Abstract
Purpose
Information on older offenders’ mental health service (MHS) used before and after sentence is sparse. We therefore aimed to determine the 1-year prevalence of MHS use before sentence, and the likelihood and predictors of MHS use in the 5-year post-sentence period by first-time older adult offenders (≥45 years).
Methods
Pre- and post-sentence MHS use by a cohort of 1,853 first-time offenders over 45 years in Western Australia was determined through whole-population linked administrative data. Logistic regression models compared the 1-year pre-sentence MHS contacts between offenders and matched non-offenders. Cox proportional hazards regression models identified the socio-demographic, offending and pre-sentence health service variables that determined post-sentence MHS use.
Results
Older offenders were six times more likely to have used MHSs than non-offenders before sentence. Substance use was the most commonly treated disorder. Non-custodial offenders were twice more likely than prisoners to have been treated for any mental disorder and substance use disorders, and violent offenders were four times more likely to have attempted self-harm than non-violent offenders before being sentenced. The strongest predictors of post-sentence MHS contact were past psychiatric diagnosis in offenders with a pre-sentence MHS contact, and pre-sentence hospitalisation for attempted self-harm or physical illness, or being a male in those without. Discontinuity in MHS use after sentence by over half of the offenders with a prior contact was prominent.
Conclusion
Better detection and treatment of mental disorders in older offenders to ensure continuity of care at all transition points through age-sensitive correctional and community-based MHSs is needed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Growing proportions of older prisoners have been reported over recent decades in most western countries [1] including Australia [2]. While this growth is partly attributed to ageing populations and rising crime rates by older people [1, 3], other reasons include the imposition of longer sentences leading to ageing of violent offenders incarcerated when younger, increased incarceration rates for repeat offenders and retrospective sentencing for homicidal or sexual offences committed earlier in life [3–6]. Those incarcerated first at older ages constitute over half of all ‘old’ prisoners and experience relatively more adjustment problems with imprisonment compared with re-offenders or those who grow old in prison [1, 3].
Research has demonstrated greater physical and psychiatric morbidity in older prisoners compared with younger prisoners and the older general population [4, 7–9]. While young offenders mostly present with acute health conditions requiring short-term management, diseases in older offenders are usually chronic and progressive [4, 6]. Estimates indicate that on average, older offenders have three chronic health conditions and almost 20 % have a comorbid mental illness [10], mostly including dementia, affective psychoses, depression, anxiety and alcohol dependence disorders [4]. Older offenders’ requirements for multi-speciality treatments and long-term care [11] may lead to incarceration costs which may be up to three times that for younger offenders [5, 10]. However, while physical healthcare may mostly be appropriate, psychiatric care could be compromised for this group [12].
Furthermore, we recently identified poor post-sentence health outcomes associated with age and low pre-sentence MHS use, whereby older first-time offenders (≥45 years) without pre-sentence MHS contact had a significantly elevated risk of natural death within 2 years of sentence completion than younger offenders [13]. Therefore, information on pre-sentence MHS use and predictors of post-sentence MHS is vital for informing service provision and improvements for this group of first-time older offenders.
To date, only a few whole-population studies have reported offenders to have a greater likelihood of using MHSs before sentencing compared with the wider non-offending community [14–18]. Only two other studies have identified the predictors of MHS use in ex-offenders [19, 20]: one focussing on adult offenders younger than 45 years [19] and the other on substance abuse service use [20]. However, no study has targeted older offenders although in 2012 people over 45 years constituted 11 % of prison entrants Australia-wide, of whom over two-fifths reported a diagnosed mental illness and almost one-third used psychiatric medicines [21]. Even greater proportions would have served non-custodial sentences [22].
This paper describes MHS use 1 year before the first-ever (index) sentence in an offender cohort aged 45 years and above in Western Australia (WA). We also explore the probability of MHS use within 5 years of sentence completion and identify the socio-demographic, offending and pre-sentence health service use variables that were predictive of post-sentence MHS contact in this group.
Methods
Defining ‘older’ offenders
Offenders are believed to age faster than the general population and exhibit health problems prematurely by about 10 years [3–5] due to a range of behavioural, lifestyle and associated health factors [6], although the evidence is unclear. Further, the poorer health and lower life expectancy of Indigenous Australians (Aborigines and Torres Strait Islanders) compared with non-Indigenous Australians are well-established [23]. Most ‘older’ offender research uses age thresholds between 50 and 65 years [4, 24]. However, the Australian Institute of Criminology recommends a threshold of 50 and 45 years to characterise older non-Indigenous and Indigenous offenders, respectively [2]. For these reasons and to ensure a sufficient number of people for analysis, we used a uniform age threshold of 45 years to define our cohort. A threshold of 50 years (n = 1,053) was insufficient to examine statistical associations reliably. However, including offenders aged 45–49 years (n = 800) nearly doubled the sample (43.2 % of cohort) and increased statistical power considerably, thus enabling more reliable comparisons to be performed.
Study populations
The offender cohort included 1,853 offenders aged 45 years and above who commenced their index (first-ever) sentence in WA between 1st January 1985 and 31st December 1994, either on a community correction (non-custodial) order or in one of WA’s 13 prisons, and completed it before the censor date of 31st December 2008, thus excluding 29 offenders who either died while serving their index sentence or were still serving it on the censor date. A community comparison group of 1,877 non-sentenced people, henceforth referred to as ‘non-offenders’, was selected from the WA Electoral Roll by frequency matching to offenders of the same gender and age group at sentence commencement. Matching on race (i.e. Indigenous status) was not possible due to its unavailability on the Electoral Roll. Detailed selection criteria are described elsewhere [18]. For each non-offender, a hypothetical sentence start and end date was created corresponding to their matched offender and 13 people who either died before completing their hypothetical sentence or were still serving it on the censor date were removed, with 1,864 non-offenders included.
Data sources
The WA Department of Corrective Services provided correctional records for offenders. Offender and non-offender records were probabilistically linked [25] through the WA Data Linkage System to State-wide statutory health data collections, namely the Hospital Morbidity Data System for inpatient separations, the Mental Health Information System for public non-admitted (outpatient, ambulatory and community-based) psychiatric services and the Mortality Register for deaths [26].
MHS contact definition
A MHS contact was defined as any public or private psychiatric inpatient admission or any contact with public non-admitted MHSs. Diagnosed mental disorders were determined from the primary diagnosis in non-admitted records, or the primary or any of the 21 secondary diagnostic fields in inpatient records. Changes in diagnostic classification systems over time [27] were harmonised by transforming all psychiatric diagnostic codes to the International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM), effective in Australia from 1988 to July 1999 and corresponding to the timing of most study events.
Ascertainment of pre-sentence history
MHS contacts in the 1-year (0–1 year) and 5-year (0–5 year) pre-sentence periods were identified through psychiatric diagnoses (ICD-9-CM codes 290–319) during each period, and the latest psychiatric diagnosis established [18, 27–29]. For 1-year pre-sentence MHS use, seven diagnostic categories were created in hierarchical order of severity [16, 18, 29, 30]. These comprised non-affective psychotic disorders (295, 297, 298), affective psychotic disorders (296), personality disorders (301), substance use disorders (291, 292, 303, 304, 305), neurotic or depressive disorders (300, 311), adjustment disorders (308, 309) and a residual category comprising mental disorders of insufficient frequency or direct relevance to be analysed separately (290, 293, 294, 299, 302, 306, 307, 310, 312–319). If the last MHS contact had multiple psychiatric diagnoses, then the most serious condition according to the above hierarchy was chosen [16, 18, 27–30].
Thereafter, 5-year pre-sentence MHS use was defined through broad diagnostic categories including psychoses (295–298), substance use (291, 292, 303, 304, 305) and other mental disorders (290, 293, 294, 299–302, 306–319). In case of multiple psychiatric diagnoses on the last MHS contact, psychotic disorders took precedence over substance use disorders which were selected over other mental disorders [19, 29]. Both 1-year and 5-year history of attempted self-harm treatment was identified from the hospital discharge external cause of injury codes (E950.0–E959.9, E980.0–E980.6). Similarly, a 5-year pre-sentence history of physical illness was defined as any hospitalisation for physical illness (ICD-9-CM codes excluding 290–310; ICD-10-AM codes excluding F00–F99).
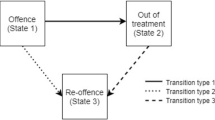
Ascertainment of post-sentence outcomes
MHS contacts within 5 years of sentence completion were identified. Follow-up was censored at 5 years or earlier if non-offenders died (n = 89) and for offenders, if they were re-sentenced (n = 185), died (n = 96) or at the follow-up censor date (n = 2), whichever came first. Five outcomes of interest were the time to first MHS contact after the end of the index sentence for (i) any mental disorder (290–319); (ii) psychotic disorder (295–298); (iii) substance use disorder (291, 292, 303, 304, 305); (iv) other mental disorder (290, 293, 294, 299–302, 306–319); and (v) attempted self-harm (E950.0–E959.9, E980.0–E980.6).
Geographic accessibility and social disadvantage
Social disadvantage was measured through the Index of Relative Socio-Economic Disadvantage (IRSD) [31], a summary measure of Socio-Economic Index for Areas (SEIFA) indicating relative disadvantage in terms of accessibility to education, employment and income [32]. IRSD quintiles (most disadvantaged to least disadvantaged) from the national Census year (1986, 1991 or 1996) closest to the year of index offence were used. Geographical accessibility was measured via the Accessibility and Remoteness Index of Australia (ARIA) scores from the 1996 Census, classified into highly accessible (ARIA scores: 0.00–1.84), accessible (1.84–5.80) and remote (5.80–12.00) categories [33]. Residential postcode at the time of index sentence was used to determine both measures.
Offence type
Offences were classified using the Australian and New Zealand Standard Offence Classification (ANZSOC) [34]. For a person concurrently convicted of multiple offences, the most serious crime was determined through the National Offence Index [35]. Offenders were thereafter categorised as violent (ANZSOC codes: 0111–0621) and non-violent (0711–1695).
Custodial setting and release type
Offenders were classified as being imprisoned or serving a non-custodial order. Those who had served a part of their sentence in both settings (n = 231, 12.3 %), mostly on being transferred to community corrections from prison, were included in the prisoner group [18]. Offenders could be released to freedom or conditionally (e.g. bail, parole and home detention) or re-sentenced.
Statistical analyses
Cohort characteristics and pre-sentence health service use were described using descriptive statistics for each gender–race demographic group, namely Indigenous females, Indigenous males, non-Indigenous females and non-Indigenous males, and collectively. Logistic regression models adjusted for gender, race and age compared 1-year pre-sentence MHS use across offender and non-offender groups. Kaplan–Meier estimates of the 5-year probability of post-sentence MHS outcomes were calculated for the full cohort and separately for offenders with (n = 392) and without (n = 1,461) a 5-year pre-sentence MHS contact, and also for the respective groups of non-offenders with (n = 124) and without (n = 1,740) a prior MHS contact.
Multivariable Cox proportional hazards regression models were used to identify the determinants for the two most common outcomes (any mental disorder and substance use disorder), separately for offenders with and without a 5-year pre-sentence MHS contact. Potential predictors examined included socio-demographic variables (gender, race, age at index sentence completion, ARIA and SEIFA), characteristics related to the index sentence (offence type, custodial setting and sentence duration) and pre-sentence health history (mental illness, physical illness and attempted self-harm). All statistical analyses were performed using SAS version 9.3.
Ethics
The Research and Evaluation Committee of the Department of Corrective Services (Reference Number: 2006/00276), and the Human Research and Ethics Committees of the Department of Health (Reference Number: 200623) and The University of Western Australia (Reference Number: RA/4/1/1347) approved this study.
Results
Description of offender cohort and non-offender comparison group
The offender cohort (n = 1,853) comprised 74.3 % non-Indigenous males, 17.1 % non-Indigenous females, 6.7 % Indigenous males and 1.9 % Indigenous females (Table 1). Most offenders were greatly disadvantaged socio-economically (48.2 %), lived in highly accessible areas (73.1 %), were non-violent (58.1 %), served community correction orders (62.9 %) and were unconditionally released to freedom (84.1 %). Indigenous males were the exception with 64.8 % violent offenders and 55.2 % imprisoned. Over 60 % of the cohort was aged 45–54 years both at sentence commencement (mean age = 53.2 years, SD = 7.1) and completion (mean age = 54.4 years, SD = 7.3). On average, the index sentence duration was 1.2 years (SD = 1.4) and the post-sentence follow-up period was 4.5 years (SD = 1.3), with 84.8 % offenders having a 5-year follow-up.
Pre-sentence MHS use
A 5-year pre-sentence MHS contact was present in 392 (21.2 %) offenders and 124 (6.7 %) non-offenders (Table 1). Substance use was the most commonly treated disorder for offenders and non-offenders in both periods. Overall, a 5-year pre-sentence history of attempted self-harm treatment was identified in 3.1 % offenders and 0.3 % non-offenders; and hospitalisation for physical illness in 46 % offenders and 42.2 % non-offenders.
A 1-year pre-sentence MHS contact existed for 221 (11.9 %) offenders and 43 (2.3 %) non-offenders ranging from 8.6 to 8.8 % in Indigenous female and male offenders to 11.9 to 13.6 % in non-Indigenous male and female offenders, respectively (Table 1). Due to the small numbers of Indigenous female offenders (n = 35), they were excluded from further gender–race comparisons. Substance use was the most commonly treated disorder in offenders (5.7 % overall, 6.4 % Indigenous males, 6.3 % non-Indigenous males and 2.9 % non-Indigenous females) and non-offenders (1.1 %) (Table 2). This was followed by neurotic/depressive disorders (1.7 % overall, 1.6 % Indigenous males, 1.0 % non-Indigenous males and 4.4 % non-Indigenous females) and non-offenders (0.5 %). Further, of those with a treated mental disorder, only 26 (1.4 %) offenders and 1 (0.05 %) non-offender had a comorbid substance use disorder recorded in the 1-year pre-sentence period.
Offenders versus non-offenders
Offenders were six times more likely (p < 0.0001) to have had at least one MHS contact for any mental disorder than non-offenders in the 1-year pre-sentence period, after adjusting for gender, race and age (Table 3). Adjusted Odds Ratios (ORs) were higher in offenders for all diagnostic categories, especially adjustment disorders (OR: 32.0, p < 0.001) and affective psychoses (OR: 15.3, p < 0.01), as well as for attempted self-harm (OR: 13.4, p < 0.001) than non-offenders.
Violent versus non-violent offenders
Violent and non-violent offenders had a similar 1-year pre-sentence MHS contact for most mental disorders, although hospitalisation for attempted self-harm was significantly higher in violent offenders (OR: 4.2, p < 0.01) than their non-violent peers (Table 3).
Custodial setting: prison versus community corrections
Prisoners were significantly less likely than those on community orders to have had a pre-sentence MHS contact for any mental disorder (OR: 0.6, p < 0.01) and for substance use disorders (OR = 0.5, p < 0.01), with no significant differences for other psychiatric diagnoses (Table 3).
Estimated 5-year likelihood of post-sentence MHS use
Overall, the 5-year probability of any post-sentence MHS contact was 23.0 % in offenders and 8.6 % in non-offenders (Table 4). It was lower (15.3 %) for offenders without and higher (52.2 %) for offenders with a pre-sentence MHS contact. The likelihood of post-sentence MHS use was highest for substance use disorders both in offenders with (37.4 % overall, 52.4 % in Indigenous males, 39.4 % in non-Indigenous males and 23.9 % in non-Indigenous females) and without (10.8 % overall, 16.5 % in Indigenous males, 11.3 % in non-Indigenous males and 6.4 % in non-Indigenous females) a pre-sentence MHS contact (Fig. 1). Similar patterns, but of a lower magnitude, were observed for all treated conditions in all demographics groups of non-offenders (Table 4).
Predictors of MHS use in 5-year post-sentence period
Among offenders with a pre-sentence MHS contact, the nature of past psychiatric diagnosis was a consistent predictor of post-sentence MHS use for any mental disorder and for substance use disorders (Table 5). Relative to offenders with a pre-sentence history of other disorders, those with a history of psychotic disorders were twice as likely to have a post-sentence MHS contact (Hazard Ratio (HR):2.1, p < 0.01) for any mental disorder, while those with substance use disorder treatment history were 2.7 times (p < 0.0001) more likely to have a post-sentence MHS contact for substance use disorder. Also, a 1-year pre-sentence MHS contact was 1.5 times (p < 0.05) more likely than an earlier (1–5 year) contact to lead to post-sentence MHS use.
Among offenders without pre-sentence MHS contact, a pre-sentence hospitalisation for attempted self-harm or physical illness, or being a male were the strongest predictors of post-sentence MHS use (Table 5). The HRs for post-sentence MHS contacts were 3.5 (p < 0.05) for any mental disorder and 6.6 (p < 0.001) for substance use disorder in offenders with a history of treated attempted self-harm, and 1.7 (p < 0.001) for any mental disorder and 1.5 (p < 0.05) for substance use disorder in those with a history of physical illness. Males were twice as likely (p < 0.05) to use MHSs for substance use disorders after sentence than females without a pre-sentence MHS contact.
No other socio-demographic variables were strong or consistent determinants of MHS outcome in offenders with an MHS use history (Table 5). However, within offenders without pre-sentence MHS contact, the most disadvantaged offenders had a greater likelihood of post-sentence MHS contact for any mental disorder (HR: 1.6, p < 0.05) and substance use disorder (HR: 1.8, p < 0.05) compared with the least disadvantaged offenders. None of the examined offence variables were strongly associated with either MHS outcome in offenders with or without a prior MHS contact. Although there was a decreasing trend in post-sentence MHS use by offenders serving longer sentences, with offenders serving <6 months being more likely (p < 0.05) to have a post-sentence MHS contact for any mental disorder if they had a pre-sentence MHS contact, however, most HRs did not reach statistical significance.
Discussion
Offenders over 45 years were six times (p < 0.0001) more likely to have used MHSs for any mental disorder than non-offenders (11.9 vs. 2.3 %) in the 1 year before their index sentence after adjusting for gender, race and age. They also had a greater likelihood of MHS contact within 5 years of sentence completion than non-offenders. These findings are consistent with results from our previous work on first-time offenders younger than 45 years who were eight times (p < 0.0001) more likely to have used MHSs for any mental disorder than their matched non-offenders (8.3 vs. 1.1 %) [18]. In fact, the relatively greater prevalence of gender- and race-adjusted 1-year pre-sentence MHS contacts in older offenders (11.9 %) than their younger (8.3 %) counterparts (OR: 1.5, 95 % CI: 1.3–1.7, p < 0.0001) is consistent with the high psychiatric morbidity reported in older offenders [4, 36], although general population studies report reducing prevalence of mental disorders with age [37, 38]. However, as over two-fifths of older (≥45 years) Australian prison entrants have a diagnosed mental illness [21], our findings highlight the limited MHS use by older offenders with mental disorders as also observed in the general population [39, 40].
Older non-custodial offenders had significantly greater likelihood of 1-year pre-sentence MHS contacts for any mental and substance use disorders than older prisoners which is in contrast to our findings in offenders younger than 45 years where a similar likelihood was observed [18]. Given that two-thirds of older offenders were serving non-custodial sentences, this emphasises the importance of routine screening for mental disorders in this group to facilitate on-going community-based management during sentence. However, although pre-sentence MHS contact prevalence differed by custodial setting, it was not a determinant of post-sentence MHS contact in multivariable analyses. This is surprising given that non-custodial offenders would likely have greater post-sentence MHS contacts relative to ex-prisoners due to their greater psychiatric morbidity at sentence commencement, better familiarity, access and absence of incarceration-related stigma [19, 41]. Further, reviews have recognized short-comings in MHS provision by Australian prison health services [42, 43]. Therefore, our findings may possibly be explained by the relatively better screening and treatment of mental and substance use disorders available for prisoners than for non-custodial offenders [44], which may have led to a better post-release uptake of MHSs by ex-prisoners as well.
While violent offenders are reported to have greater psychiatric hospitalisations than non-violent offenders [15], we found no difference in MHS use between these groups in either the pre- or post-sentence periods after adjusting for other variables, with one exception. Violent offenders were four times more likely than non-violent offenders to have attempted self-harm in the 1 year before their index sentence, possibly related to their underlying mental disorders, inherent aggression and impulsivity [45]. Co-occurrence of aggression against the self and others has been previously illustrated in violent psychiatric inpatients [46]. Indeed, research has identified an overlap in the factors predictive of the risk of violence towards others and the risk of self-harm [46–48]. Similar to our findings, these studies identified a history of self-harm to be strongly predictive of future violence to others [46–48] and highlighted the relevance of jointly managing both issues in forensic populations.
Almost half of the offenders with a pre-sentence MHS contact did not use MHSs within 5 years of sentence completion. Of those who did, offenders with psychotic disorders were considerably more likely to use MHSs than those with other disorders. This differential MHS use is similar to observations in the general Australian community [49, 50] and offenders younger than 45 years [19], and may indicate greater treatment-seeking behaviour, detection or availability of post-sentence MHSs for those with more serious underlying psychopathology [49]. It raises concerns regarding the adequacy of current throughcare and/or transitional care practices which link offenders with appropriate community-based services [51].
Exclusively in older offenders without a known MHS contact, pre-sentence hospitalisation for physical illness was a strong predictor of post-sentence MHS contact, similar to findings in adult offenders younger than 45 years [19]. General population studies have identified higher prevalence of mental disorders (28.0 vs. 17.6 %) [52] and a greater likelihood of using MHSs in people with chronic physical illnesses than in those without [53, 54]. Experiencing an adverse physical event also increases the likelihood of receiving mental healthcare and prescriptions by at least three times [55]. Thus, our findings are reasonably explained by the greater prevalence [52] and/or risk of developing mental disorders [56–58] in people with chronic physical health conditions possibly due to the common underlying risk factors and/or changes in self-image, lifestyle and social factors leading to mental health deterioration [55, 57].
The prevalence of mental illness in older offenders is known to differ by age sub-groups [4]. However, we found that although older age groups generally had greater adjusted probabilities of post-sentence MHS contact than those aged 45–49 years, most differences were not significant. This lack of significant differences in post-sentence MHS use, especially between those aged 45–49 and 50–54, is notable and validates our use of 45 years as the cut-off age. Therefore, while 50 years is an often used criterion for defining ‘older’ offenders [24], the use of 45 years may be a plausible option for identifying older offenders for future studies restricted by low power on using the 50-year cut-off age.
Interestingly, older males without a pre-sentence MHS contact were twice as likely as females to use MHSs after their sentence. This differs from findings in younger offenders [19] as well as the general population [37] where females were more likely to use MHSs. It is possibly explained by the association of serious mental disorders with higher MHS use [19, 37] considering that non-Indigenous male offenders (74 % of our cohort) had a greater baseline prevalence of psychotic disorders than non-Indigenous female offenders in this cohort. No other evaluated socio-demographic characteristics that were associated with post-sentence MHS use, although many older prisoners face socio-economic hardship related to employment difficulties, reduced family and social cohesion, or limited accommodation options [21], which can compromise their ability to cope after release.
Arrest data were unavailable for our study which used sentencing records to ascertain first-time older offenders. Nevertheless, prevalence estimates of MHS use as identified by whole-population studies on younger offenders who were either arrested [14] or sentenced [18] in WA over the same time period are similar (11.1 % arrested vs. 8.3 % sentenced). Importantly, previous research has identified that most offenders with a psychiatric treatment history were arrested before their first MHS contact [14, 59, 60] suggesting that this contact was likely initiated by the criminal justice system. In a forensic population, this raises the issue of malingering, i.e. presentation of exaggerated or false symptoms to gain benefit in a court of law, estimated to be present in one-fifth of all forensic assessments [61, 62]. Our data showed that of 221 older offenders with a 1-year pre-sentence MHS contact, only 39 offenders (17.7 %) did not have a prior (1–5 year) MHS contact, consistent with previous estimates of psychiatric malingering in this population [61, 62]. Most offenders (82.3 %) had both a recent (0–1 year) and remote (1–5 year) pre-sentence MHS contact history and were very likely to be genuine MHS users. Further, the finding of a 12-month pre-sentence MHS contact (versus a 1–5 year contact) being a strong determinant of post-sentence MHS use adds weight to the credibility of most pre-sentence contacts for psychiatric care in this cohort.
The whole-population design of our study using routinely collected administrative data overcame methodological limitations of previous survey-based studies including issues related to sample size limitations, loss to follow up and selection, recall and social desirability biases [63]. However, even with a whole-population cohort of offenders, few MHS contacts in some diagnostic categories and sub-groups of older offenders limited comparisons. Indeed, the low proportion of MHS contacts with comorbid substance use may be attributable to the under-treatment of substance use disorders [64] or their under-reporting on administrative databases [65]. Other limitations included a lack of information on contact with general practitioners or private psychologists or psychiatrists for mental healthcare, which were not captured in the available data collections. However, greater social disadvantage in offenders makes use of private secondary healthcare less likely than by the general population. While mentally ill people in the community commonly make contact with general practitioners [66], possibly leading to low use of secondary MHSs, no published study has investigated the engagement of offenders with general practitioners for mental healthcare. On the contrary, offenders are reported to commonly use emergency department services [67], data which were unavailable. In addition, no information about relative changes in offenders’ perceived psychological well-being [68] at sentence completion relative to commencement was available. Similarly, specific throughcare and/or transitional care services [51] from the criminal justice system to the community-based MHSs received by each offender were not known. Lastly, due to the inability to match on race, the proportion of Indigenous non-offenders received (1.3 % of comparison group) was markedly less than their representation in the cohort (8.6 %), although it was consistent with the census estimates (1.6 % of WA population ≥45 years) [69]. Future studies using alternative study designs and rich data may elicit the influence of personal, social, criminal justice and health system factors on offenders’ engagement with psychiatric services.
Conclusion
Pre-sentence MHS use by first-time older offenders is significantly greater than their counterparts in the general population as well as first-time younger offenders. The greater baseline prevalence of MHS use by older offenders sentenced to non-custodial orders than prisons warrants attention to the identification and continuing treatment of mental disorders upon sentence commencement for this large and often over-looked group. The high proportion of offenders discontinuing MHS use after sentence, especially those treated for non-psychotic disorders before sentence, is noteworthy. Among offenders with no prior MHS use, those with a pre-sentence hospitalisation for attempted self-harm and/or physical illness, those from the most disadvantaged areas and men were more likely to use MHSs after sentence. These findings underscore the need for better detection and treatment of mental disorders in these vulnerable groups through individually tailored age-sensitive correctional and community-based MHSs at all transition points to comprehensively address the health requirements of these special needs group of offenders. However, despite several contemporary correctional programmes aimed at improving post-release community integration of prisoners in WA [70], few are currently age sensitive.
References
Aday RH, Krabill JJ (2012) Older and geriatric offenders: critical issues for the 21st century. In: Gideon L (ed) Special needs offenders in correctional institutions. SAGE Publications Inc, London
Baidawi S, Turner S, Trotter C, Browning C, Collier P, O’Connor D, Sheehan R (2011) Older prisoners—a challenge for Australian corrections. Trends and Issues in Crime and Criminal Justice 426
Uzoaba J (1998) Managing older offenders: where do we stand?. Correctional Services of Canada, Ottawa
Kakoullis A, Le Mesurier N, Kingston P (2010) The mental health of older prisoners. Int Psychogeriatr 22(5):693–701. doi:10.1017/S1041610210000359
Grant A (1999) Elderly inmates: issues for Australia. Trends and Issues in Crime and Criminal Justice 115
Atabay T (2009) United Nations handbook on prisoners with special needs. United Nations Office on Drugs and Crime, New York
Fazel S, Hope T, O’Donnell I, Jacoby R (2001) Hidden psychiatric morbidity in elderly prisoners. Br J Psychiatry 179:535–539. doi:10.1192/bjp.179.6.535
Yorston GA, Taylor PJ (2006) Commentary: older offenders—no place to go? J Am Acad Psychiatry Law 34(3):333–337
Fazel S, Baillargeon J (2011) The health of prisoners. Lancet 377:956–965
Mitka M (2004) Aging prisoners stressing health care system. JAMA 292(4):423–424
Human Rights Watch (2012) Old behind bars: the aging prison population in the United States. Human Rights Watch, United States of America
Fazel S, Hope T, O’Donnell I, Jacoby R (2004) Unmet treatment needs of older prisoners: a primary care survey. Age Ageing 33(4):396–398
Sodhi-Berry N, Knuiman M, Alan J, Morgan V, Preen D (2014) Pre-sentence mental health service use predicts post-sentence mortality in a population cohort of first-time adult offenders. Soc Psychiatry Psychiatr Epidemiol. doi:10.1007/s00127-014-0919-8
Morgan V, Morgan F, Valuri G, Ferrante A, Castle D, Jablensky A (2012) A whole-of-population study of the prevalence and patterns of criminal offending in schizophrenia and other psychiatric disorders. Psychol Med First View 1–12. doi:10.1017/S0033291712002887
Timonen M, Miettunen J, Hakko H, Järvelin M, Veijola J, Kinnunen J, Räsänen P (2000) Psychiatric admissions at different levels of the national health care services and male criminality: the Northern Finland 1966 Birth Cohort study. Soc Psychiatry Psychiatr Epidemiol 35(5):198–201. doi:10.1007/s001270050228
Wallace C, Mullen P, Burgess P, Palmer S, Ruschena D, Browne C (1998) Serious criminal offending and mental disorder—case linkage study. Br J Psychiatry 172:477–484. doi:10.1192/bjp.172.6.477
Hobbs M, Krazlan K, Ridout S, Mai Q, Knuiman M, Chapman R (2006) Mortality and morbidity in prisoners after release from prison in Western Australia 1995–2003. Research and Public Policy Series No. 71. AIC, Canberra
Sodhi-Berry N, Preen DB, Alan J, Knuiman M, Morgan VA (2014) Pre-sentence mental health service use in adult offenders in Western Australia: baseline results from a longitudinal whole-population cohort study. Crim Behav Mental Health 24(3):204–221. doi:10.1002/cbm.1901
Sodhi-Berry N, Knuiman M, Preen DB, Alan J, Morgan VA (2014) Predictors of post-sentence mental health service use in a population cohort of first-time adult offenders in Western Australia. Crim Behav Mental Health Early View. doi:10.1002/cbm.1927
Hartwell S, Deng X, Fisher W, Siegfriedt J, Roy-Bujnowski K, Johnson C, Fulwiler C (2013) Predictors of accessing substance abuse services among individuals with mental disorders released from correctional custody. J Dual Diagn 9(1):11–22. doi:10.1080/15504263.2012.749449
Australian Institute of Health and Welfare (2013) The health of Australia’s prisoners. AIHW, Canberra
Yorston G (1999) Aged and dangerous—old-age forensic psychiatry. Br J Psychiatry 174:193–195. doi:10.1192/bjp.174.3.193
Australian Institute of Health and Welfare, Australian Bureau of Statistics (2008) The Health and Welfare of Australia’s Aboriginal and Torres Strait Islander Peoples. Catalogue No. AIHW 21. AIHW & ABS, Commonwealth of Australia
Loeb SJ, AbuDagga A (2006) Health-related research on older inmates: an integrative review. Res Nurs Health 29(6):556–565. doi:10.1002/nur.20177
Kelman C, Bass A, Holman C (2002) Research use of linked health data—a best practice protocol. Aust N Z J Public Health 26(3):251–255. doi:10.1111/j.1467-842X.2002.tb00682.x
Holman C, Bass J, Rouse I, Hobbs M (1999) Population-based linkage of health records in Western Australia: development of a health services research linked database. Aust N Z J Public Health 23(5):453–459. doi:10.1111/j.1467-842X.1999.tb01297.x
Morgan V, Jablensky A (2010) From inventory to benchmark: quality of psychiatric case registers in research. Br J Psychiatry 197(1):8–10. doi:10.1192/bjp.bp.109.076588
Sara G, Luo L, Carr VJ, Raudino A, Green MJ, Laurens KR, Dean K, Cohen M, Burgess P, Morgan VA (2014) Comparing algorithms for deriving psychosis diagnoses from longitudinal administrative clinical records. Soc Psychiatry Psychiatr Epidemiol. doi:10.1007/s00127-014-0881-5
Lawrence D, Holman C, Jablensky A (2001) Duty to care: preventable physical illness in people with mental illness. The University of Western Australia, Perth
Ruschena D, Mullen P, Burgess P, Cordner S, Barry-Walsh J, Drummer O, Palmer S, Browne C, Wallace C (1998) Sudden death in psychiatric patients. Br J Psychiatry 172:331–336. doi:10.1192/bjp.172.4.331
Australian Bureau of Statistics (2006) Census of population and housing: Socio-Economic Indexes for Areas (SEIFA), Australia—data only, 2006. Catalogue No. 2033.0.55.001. ABS, Canberra
Australian Institute of Health and Welfare (2012) Socio-Economic Indexes for Areas (SEIFA) cluster. Metadata Online Registry (METeOR), AIHW, Canberra
Department of Health and Aged Care (2001) Measuring Remoteness: Accessibility/Remoteness Index of Australia (ARIA). Occasional Paper New Series No. 14. Department of Health and Aged Care, Canberra
Australian Bureau of Statistics (1997) Australian Standard Offence Classification. Catalogue No. 1234.0. ABS, Canberra
Australian Bureau of Statistics (2003) Appendix 5: National Offence Index—Technical Paper. In: Criminal Courts, Australia, 2001-02. Catalogue No. 4513.0. ABS, Commonwealth of Australia, Canberra
Fazel S, Grann M (2002) Older criminals: a descriptive study of psychiatrically examined offenders in Sweden. Int J Geriatr Psychiatry 17(10):907–913. doi:10.1002/gps.715
Australian Bureau of Statistics (2007) National Survey of Mental Health and Wellbeing: Summary of Results. Catalogue No. 4326.0. vol 4326.0. ABS, Canberra
Nagle C (1999) Mental health and well-being: profile of adults Western Australia 1997–98. ABS, Canberra
Andrews G, Hall W, Teesson M, Scott H (1999) The Mental Health of Australians. Mental Health Branch, Commonwealth Department of Health and Aged Care, Canberra
Thornicroft G (2007) Most people with mental illness are not treated. Lancet 370(9590):807–808. doi:10.1016/S0140-6736(07)61392-0
Owens G, Rogers S, Whitesell A (2011) Use of mental health services and barriers to care for individuals on probation or parole. J Offender Rehabil 50(1):37–47
Human Rights Law Resource Centre (2008) Australia’s compliance with the convention against torture. Report to the United Nations Committee against Torture. Human Rights Law Resource Centre, Melbourne
Burdekin B (1993) Human Rights and Mental Illness: Report of the National Inquiry into the Human Rights of People with Mental Illness. Australian Human Rights Commission
Cropsey K, Binswanger I, Clark CB, Taxman F (2012) The unmet medical needs of correctional populations in the United States. J Natl Med Assoc 104(11–12):487–492
Gvion Y, Apter A (2011) Aggression, impulsivity, and suicide behavior: a review of the literature. Arch Suicide Res 15(2):93–112
Hillbrand M (1995) Aggression against self and aggression against others in violent psychiatric patients. J Consult Clin Psychol 63(4):668–671
Fagan J, Papaconstantinou A, Ijas A, Lynch A, O’Neill H, Kennedy H (2009) The suicide risk assessment and management manual (S-RAMM) validation study II. Ir J Psychol Med 26(3):107–113
Abidin Z, Davoren M, Naughton L, Gibbons O, Nulty A, Kennedy H (2013) Susceptibility (risk and protective) factors of in-patient violence and self-harm: prospective study of structured professional judgement instruments START and SAPROF, DUNDRUM-3 and DUNDRUM-4 in forensic mental health services. BMC Psychiatry 13:197. doi:10.1186/1471-244X-13-197
Burgess PM, Pirkis JE, Slade TN, Johnston AK, Meadows GN, Gunn JM (2009) Service use for mental health problems: findings from the 2007 National Survey of Mental Health and Wellbeing. Aust N Z J Psychiatry 43(7):615–623. doi:10.1080/00048670902970858
Short T, Thomas S, Luebbers S, Ogloff JR, Mullen P (2010) Utilization of public mental health services in a random community sample. Aust N Z J Psychiatry 44(5):475–481
Borzycki M, Baldry E (2003) Promoting integration: the provision of prisoner post-release services. Trends and Issues in Crime and Criminal Justice 262:1–6
Slade T, Johnston A, Teeson M, Whiteford H, Burgess P, Pirkis J, Saw S (2009) The Mental Health of Australians 2. Report on the 2007 National Survey of Mental Health and Wellbeing. Department of Health and Ageing, Canberra
Perkins D, Fuller J, Kelley B, Lewin T, Fitzgerald M, Coleman C, Inder K, Allan J, Arya D, Roberts R, Buss R (2013) Factors associated with reported service use for mental health problems by residents of rural and remote communities: cross-sectional findings from a baseline survey. BMC Health Serv Res 13:157–170
Rabinowitz J, Gross R, Feldman D (1999) Correlates of a perceived need for mental health assistance and differences between those who do and do not seek help. Soc Psychiatry Psychiatr Epidemiol 34(3):141–146
Yoon J, Bernell SL (2012) The role of adverse physical health events on the utilization of mental health services. Health Serv Res 48(1):175–194. doi:10.1111/j.1475-6773.2012.01442.x
National Centre for Chronic Disease Prevention and Health Promotion (2012) Mental Health and Chronic Diseases. National Centre for Chronic Disease Prevention and Health Promotion. http://www.cdc.gov/nationalhealthyworksite/docs/issue-brief-no-2-mental-health-and-chronic-disease.pdf. Accessed 25 Oct 2014
Clarke D, Currie K (2009) Depression, anxiety and their relationship with chronic diseases: a review of the epidemiology, risk and treatment evidence. Med J Aust 190:S54–S60
Wilhelm K, Mitchell P, Slade T, Brownhill S, Andrews G (2003) Prevalence and correlates of DSM-IV major depression in an Australian national survey. J Affect Disord 75:155–162
Large M, Nielssen O (2011) Violence in first-episode psychosis: a systematic review and meta-analysis. Schizophr Res 125(2):209–220
Wallace C, Mullen P, Burgess P (2004) Criminal offending in schizophrenia over a 25-year period marked by deinstitutionalization and increasing prevalence of comorbid substance use disorders. Am J Psychiatry 161(4):716–727. doi:10.1176/appi.ajp.161.4.716
Rogers R, Sewell K, Morey L, Ustad K (1996) Detection of feigned mental disorders on the Personality Assessment Inventory: a discriminant analysis. J Personal Assess 67:629–640
McDermott BE, Dualan IV, Scott CL (2013) Malingering in the correctional system: does incentive affect prevalence? Int J Law Psychiatry 36(3–4):287–292. doi:10.1016/j.ijlp.2013.04.013
Drapeau A, Boyer R, Diallo F (2011) Discrepancies between survey and administrative data on the use of mental health services in the general population: findings from a study conducted in Quebec. BMC Public Health 11:837. doi:10.1186/1471-2458-11-837
Ogloff JRP, Lemphers A, Dwyer C (2004) Dual diagnosis in an Australian forensic psychiatric hospital: prevalence and implications for services. Behav Sci Law 22(4):543–562. doi:10.1002/bsl.604
Preen DB, Holman CDJ, Lawrence DM, Baynham NJ, Semmens JB (2004) Hospital chart review provided more accurate comorbidity information than data from a general practitioner survey or an administrative database. J Clin Epidemiol 57(12):1295–1304. doi:10.1016/j.jclinepi.2004.03.016
Mai Q, Holman CD, Sanfilippo FM, Emery JD, Stewart LM (2010) Do users of mental health services lack access to general practitioner services? Med J Aust 192(9):501–506
Frank J, Andrews C, Green T, Samuels A, Trinh T, Friedmann P (2013) Emergency department utilization among recently released prisoners: a retrospective cohort study. BMC Emerg Med 13:16
Andersen RM (1995) Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav 36(1):1–10. doi:10.2307/2137284
Australian Bureau of Statistics (2013) Estimates of Aboriginal and Torres Strait Islander Australians, June 2011. Catalogue No. 3238.0.55.001. Australian Bureau of Statistics, Canberra
Outcare (2010) Making our prisons work. An inquiry into the efficiency and effectiveness of prisoner education, training and employment strategies. Outcare Incorporated. Submission to the Parliament of Western Australia. http://outcare.com.au/wp-content/uploads/2011/10/Making-Our-Prisons-Work-5-March-2010.-Outcare-Parliamentary-submission.pdf. Accessed 5 Nov 2012
Acknowledgments
This study was supported by a NHMRC Grant (No. 403909) and the first author was supported by the UWA-SIRF scholarship. We thank the Data Linkage Branch for linkage and client support services aspects of data provision. We also thank the WA Department of Corrective Services, the custodians of the Inpatient and Mental Health Data Collections of the WA Department of Health and the WA Registry of Births, Deaths and Marriages for the provision of service data.
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Disclaimer
The results and discussions of this study are not an expression of the views or policies of the Department of Corrective Services, the Department of Health or the Department of the Attorney General.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sodhi-Berry, N., Knuiman, M., Alan, J. et al. Pre- and post-sentence mental health service use by a population cohort of older offenders (≥45 years) in Western Australia. Soc Psychiatry Psychiatr Epidemiol 50, 1097–1110 (2015). https://doi.org/10.1007/s00127-015-1008-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-015-1008-3