Abstract
Purpose
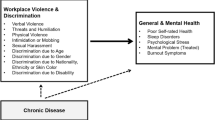
Implementation of primary care has long been a priority in low- and middle-income countries. Violence at work may hamper progress in this field. Hence, we examined the associations between violence at work and depressive symptoms/major depression in primary care teams (physicians, nurses, nursing assistants, and community health workers).
Methods
A cross-sectional study was undertaken in the city of Sao Paulo, Brazil. We assessed a random sample of Family Health Program teams. We investigated depressive symptoms and major depression using the nine-item Patient Health Questionnaire (PHQ-9), and exposure to violence at work in the previous 12 months using a standardized questionnaire. Associations between exposure to violence and depressive symptoms/major depression were analyzed using multinomial logistic regression.
Results
Of 3141 eligible workers, 2940 (93 %) completed the interview. Of these, 36.3 % (95 % CI 34.6–38.1) presented intermediate depressive symptoms, and 16 % (95 % CI 14.6–17.2), probable major depression. The frequencies of exposure to the different types of violence at work were: insults (44.9 %), threats (24.8 %), physical aggression (2.3 %), and witnessing violence (29.5 %). These exposures were strongly and progressively associated with depressive symptoms (adjusted odds ratio 1.67 for exposure to one type of violence; and 5.10 for all four types), and probable major depression (adjusted odds ratio 1.84 for one type; and 14.34 for all four types).
Conclusion
Primary care workers presenting depressive symptoms and those who have experienced violence at work should be assisted. Policy makers should prioritize strategies to prevent these problems, since they can threaten primary care sustainability.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Primary care has been expanding in low- and middle-income countries (LMICs) since the 1970s [1]. In many of these countries, primary care models focusing on strengthening the link between health care providers and the population have played a key role in reducing morbidity and mortality [1–4]. However, violence against health care workers may hamper progress in this field.
High rates of violence against health care workers have been described in emergency rooms and psychiatric settings, particularly of high-income countries [5–7]. Several consequences of this exposure to violence at work have been highlighted in the scientific literature, such as malpractice, low quality of care, depression, post-traumatic disorder, absenteeism, and high turnover [8, 9]. Violence against health care workers in primary care settings has been under-researched. The few existing studies assessed violence against general practitioners in high-income countries, such as Australia and England [10, 11].
Since primary care workers act directly within communities, they may be more exposed to violence at work than health care professionals working exclusively in health care centers. This may be especially problematic in large urban areas of LMICs. Rapid urbanization associated with high rates of urban violence may lead to primary care workers being exposed to even greater levels of violence than those described in high-income countries.
We report here on a study of primary care teams in Sao Paulo, Brazil. We assess the prevalence of exposure to different types of violence at work (insults, threats, physical aggression, and witnessing violence), and the prevalence and severity of depressive symptoms among primary care workers. We also estimate the association between exposure to violence at work and presence of depressive symptoms and probable major depression. Brazil is a particularly valuable site for such research because it has large urban areas and high rates of violence, and it has implemented an enormous primary care program over the past 20 years. The Family Health Program (FHP) currently comprises over 320,000 workers, and covers more than 118 million people across the country, and is still expanding [12]. A similar picture can be found in other LMICs, such as South Africa [3]. In the city of Sao Paulo, which has 11.3 million inhabitants and is the largest urban area in South America, FHP teams are based in 270 primary care centers, and cover 45 % of the population [13].
Method
Study design and participants
The PANDORA-SP (Panorama of Primary Health Care Workers in São Paulo, Brazil: Depression, Organizational Justice, Violence at Work, and Burnout Assessments) was a cross-sectional study undertaken in the city of São Paulo, from October 2011 to November 2012 that evaluated FHP workers: physicians, nurses, nursing assistants, and community health workers (CHW). Primary care centers are managed by 10 private institutions, which have partnerships with City Hall. Each primary care center has from 1 to 12 FHP teams, and each private institution coordinates from 20 to 232 FHP teams.
From the list of all primary care centers with FHP in São Paulo, we randomly selected 66 primary health centers, stratifying by private institutions, number of FHP teams per institution, and number of FHP teams per primary care center. All workers in FHP teams of the primary care centers selected, who had been employed for at least 3 months, were eligible to participate. In São Paulo, FHP job contracts state that the first 3 months of employment are a review period. Therefore, we decided to survey only those workers who had been employed for more than 3 months, to avoid biased responses from individuals concerned about retaining their jobs at the end of their review period.
Both the Medical School of the University of São Paulo (FMUSP) Ethics Committee and the IRB of the Municipal Health Department of the city of São Paulo approved this research. Privacy and confidentiality were guaranteed for participants, and all signed an informed consent before participation.
Measures
Depressive symptoms
Depressive symptoms were assessed using the Brazilian version of the nine-item Patient Health Questionnaire (PHQ-9) [14], which is the depression module of the Primary Care Evaluation of Mental Disorders (PRIME-MD), and is based on the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) criteria for major depression. The Brazilian validation of the PHQ-9 in a general population sample demonstrated sensitivity = 77.5 % (95 % confidence interval = 61.5, 89.2); specificity = 86.7 % (95 % confidence interval = 83.0, 89.9); positive predictive value = 57.8 % (95 % confidence interval = 53.2, 62.4); negative predictive value = 94.3 % (95 % confidence interval = 92.1, 96.4). Participants are required to answer whether, within the previous 2 weeks, they had experienced symptoms that tend to be associated with depression. The possible answers and respective scores are ‘not at all’ (0), ‘less that 1 week’ (1), ‘1 week or more’ (2), and ‘almost every day’ (3). On the basis of PHQ-9 scores, we classified participants into three categories: ‘no depressive symptoms’, ‘depressive symptoms’, or ‘probable major depression’. Participants were classified as having ‘depressive symptoms’ when they reported two or more of the nine depressive symptoms, with only one of the symptoms being depressed mood or anhedonia, for at least 1 week or more of the 15 days prior to interview. Participants were classified as having ‘probable major depression’ when they reported five or more of the nine depressive symptoms, with at least one of the symptoms being depressed mood or anhedonia, for at least 1 week or more of the 15 days prior to interview (scores 2 or 3), with the exception of symptom nine (“thoughts that you would be better off dead or of hurting yourself in some way”) for which any occurrence was counted (“less than 1 week”, “1 week or more” and “almost every day”).
Exposure to violence
Primary care workers regularly perform activities outside health centers, such as home visits, and work directly within the communities. We investigated experiences of violence perpetrated by someone enrolled in the FHP that occurred both in and outside the primary care center. We named this exposure community violence at work, which interweaves two definitions employed in WHO reports: interpersonal community violence, which is ‘violence between individuals who are unrelated, and who may not know each other’ [15], and workplace violence, defined as ‘incidents where staff are abused, threatened or assaulted in circumstances related to their work’ [9]. We studied two types of exposure: direct (situations in which workers are the target of insults, threats, and physical aggressions, by someone from the enrolled population) and indirect (situations in which the worker witnesses violence). To evaluate the direct type, we adapted the questionnaire of the WHO multi-country study on women’s health and domestic violence (Brazilian version) [16], that investigated violence against women perpetrated by an intimate partner. We maintained the underlying principles of the WHO questionnaire: episodes of violence in the previous 12 months; differentiation of acts of violence, such as whether it was an insult, threat, or physical aggression; and the frequency of exposure (‘once’, ‘a few times’, or ‘several times’). We included the following question to determine whether the episode occurred during work, and whether it was perpetrated by someone from the enrolled population: ‘Was it perpetrated by someone from the enrolled FHP population, and while you were working for the FHP’? Questions about indirect exposure to violence at work included witnessing physical assaults, fights using any type of weapon, robberies, someone being shot or murdered, and shootings.
Procedures
To facilitate data collection, an electronic questionnaire was created using the Open Data Kit (ODK) [17]. A pilot study was conducted (n = 54) in a primary care center linked to the FMUSP, to test the procedures and identify unclear questions.
After initial contact with each of the ten institutions and the managers of the 66 primary care centers, trained field researchers scheduled face-to-face meetings with each of the 351 primary care teams. As a result, a total of 3141 workers (community health workers, nursing assistants, nurses and physicians) were invited to participate in our study. The aims of the meetings were to explain the study and its importance, to guarantee privacy, to answer questions, and to schedule the interviews. If primary care workers were not able to attend at the arranged time, they were given the opportunity to reschedule. In addition, as a strategy to reduce losses related to FHP workers being absent from work or on vacation, the field researchers systematically returned to the primary care centers to ensure these workers were not excluded from the study. The participants did not receive any kind of financial incentive to participate in the study. Privacy was guaranteed for participants through the use of a private room for interviews.
Statistical analysis
All analyses were performed using STATACorp 12.0. Logistic regression was used to estimate odds ratios (OR) and 95 % confidence intervals (95 % CI) for the association of depressive symptoms with community violence at work and characteristics of participants. We performed multinomial logistic regression because it allowed analysis of associations of the main exposure with a non-binary outcome: ‘no depressive symptoms’, ‘depressive symptoms’, and ‘probable major depression’. We analyzed each type of violence (insults, threats, physical aggression, and witnessing), and frequency of exposure in the previous 12 months (‘no exposure’, ‘one or a few’, or ‘several times’). We also assessed the number of types of community violence experienced at work (0–4). Chi-squared tests for linear trend were conducted to verify whether frequency of exposure to violence was associated with depression (Table 3).
Since we had randomly selected primary care centers, and not workers directly, we had to adjust both bivariate and multivariate regressions for clustering. Each primary care center was considered a cluster. The intraclass correlation coefficients were as follows: 0.02 for depression, 0.04 for insults, 0.07 for threats, 0.008 for physical aggression and 0.02 for witnessing violence.
We also controlled for gender, age, self-reported skin color, marital status, schooling, monthly income, and stressful life events (SLEs), as they are well-known correlates of depression in Brazil [18]. An SLE could be serious disease, hospitalization, financial strain, romantic breakup, forced change of residence, or death of a close relative, which had occurred in the previous 12 months.
Results
The number of FHP teams per primary care center ranged from 1 to 12 (mean 6.0; SD 2.1). We assessed 351 primary care teams. Of 3141 eligible workers, 2940 (93 %) completed the interview. The majority of participants were CHW (60.2 %), followed by nursing assistants (22 %), nurses (10.4 %), and physicians (7.4 %). The mean age was 36.7 years (SD = 9.6), and most participants were women (90.5 %). 37 % of the participants reported up to 8 years of schooling (mainly CHW). Ten percent of the participants had experienced 3 or more SLEs in the previous 12 months. Other characteristics of the participants are displayed in Table 1.
Proportions of exposure to community violence at work were as follows: insults (44.9 %), witnessing violence (29.5 %), threats (24.8 %), and physical aggression (2.3 %). Almost 30 % of participants reported exposure to two or more types of community violence at work. CHW were more likely to witness violence during their work than other workers (OR ranged from 0.19 to 0.25 with CHW as reference) (Table 2). Physicians and nurses presented a higher odds ratio [OR] for being threatened than CHW, respectively, OR = 1.70 (95 % confidence interval [CI] = 1.24, 2.34), and OR = 1.37 (95 % CI = 1.05, 1.79).
Based on the PHQ-9, 36.3 % (95 % CI = 34.6, 38.1) of participants presented intermediate depressive symptoms and 16 % (95 % CI = 14.6, 17.2) probable major depression. Both were strongly associated with exposure to community violence at work. Moreover, the more frequent the exposure to violence at work, the higher the odds ratio for intermediate depressive symptoms and of probable major depression. Workers who had experienced insults, threats, or witnessing violence several times were more likely to present intermediate depressive symptoms and probable major depression. Importantly, the odds ratio for presenting intermediate depressive symptoms was 1.67 (95 % CI = 1.36, 2.04) in workers exposed to one type of community violence, and 5.10 (95 % CI = 1.31, 19.76) for those exposed to four types. The odds ratio for probable major depression was 1.84 (95 % CI = 1.32, 2.56) for exposure to one type of community violence, and 14.34 (95 % CI = 3.86, 53.17) for those exposed to all four types (Table 3).
Discussion
To the best of our knowledge, this study in São Paulo, Brazil is the first in an LMIC to assess depressive symptoms/major depression and exposure to community violence at work in an entire team of primary care workers, including community health workers. Further, it is the first study to investigate witnessing violence at work in primary care settings. We found a very high prevalence of depressive symptoms/probable major depression based on the PHQ-9, which is higher than that found among health care workers in high-income countries [8, 19], and substantially higher than the prevalence found in a population-based study in Brazil [20]. High levels of exposure to community violence at work were also reported by participants. CHW were more likely to witness violence, while nurses and physicians presented a higher risk of being threatened.
The number of exposures to community violence at work, and the number of types of violence experienced in the previous year were strongly associated with both depressive symptoms and probable major depression. The odds ratio for depression was significantly and progressively higher for those who had experienced community violence more frequently, and for those who reported exposure to different types of community violence at work. This result is consistent with prior evidence of dose–response relations between the number of traumatic events and the severity of depression [21, 22].
The strengths of our study include the large sample size, very high response rate, and adjustments for several covariates, including SLEs. However, the prevalence of depression may have been higher if we had assessed those workers who were absent from work; and the prevalence of violence could have been under-reported due to reporting or recall bias [23], or stigma and shame [24]. The cross-sectional design did not allow us to verify whether exposure to violence occurred before the onset of depression. The associations between physical aggression and depression were imprecise due to the low proportion of workers who reported this type of violence. We did not investigate domestic violence in a sample mainly composed of women, despite evidence of an association between domestic violence and depression [25, 26]. Finally, the location of the study in Latin America’s largest urban area confers both a major advantage—results are highly relevant to primary care teams in urban areas of LMIC—and a limitation in that results may not be generalizable to non-urban settings.
Direct comparison of our findings with previous ones is not possible because to our knowledge, no previous study in an LMIC has investigated exposure to community violence at work among an entire team of primary care workers, including community health workers. However, workplace violence has been investigated in other health care settings. For instance, the WHO’s ‘Workplace Violence in the Health Sectors’ [9] reported on a study of exposure to workplace violence in seven countries, evaluating mainly workers in hospitals settings, and described the proportions of health care workers who had experienced at least one incident of physical or psychological violence in the previous 12 months. In that study, 46.6 % of the health care workers studied in Rio de Janeiro, one of the largest urban areas in Brazil, reported exposure to violence at work in the previous 12 months, which is far less than what we have found among primary care workers (60.3 %).
Data on witnessing violence among health care workers are scarce. Of our participants, 29.5 % had witnessed violence, whereas home care workers in the US have presented a rate of only 4 % [8]. Given that primary care workers regularly work in the community, they are more likely to witness violence during their work. CHW reported witnessing violence at work more frequently than other primary care workers (40 % versus 11.5 % for physicians, 13.1 % for nurses, and 14.5 % for nursing assistants). This result was expected, since CHW spend more time working in the community than the others.
The proportion of exposure to insults (52.5 %), threats (35.5 %), among physicians were higher than those found among general practitioners in Australia (verbal abuse, 42.1 %; threats, 23.1 %). Regarding physical violence, we found a similar proportion (2.3 % among physicians versus 2.7 % among general practitioners in Australia) [10] (Table 2). Physicians and nurses were more likely to suffer threats than CHW. Nurses and physicians in primary care deal directly with their patients’ complaints about difficulties experienced in the Brazilian National Health System. For instance, lack of medications, lack of access to laboratory tests and other specialties. Patients consider these professionals to be government health system representatives and, therefore, expect them to solve any problems which may arise. However, the patients’ expectations frequently cannot be met, creating potential for conflict. In addition, patients can develop defensive behavior and react aggressively towards doctors and nurses after bad experiences with health professionals, such as experiencing violence committed by health workers [27]. Finally, a possible contributing factor to violence against those health care professionals is that depressed workers can be more prone to react when faced with complaints and/or aggressive behavior from their patients, which can damage nurse–patient and doctor–patient relationships. This situation could possibly lead to a vicious cycle: depressed worker, overreaction to patient complaints/behavior, problematic health care worker–patient relationships, more aggressive behavior from patients or from the enrolled population, more depression among health workers.
Our participants presented higher prevalence of depressive symptoms (36.3 %), and probable major depression (16 %) than health care workers in other countries [8, 28], and substantially higher than in a population-based study in Brazil (major depression: 9.4 %) [20]. Similar to our findings, exposure to violence at work increased the odds ratio for depression among home care workers in the US (OR = 3.7, 5.7) [8]. Depression has direct and indirect repercussions, such as disability, impaired work performance, mal practice, and suicide [29, 30]. Violence towards health care workers has been associated with absenteeism, high turnover, depression and low quality of care offered to the patients [7–9, 31–33]. These repercussions make our findings of great concern. Since primary care workers are considered the ‘gatekeepers’ of health care systems, and should ideally guarantee accessibility, longitudinality, and comprehensive care for populations [34], the consequences of exposure to violence at work and depressive symptoms/major depression in these workers can affect accessibility to health care systems and, also, the quality of care delivered to the populations. Therefore, these problems can endanger the sustainability of primary care and, consequently, of the entire health care system. Additionally, in LMICs, where a health care workforce crisis exists [35, 36], and the lack of health professionals in primary care is of great concern, the consequences of exposure to violence at work and of depression in these workers can be even worse.
Our results have implications for stakeholders, for health care organizations, and for policy makers, especially in LMICs, as they expand primary health care. First, workers presenting depressive symptoms need to be recognized and treated. Second, since organizations and policy makers have been facing the health workforce crisis [35, 36], particularly in LMICs and violence at work is an essential factor that contributes towards this crisis, investments should be made in preventing the occurrence of violence experienced by primary care workers, and in assisting workers who have already suffered violence. Finally, we suggest including ‘witnessing violence at work’ in the definition of workplace violence, to be considered an occupational risk and to have legal implications.
References
Rohde J, Cousens S (2008) 30 years after Alma-Ata: has primary health care worked in countries? Lancet 372(9642):950–961
Rasella D, Harhay MO, Pamponet ML, Aquino R, Barreto ML (2014) Impact of primary health care on mortality from heart and cerebrovascular diseases in Brazil: a nationwide analysis of longitudinal data. BMJ 348:g4014
Mayosi BM, Lawn JE, van Niekerk A, Bradshaw D, Abdool Karim SS, Coovadia HM (2012) Health in South Africa: changes and challenges since 2009. Lancet 380(9858):2029–2043
Pallas SW, Minhas D, Pérez-Escamilla R, Taylor L, Curry L, Bradley EH (2013) Community health workers in low- and middle-income countries: what do we know about scaling up and sustainability? Am J Public Health 103(7):e74–e82
Nelson R (2014) Tackling violence against health-care workers. Lancet 383(9926):1373–1374
Tak SW, Sweeney MH, Alterman T et al (2010) Workplace assaults on nursing assistants in US nursing homes: a multilevel analysis. Am J Public Health 100(10):1938–1945
Gerberich SG, Church TR, McGovern PM et al (2004) An epidemiological study of the magnitude and consequences of work related violence: the Minnesota Nurses’ Study. Occup Environ Med 61:495–503
Geiger-Brown J, Muntaner C, McPhaul K, Lipscomb J, Trinkoff A (2007) Abuse and violence during home care work as predictor of worker depression. Home Health Care Serv Q 26:59–77
Di Martino V (2003) Workplace violence in the health sector: Country case studies. World Health Organization. http://www.who.int/violence_injury_prevention/injury/en/WVsynthesisreport.pdf. Accessed 5 May 2014
Magin PJ, Adams J, Sibbritt DW, Joy E, Ireland MC (2005) Experiences of occupational violence in Australian urban general practice: a cross-sectional study of GPs. Med J Aust 183:352–356
Hobbs FDR (1991) Violence in general practice: a survey of general practitioners’ views. BMJ 302(6772):329–332
Ministério da Saúde. Histórico da cobertura da estratégia saúde da família. Ministério da Saúde. http://dab.saude.gov.br/portaldab/ape_esf.php. Accessed 22 Aug 2014
Secretaria Municipal de Saúde (2012) Estratégia Saúde da Família. Prefeitura de São Paulo. http://www.prefeitura.sp.gov.br/cidade/secretarias/saude/atencao_basica/esf/index.php?p=17783. Accessed 21 Apr 2014
Santos IS, Tavares BF, Munhoz TN et al (2013) Sensitivity and specificity of the Patient Health Questionnaire-9 (PHQ-9) among adults from the general population. Cad Saude Publica 29:1533–1543
Krug EG, Dahlberg LL, Mercy JA, Zwi AB, Lozano R (2002) World report on violence and health. World Health Organization. http://whqlibdoc.who.int/publications/2002/9241545615_eng.pdf?ua=1. Accessed 16 Jun 2014
Schraiber LB, Latorre M do RDO, França I, Segri NJ, D’Oliveira AFPL (2010) Validity of the WHO VAW study instrument for estimating gender-based violence against women. Rev Saude Publica 44:658–666
OpenDataKit Web site (2008). http://opendatakit.org. Accessed 18 Oct 2014
Lopes CS, Faerstein E, Chor D (2003) Stressful life events and common mental disorders: results of the Pro-Saude Study. Cad Saude Publica 19:1713–1720
Goldberg RJ, Steury S (2001) Depression in the workplace: costs and barriers to treatment. Psychiatr Serv 52:1639–1643
Andrade LH, Wang Y-P, Andreoni S et al (2012) Mental disorders in megacities: findings from the Sao Paulo megacity mental health survey. Brazil. PLoS One 7:e31879
Tracy M, Morgenstern H, Zivin K, Aiello AE, Galea S (2014) Traumatic event exposure and depression severity over time: results from a prospective cohort study in an urban area. Soc Psychiatry Psychiatr Epidemiol 49:1769–1782
Suliman S, Mkabile SG, Fincham DS et al (2009) Cumulative effect of multiple trauma on symptoms of posttraumatic stress disorder, anxiety, and depression in adolescents. Compr Psychiatry 50:121–127
Moshiro C, Heuch I, Astrøm AN, Setel P, Kvåle G (2005) Effect of recall on estimation of non-fatal injury rates: a community based study in Tanzania. Inj Prev 11:48–52
Ellsberg M, Caldera T, Herrera A, Winkvist A, Kullgren G (1999) Domestic violence and emotional distress among Nicaraguan women: results from a population-based study. Am Psychol 54:30–36
Campbell JC (2002) Health consequences of intimate partner violence. Lancet 359:1331–1336
Devries K, Watts C, Yoshihama M et al (2011) Violence against women is strongly associated with suicide attempts: evidence from the WHO multi-country study on women’s health and domestic violence against women. Soc Sci Med 73:79–86
D’Oliveira AFP, Diniz SG, Schraiber LB (2002) Violence against women in health-care institutions: an emerging problem. Lancet 359(9318):1681–1685
Chambers R, Campbell I (1996) Anxiety and depression in general practitioners: associations with type of practice, fundholding, gender and other personal characteristics. Fam Pract 13:170–173
Goldberg RJ, Steury S (2001) Depression in the workplace: costs and barriers to treatment. Psychiatr Serv 52:1639–1643
Kõlves K, De Leo D (2013) Suicide in medical doctors and nurses: an analysis of the Queensland Suicide Register. J Nerv Ment Dis 201(11):987–990
Wieclaw J, Agerbo E, Bo Mortensen P, Burr H, Tüchsen F, Bonde JP (2006) Work related violence and threats and the risk of depression and stress disorders. J Epidemiol Community Health 60(9):771–775
Büssing A, Höge T (2004) Aggression and violence against home care workers. J Occup Health Psychol 9:206–219
Marchand A, Durand P, Haines V, Harvey S (2014) The multilevel determinants of workers’ mental health: results from the SALVEO study. Soc Psychiatry Psychiatr Epidemiol 50(3):445–459
Starfield B (1994) Is primary care essential? Lancet 344:1129–1133
World Health Organization (2006) The World Health Report 2006: Working together for health. World Health Organization website http://www.who.int/whr/2006. Accessed 10 May 2014
World Health Organization (2003) Workforce crisis a major obstacle in global tuberculosis control. Bull World Health Organ 81(11):85
Acknowledgments
Our study was funded by the São Paulo Research Foundation (FAPESP—2010/07180-6). The sponsor had no role in study design, data collection and processing, interpretation, or writing of the manuscript. PRM was partially funded by CNPq-Brazil. ATCS was partially funded by the NAPSaMP-USP.
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
da Silva, A.T.C., Peres, M.F.T., Lopes, C.d.S. et al. Violence at work and depressive symptoms in primary health care teams: a cross-sectional study in Brazil. Soc Psychiatry Psychiatr Epidemiol 50, 1347–1355 (2015). https://doi.org/10.1007/s00127-015-1039-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-015-1039-9