect (HR 1.504, 95 % CI 0.94–2.39, p = 0.09), physical abuse (HR 1.332, 95 % CI 0.80–2.22, p = 0.27), psychological abuse (HR 1.112, 95 % CI 0.69–1.78, p = 0.66) and sexual abuse (HR 0.974, 95 % CI 0.49–1.90, p = 0.94).
Discussion
This paper examined the impact that trauma and perceived discrimination have on the transition to psychosis among a large sample of individuals at risk for developing psychosis. Relative to controls the CHR group reported having experienced significantly more trauma, bullying, and endorsed more items on perceived discrimination. However, although trauma and bullying were not found to contribute to the prediction of psychosis, those who endorsed more items on the perceived discrimination scale had a greater chance of conversion to psychosis.
Our results are somewhat in contrast to the results of previous studies reporting sexual abuse as a predictor of conversion to psychosis [17, 18]. This may be due to our lower rates of sexual abuse (14.3 % compared to 27 and 28 % in previous studies) or differences in trauma measures in that the other studies used the General Trauma Questionnaire, or the Childhood Trauma Questionnaire. Regardless of this, consistent with other studies, we still found that CHR participants report significantly more levels of overall trauma compared to healthy controls. It is possible however, that a past history of a trauma is a vulnerability factor for being at risk for psychosis and not a vulnerability factor for making the transition to psychosis once part of a high risk group. Additionally, similar to past reports [12], we found that with increased levels of reported trauma there were higher ratings on suspiciousness. However, it has to be noted that none of the correlations exceeded 0.22, which suggests that the relationship was relatively weak.
In our sample perceived discrimination was a significant predictor of later conversion to psychosis. It is well established that the incidence of schizophrenia and other psychotic disorders are higher in ethnic minority groups, and it has been shown that perceived discrimination by ethnic minority groups, at least in studies conducted in Western Europe, may be contributing to this phenomenon [8]. In addition, a study conducted in the USA [27] demonstrating a twofold increase (after controlling for social economic status) in schizophrenia in African–Americans suggests that being African–American is possibly an exposure to status discrimination such as neighborhood segregations, poorer education and fewer opportunities. The authors suggest that a “downstream effect of social racism, and a potential mediator of discrimination, is perceived discrimination”, (p 756). Furthermore, a recent paper [28] demonstrates that in addition to ethnic minority position being associated with increased risk for psychosis, sexual minorities are also at risk for psychosis suggesting that exposure to minority stress in general may represent an important mechanism for the later development of psychosis. This fits with the “social defeat” theory offered by Selten and Cantor-Graae [29] which provides some insight. Social defeat is used to describe the chronic feeling of having an outsider status, or being in a subordinate position. Therefore, it may be that a chronic experience of perceived discrimination is contributing to a feeling of social adversity and outsider status, which is possibly driving this relationship. Furthermore, a separate study [30] has demonstrated that young adults with severe hearing impairments not only experience more feelings of social defeat but also demonstrate greater dopamine release in response to dexamphetamine. This supports the second part of the social defeat theory, which proposes that the chronic experience of social exclusion leads to a sensitization of the dopamine system. Interestingly, we observed that suspiciousness and disorganized communication were positively correlated with total perceived discrimination. These findings may help clarify the direction of this relationship in that perceived discrimination may have preceded the attenuated psychotic symptoms for some individuals but certainly did precede psychosis in our sample (rather than being a consequence of having a psychotic disorder).
Finally, as per our first paper, perceived discrimination was related to ethnicity, and in all participants, perceived discrimination was significantly associated with being from an ethnic minority.
Limitations
There are limitations to this study. Our measures of trauma and PD are brief. We do not have data on how often the trauma occurred, the age of the participant at the time of the trauma or the severity of the trauma. There is also the possibility of recall bias. Similarly, we do not have details on when the perceived discrimination first began. Lastly, given that those with a minority racial status were more likely than those with a Caucasian racial status to have missing perceived discrimination data, it is likely that this could have led to possible bias in the results. However, it should be noted that this observed difference was found among the control group only, and therefore would not have impacted any of the conversion to psychosis results. The strengths are that this is a large well-defined sample with longitudinal data.
Clinical implications
The consistently reported high rates of trauma in this population obviously warrant further attention, and may be an important area of intervention. A recent general population study [31] found that cessation of physical abuse and bullying predicted a cessation of psychotic like experiences. It should however be noted that this study was conducted in the general population and trauma was related to increased “psychotic like experiences”, so it is difficult to know if this would also apply to individuals who are meeting established CHR criteria. Sahin et al. [12] suggest that clinicians be aware of these elevated rates among those at risk and make routine assessment of trauma history in clinical care. Lastly, given our previous findings that perceived discrimination was related to negative schemas [21], it may be that a pervasive negative sense of the self and others is contributing to an increase in perceptions of discrimination. It may therefore be relevant to address these concepts from a cognitive behavioral approach, in hopes to reduce or eliminate these maladaptive beliefs. It is also possible that the reverse is true, that the actual experience of discrimination leads to a pervasive negative sense of self and others. Determining the direction of this association may be important for future research. Finally, it may be that some of these young people are indeed outsiders and a treatment that focuses on skill and relationship development may be more useful than addressing beliefs.
Summary
In summary, CHR participants report experiencing more trauma, bullying, and perceived discrimination compared to healthy controls. Additionally, the more lifetime perceived discrimination endorsed, the greater the chance of conversion to psychosis. While it is difficult to determine the actual experience of discrimination, an attempt to at least identify perceived discrimination may help eliminate feelings of having an outsider status, and ultimately contribute to a reduction or prevention of psychosis.
References
van Os J, Rutten BP, Poulton R (2008) Gene-environment interactions in schizophrenia: review of epidemiological findings and future directions. Schizophr Bull 34(6):1066–1082
Houston JE et al (2008) Childhood sexual abuse, early cannabis use, and psychosis: testing an interaction model based on the National Comorbidity Survey. Schizophr Bull 34(3):580–585
Konings M et al (2012) Replication in two independent population-based samples that childhood maltreatment and cannabis use synergistically impact on psychosis risk. Psychol Med 42(1):149–159
Read J et al (2005) Childhood trauma, psychosis and schizophrenia: a literature review with theoretical and clinical implications. Acta Psychiatr Scand 112(5):330–350
Bendall S et al (2008) Childhood trauma and psychotic disorders: a systematic, critical review of the evidence. Schizophr Bull 34(3):568–579
Kraan T et al (2015) Trauma and recent life events in individuals at ultra high risk for psychosis: review and meta-analysis. Schizophr Res 161(2–3):143–149
Trotta A, Murray RM, Fisher HL (2015) The impact of childhood adversity on the persistence of psychotic symptoms: a systematic review and meta-analysis. Psychol Med 45(12):2481–2498
Veling W et al (2007) Discrimination and the incidence of psychotic disorders among ethnic minorities in The Netherlands. Int J Epidemiol 36(4):761–768
Karlsen S et al (2005) Racism, psychosis and common mental disorder among ethnic minority groups in England. Psychol Med 35(12):1795–1803
Janssen I et al (2003) Discrimination and delusional ideation. Br J Psychiatry 182:71–76
Russo DA et al (2014) Trauma history characteristics associated with mental states at clinical high risk for psychosis. Psychiatry Res 220(1–2):237–244
Sahin S et al (2013) The history of childhood trauma among individuals with ultra high risk for psychosis is as common as among patients with first-episode schizophrenia. Early Interv Psychiatry 7(4):414–420
Velthorst E et al (2013) History of trauma and the association with baseline symptoms in an Ultra-High Risk for psychosis cohort. Psychiatry Res 210(1):75–81
Tikka M et al (2013) Childhood trauma and premorbid adjustment among individuals at clinical high risk for psychosis and normal control subjects. Early Interv Psychiatry 7(1):51–57
Yung AR et al (2015) Childhood maltreatment and transition to psychotic disorder independently predict long-term functioning in young people at ultra-high risk for psychosis. Psychol Med:1–13
Bernstein DP et al (2003) Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse Negl 27(2):169–190
Bechdolf A et al (2010) Experience of trauma and conversion to psychosis in an ultra-high-risk (prodromal) group. Acta Psychiatr Scand 121(5):377–384
Thompson AD et al (2014) Sexual trauma increases the risk of developing psychosis in an ultra high-risk “prodromal” population. Schizophr Bull 40(3):697–706
Addington J et al (2013) Early traumatic experiences in those at clinical high risk for psychosis. Early Interv Psychiatry 7(3):300–305
Oh H et al (2014) Perceived discrimination and psychotic experiences across multiple ethnic groups in the US. Schizophr Res 157(1–3):259–265
Saleem MM et al (2014) Perceived discrimination in those at clinical high risk for psychosis. Early Interv Psychiatry 8(1):77–81
Miller TJ et al (2003) Prodromal assessment with the structured interview for prodromal syndromes and the scale of prodromal symptoms: predictive validity, interrater reliability, and training to reliability. Schizophr Bull 29(4):703–715
Addington J et al (2012) North American Prodrome Longitudinal Study (NAPLS 2): overview and recruitment. Schizophr Res 142(1–3):77–82
McGlashan TH, Walsh BC, Woods SW (2010) The psychosis risk syndrome: handbook for diagnosis and follow-up. Oxford University Press, New York
Addington J, Liu L, Buchy L, Cadenhead KS, Cannon TD, Cornblatt BA, Perkins DO, Seidman LJ, Tsuang MT, Walker EF, Woods SD, Bearden CE, Mathalon DH, McGlashan TH (2015) North American Prodrome Longitudinal Study (NAPLS2): the prodromal symptoms. J Nerv Ment Dis 203(5):328–335
Janssen I et al (2004) Childhood abuse as a risk factor for psychotic experiences. Acta Psychiatr Scand 109(1):38–45
Bresnahan M, Begg MD, Brown A, Schaefer C, Sohler N, Insel B, Vella L, Susser E (2007) Race and risk of schizophrenia in a US birth cohort: another example of health disparity? Int J Epidemiol 36:751–758
Gevonden MJ, Selten JP, Myin-Germeys I, de Graaf R, ten Have M, van Dorsselaer S, van Os J, Veling W (2014) Sexual minority status and psychotic symptoms: findings from the Netherlands Mental Health Survey and Incidence Studies (NEMESIS). Psychol Med 44:421–433
Selten JP, Cantor-Graae E (2007) Hypothesis: social defeat is a risk factor for schizophrenia? Br J Psychiatry Suppl 51:s9–s12
Gevonden M, Booij J, van den Brink W, Heijtel D, van Os J, Selten J-P (2014) Increased release of dopamine in the striata of young adults with hearing impairment and its relevance for the social defeat hypothesis of schizophrenia. JAMA Psychiatry 71(12):1364–1372
Kelleher I et al (2013) Childhood trauma and psychosis in a prospective cohort study: cause, effect, and directionality. Am J Psychiatry 170(7):734–741
Acknowledgments
The authors thank the NAPLS group: T Raedler, L McGregor, D Marulanda, L Legere, L Marshall, E Falukozi, E Fitton, K Smith, (University of Calgary). T Alderman, K Shafer, I Domingues, A Hurria, H Mirzakhanian (UCSD). B Walsh, J Saksa, N Santamauro, A Carlson, J Kenney, B Roman (Yale University). K Woodberry, AJ Giuliano, W Stone, JM Rodenhiser, L Tucker, R Serur, G Min, R Szent-Imrey (Beth Israel Deaconess Medical Center/Harvard). C Bearden, P Bachman, J Zinberg, S DeSilva, A Andaya, S Uguryan (UCLA). J Brasfield, H Trotman, (Emory University). A Pelletier, K Lansing, H Mates, J Nieri, B Landaas, K Graham, E Rothman, J Hurta, Y Sierra (University of North Carolina). A Auther, R Carrion, M McLaughlin, R Olsen (Zucker Hillside Hospital).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding source
This study was supported by the National Institute of Mental Health (Grant U01MH081984 to Dr Addington; Grants U01 MH081928; P50 MH080272; Commonwealth of Massachusetts SCDMH82101008006 to Dr Seidman; Grants R01 MH60720, U01 MH082022 and K24 MH76191 to Dr Cadenhead; Grant U01MH081902 to Dr Cannon; Grant U01MH082004-01A1 to Dr Perkins; Grant U01MH081988 to Dr Walker; Grant U01MH082022 to Dr Woods; and UO1 MH081857-05 Grant to Dr Cornblatt. The NIMH had no further role in study design; in the collection, analysis and interpretation of data; in the writing of the report; and in the decision to submit the paper for publication.
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Rights and permissions
About this article
Cite this article
Stowkowy, J., Liu, L., Cadenhead, K.S. et al. Early traumatic experiences, perceived discrimination and conversion to psychosis in those at clinical high risk for psychosis. Soc Psychiatry Psychiatr Epidemiol 51, 497–503 (2016). https://doi.org/10.1007/s00127-016-1182-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-016-1182-y